Chapter: Human Nervous System and Sensory Organs : Spinal Cord and Spinal Nerves
Infraclavicular Part - Peripheral Nerves
Infraclavicular Part
Three main trunks of the anterior branches, the superior, middle, and inferior trunks ofthe brachial plexus, give rise to three cords,the lateral, middle, and posterior fascicles; they are named according to their position relative to the axillary artery.
Lateral Fascicle
The lateral fascicle gives rise to the musculocutaneous nerve and the median nerve.
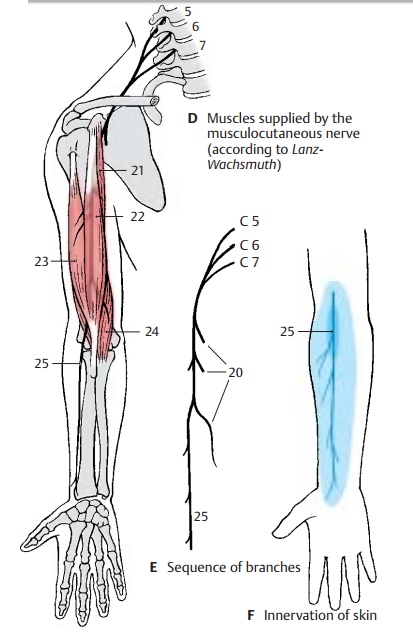
Musculocutaneous nerve (C5 – C7) (D – F).
The nerve passes through the coraco-brachial muscle and runs between the bi-ceps muscle and the brachial muscle down to the elbow. It gives off branches (E20) to the flexor muscles of the upper arm, namely, to the coracobrachial muscle (D21), to the short head (D22) and long head (D23) of the biceps muscle of the arm, and to the brachial muscle (D24).
The sensory fibers of the nerves come to the surface through the fascia at the elbow and supply the skin in the lateral region of the forearm as lateral cutaneous nerve of the fore-arm (D – F25). Injury to this nerve causesloss of sensibility in a small zone of the elbow; diminished sensibility extends to the middle of the forearm.
Innervation of the skin (F).Autonomiczone (dark blue) and maximum zone (light blue).
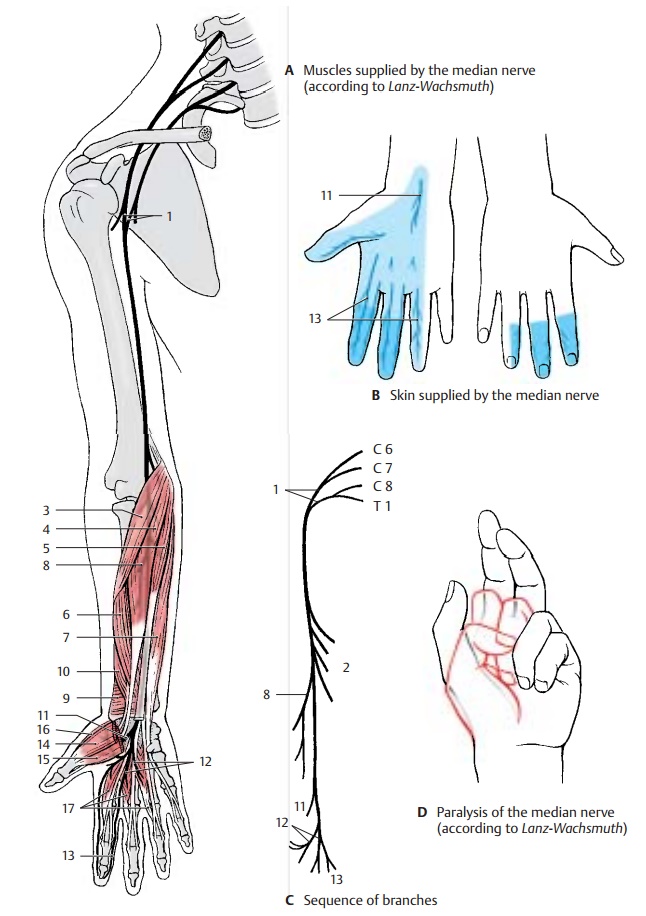
Median nerve (C6 – T1). Parts of the lateraland medial fascicles form the median loop (AC1) at the anterior surface of the axillary artery and join to form the median nerve.
