Chapter: Medical Surgical Nursing: Management of Patients With Musculoskeletal Trauma
Pelvis - Fracture
PELVIS
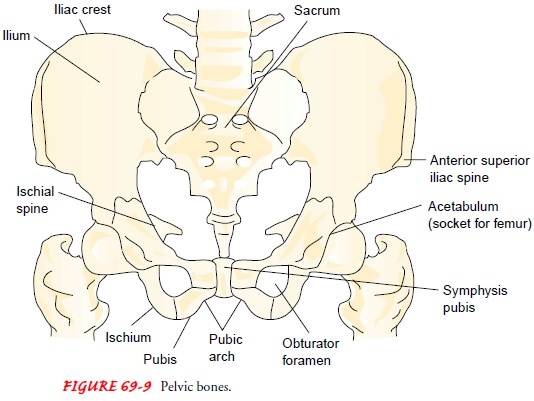
The sacrum, ilium,
pubis, and ischium bones form the pelvic bone, a fused, stable, bony ring in
adults (Fig. 69-9). Falls, motor vehicle crashes, and crush injuries can cause
pelvic fractures. Pel-vic fractures are serious because at least two thirds of
affected patients have significant and multiple injuries. Management of severe,
life-threatening pelvic fractures is coordinated with the trauma team.
Hemorrhage and thoracic, intra-abdominal, and cranial injuries have priority
over treatment of fractures. There is a high mortality rate associated with
pelvic fractures, related to hemorrhage, pulmonary complications, fat emboli,
intravascular coagulation, thromboembolic complications, and infection.
Pelvic fracture symptoms
include ecchymosis; tenderness over the symphysis pubis, anterior iliac spines,
iliac crest, sacrum, or coccyx; local swelling; numbness or tingling of pubis,
genitals, and proximal thighs; and inability to bear weight without
dis-comfort. Computed tomography of the pelvis helps to determinethe extent of
injury by demonstrating sacroiliac joint disruption, soft tissue trauma, pelvic
hematoma, and fractures. Neurovascular assessment of the lower extremities is
completed to detect injury to pelvic blood vessels and nerves.
Hemorrhage and shock are
two of the most serious consequen-ces that may occur. Bleeding arises from the
cancellous surfaces of the fracture fragments, from laceration of veins and
arteries by bone fragments, and possibly from a torn iliac artery. The
peripheral pulses of both lower extremities are palpated; absence of pulses may
indicate a torn iliac artery or one of its branches. Peritoneal lavage may be
performed to detect intra-abdominal hemorrhage. The patient is handled gently
to minimize further bleeding and shock.
The nurse assesses for injuries to the bladder, rectum,
intes-tines, other abdominal organs, and pelvic vessels and nerves. To assess
for urinary tract injury, the patient’s urine is examined for blood. A voiding
cystourethrogram and an intravenous urogram may be performed. Laceration of the
urethra is suspected in males with anterior fracture of the pelvis and blood at
the urethral me-atus. (Females rarely experience a lacerated urethra.) A
catheter should not be inserted until the status of the urethra is known.
Abdominal pain and signs of peritonitis suggest injury to the in-testines or
abdominal bleeding. Paralytic ileus may accompany pelvic fractures.
Numerous classification
systems have been used to describe pelvic fractures in relation to anatomy,
stability, and mechanism of injury. Some fractures of the pelvis do not disrupt
the pelvic ring; others disrupt the ring, which may be rotationally or
verti-cally unstable. The severity of pelvic fractures varies. Long-term
complications of pelvic fractures include malunion, nonunion, residual gait
disturbances, and back pain from ligament injury.