The nerve extends in the medial bicipital sulcus along the surface of the brachial artery to the elbow, where it passes be-tween the two heads of the round pronator muscle to the forearm. It runs between the superficial flexor muscle of the fingers and the deep flexor muscle of the fingers to the wrist. Prior to its passage through the carpaltunnel, it lies superficially between the ten-dons of the radial flexor muscle of the wrist and the long palmar muscle. In the carpal tunnel, it ramifies into its terminal branches.
The muscular branches (C2) of the nerve supply the pronator muscles and most of the flexor muscles of the forearm, namely, theround pronator muscle (A3), the radial flexor muscle of the wrist (A4), the long pal-mar muscle (A5), and the superficial flexor muscle of the fingers with radial head (A6) and humeroulnar head (A7). In the elbow, the anterior interosseous nerve of the forearm (AC8) branches off and runs along the inter-osseous membrane to the quadrate prona-tor muscle (A9). It gives off branches to the long flexor muscle of the thumb (A10) and to the radial part of the deep flexor muscle of the fingers.
In the lower third of the forearm, the sensory palmar branch of the median nerve (A – C11) branches off to the skin of the ball of the thumb (thenar eminence), to the radial side of the wrist, and to the palm.
After passing through the carpal tunnel, the median nerve divides into three branches: the common palmar digital nerves I – III (A – C12), each of which bifurcates at the level of the metacarpophalangeal joints into two proper palmar digital nerves (A – C13). From the first common palmar digital nerve, a branch extends to the thenar eminence (short abductor muscle of thumb [A14], su-perficial head of the short flexor muscle of thumb [A15 ], and opposing muscle of thumb [A16]). The common palmar digitalnerves supply the lumbrical muscles I – III(A17). They run to the interdigits and bifur-cate in such a way that each pair of properpalmar digital nerves provides sensoryfibers to the lateral aspects of an interdigit. Thus, the first pair of nerves supplies the ulnar side of the thumb and the radial side of the index finger, the second pair supplies the ulnar side of the index finger and the radial side of the middle finger, and the third pair supplies the ulnar side of the middle finger and the radial side of the ring finger. The area innervated by the proper palmar digital nerves on the posterior side includes the end phalanx of the thumb as well as the distal and middle phalanges of the fingers (B).
The median nerve gives off branches to the periosteum, elbow joint, radiocarpal joint, and mediocarpal joint. At the level of the wrist, there is normally an anastomosis with the ulnar nerve.
Clinical Note: After injury to the nerve, pro-nation of the forearm is no longer possible and flexion is severely restricted. As to the hand, the thumb, index finger and middle finger can no longer be flexed at the end and middle phalanges, resulting in a characteristic feature of median pa-ralysis, the so-called hand of oath (D). On passing the carpal tunnel, the nerve can be injured by pressure in older persons (carpal tunnel syn-drome).
Innervation of the skin (B).Autonomiczone (dark blue) and maximum zone (light blue).
Medial Fascicle (A – D)
Ulnar nerve (C8 – T1). Initially, the ulnarnerve runs in the upper arm in the medial bicipital sulcus without giving off any branches.
On the ulnar side of the upper arm, the nerve runs down behind the medial inter-muscular septum, being covered by the me-dial head of the triceps muscle. It crosses the elbow joint on the extensor side in a bony groove, the sulcus for the ulnar nerve, at the medial epicondyle of the humerus. Here, the nerve can be palpated, and the pressure causes an electrifying pain radiat-ing into the ulnar side of the hand. The nerve then passes between the two heads of the ulnar flexor muscle of the wrist to the flexor side of the forearm and runs beneath this muscle down to the wrist. It does not pass through the carpal tunnel but extends over the flexor retinaculum to the palm of the hand, where it divides into a superficialbranch and a deep branch.
In the forearm, the nerve gives off branches (C1) to the ulnar flexor muscle of the wrist (A2) and to the ulnar half of the deep flexor muscle of the fingers (A3). A sensory branch, the dorsal branch of the ulnar nerve (BC4), branches off in the middle of the fore-arm and runs to the ulnar side of the back of the hand where it supplies the skin. As for the rest of the back of the hand, its area of innervation overlaps with that of the radial nerve. Another sensory branch, the palmarbranch of the ulnar nerve (BC5), branches offin the distal third of the forearm. It extends to the palm and supplies the skin of the hy-pothenar eminence.
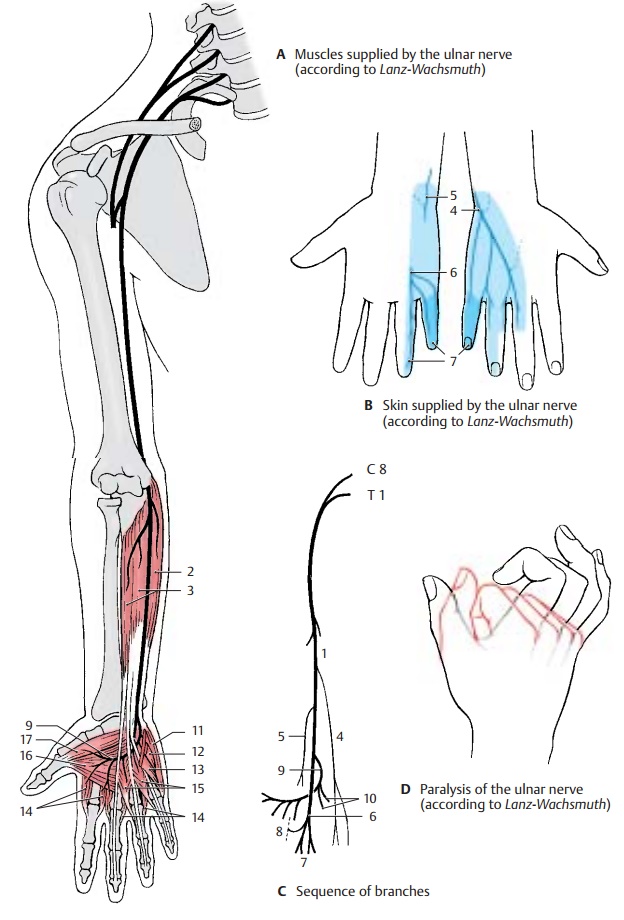
The superficial branch runs as common palmardigital nerve IV (BC6) toward the interdigitalspace between ring finger and little finger and divides into the proper palmar digitalnerves (BC7), which supply sensory fibers tothe volar aspects of the little finger and the ulnar side of the ring finger and reach to the distal phalanges on the extensor side of both fingers. There is a connection to a branch of the median nerve, called the com-municating branch of the median nerve with the ulnar nerve (C8).
The deep branch (AC9) sinks into the depth of the palm and curves toward the thenar emi-nence. It gives off branches for all muscles of the hypothenar eminence (C10) (abductor muscle of fifth finger [A11], short flexor muscle of fifth finger [A12], opposing muscle of fifth finger [A13]), for all dorsal and palmar interosseous muscles (A14), for the lumbrical muscles III and IV (A15), and finally, at the thenar eminence, for the ab-ductor muscle of thumb (A16) and the deep head of the short flexor muscle of thumb (A17).
Clinical Note: Injury to the ulnar nerve causesthe formation of a so-called clawhand (D), where the fingers are extended in the metacarpo-phalangeal joints but flexed in the proximal and distal interphalangeal joints. This characteristic posture of the fingers is caused by paralysis of the interosseous muscles and lumbrical muscles, which flex the phalanges in the metacarpo-phalangeal joints but extend them in the proxi-mal and distal interphalangeal joints. Failure of the flexor muscles causes the fingers to remain in this posture due to the now predominant exten-sor muscles. Since the little finger and the adduc-tors of the thumb are paralyzed, thumb and little finger can no longer touch each other.
Innervation of the skin (B).Autonomiczone (dark blue) and maximum zone (light blue).
Medial Fascicle (continued) (A – C)
In addition to the ulnar nerve, the medial fascicle gives rise to the medial cutaneousnerve of the arm and the medial cutaneous nerve of the forearm; both are exclusivelysensory nerves supplying the skin on the median side of the arm.
Medial cutaneous nerve of the arm (C8 –T1) (A, B). The nerve approaches the ante-rior surface of the upper arm below the axil-lary fossa. Here it ramifies and supplies the skin of the medial aspect between axilla and elbow joint. It reaches to the flexor side with its anterior branches and to the extensor side of the upper arm with its posterior branches. Frequently, there are anasto-moses to the intercostobrachial nerve.