Stable Pelvic Fractures
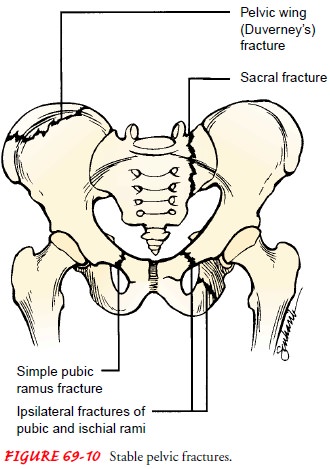
Stable fractures of the
pelvis (Fig. 69-10) include fracture of a single pubic or ischial ramus,
fracture of ipsilateral pubic and ischial rami, fracture of the pelvic wing of
ilium (ie, Duverney’s fracture), and fracture of the sacrum or coccyx. Also, if
injury results in only a slight widening of the pubic symphysis or the anterior
sacroiliac joint and the pelvic ligaments are intact, the disrupted pubic sym-physis
is likely to heal spontaneously with conservative manage-ment. Most fractures
of the pelvis heal rapidly because the pelvic bones are mostly cancellous bone,
which has a rich blood supply.
Stable pelvic fractures are treated with a few days of
bed rest and symptom management until the pain and discomfort are con-trolled.
The patient on bed rest is at risk for complications from immobility, including
constipation, venous stasis, and pulmonary complications. Fluids, dietary
fiber, ankle and leg exercises, elastic compression stockings to aid venous
return, log rolling, coughing and deep breathing, and skin care reduce the risk
for complica-tions and increase the patient’s comfort. The patient with a
frac-tured sacrum is at risk for paralytic ileus, and bowel sounds should be
monitored.
The patient with fracture of the coccyx experiences pain
on sitting and with defecation. Sitz baths may be prescribed to re-lieve pain,
and stool softeners may be given to prevent the need to strain on defecation.
As pain resolves, activity is gradually resumed with the use of ambulatory aids
(eg, crutches, walker) for protected weight bearing. Early mobilization reduces
problems related to immobility.
Unstable Pelvic Fractures
Unstable fractures of
the pelvis (Fig. 69-11) may result in rotational instability (eg, the open book
type, in which a separation occurs at the symphysis pubis with some sacral
ligament disruption), vertical instability (eg, the vertical shear type, with
superior–inferior dis-placement), or a combination of both. Lateral or
anterior–posterior compression of the pelvis produces rotationally unstable
pelvic frac-tures. Vertically unstable pelvic fractures occur when force is exerted
on the pelvis vertically, as when the person falls from a height onto extended
legs or is struck from above by a falling object. Vertical shear pelvic
fractures involve the anterior and posterior pelvic ring with vertical
displacement, usually through the sacroiliac joint. There is generally complete
disruption of the posterior sacroiliac, sacrospinous, and sacrotuberous
ligaments. Vertical displacement of the hemipelvis is usually evident.
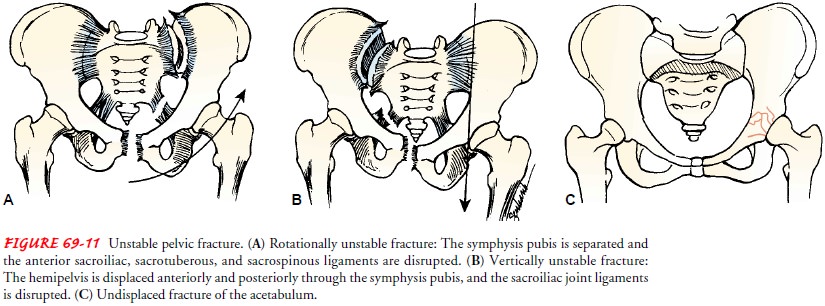
Treatment of unstable pelvic fractures generally involves
ex-ternal fixation or open reduction and internal fixation. This pro-motes
hemostasis, hemodynamic stability, comfort, and early mobilization.
Acetabulum
Fractures of the
acetabulum are seen after motor vehicle crashes in which the femur is jammed
into the dashboard. Treatment depends on the pattern of fracture. Stable,
nondisplaced fractures and frac-tures that involve minimal articular weight
bearing may be managed with traction and protective (toe touch) weight bearing.
Displaced and unstable acetabular fractures are treated with open reduction,
joint débridement, and internal fixation or arthroplasty. Internal fixation
permits early non–weight-bearing ambulation and ROM exercise. Complications
seen with acetabular fractures include nerve palsy, heterotopic ossification,
and posttraumatic arthritis.
Related Topics