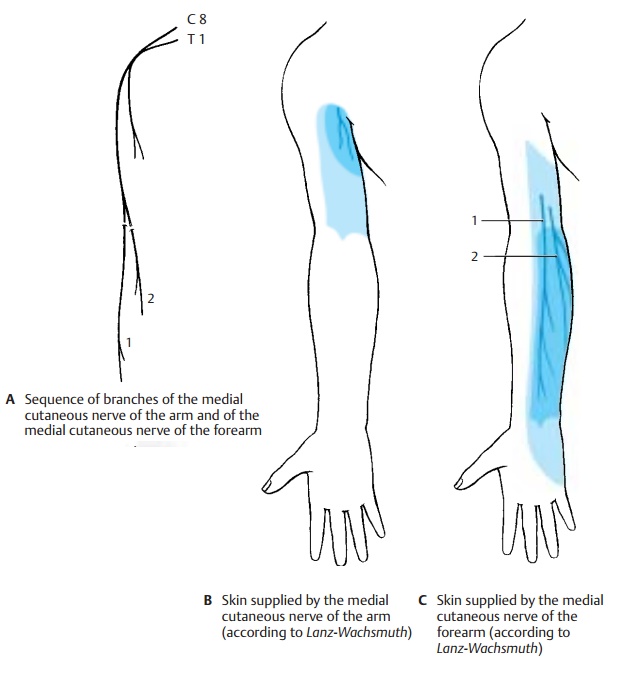
Medial cutaneous nerve of the forearm
(C8 – T1) (A, C). The nerve runs below the fascia on the ulnar side of the forearm and passes in the lower third through the fascia with two branches, the anterior branch(AC1) and the ulnar branch (AC2). The anterior branch supplies the medial flexor side of the forearm almost up to the midline, and the ulnar branch supplies the upper region of the medial extensor side almost up to the midline. The area innervated by the medial cutaneous nerve of the forearm extends slightly to the upper arm and to the hand.
Posterior Fascicle (D, F)
The posterior fascicle gives rise to the axil-lary nerve and the radial nerve.
Axillary nerve (C5 – C6).This runs deep in-side the axilla and across the capsule of the shoulder joint around the surgical neck on the back of the humerus. It passes through the lateral axillary gap and extends beneath the deltoid muscle to the anterior margin of the latter.
Before the nerve trunk passes through the lateral axillary gap, it gives off a motor branch (DF3) to the lesser teres muscle (D4), which also passes through the lateral axil-lary gap. At the same level, the superiorlateral cutaneous nerve of the arm (D–F5)branches off and reaches the skin at the pos-terior margin of the deltoid muscle, where it supplies the skin of the lateral aspects of shoulder and upper arm. From the nerve trunk extending beneath the deltoid muscle to the front, numerous branches (D6) to the deltoid muscle (D7) branch off and supply its various parts.
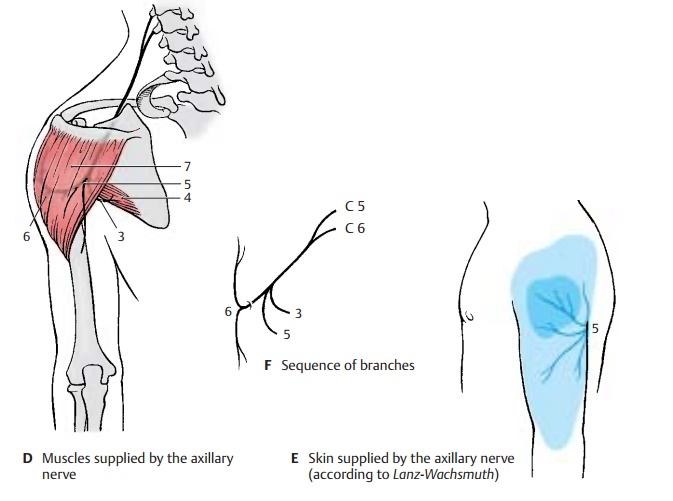
Clinical Note: As a result of its location on thecapsule of the shoulder joint, the nerve can be in-jured by dislocation of the humerus or by humeral neck fracture. This causes anesthesia in the skin area over the deltoid muscle.
Innervation of the skin (B, C, E).Auto-nomic zone (dark blue) and maximum zone (light blue).
Radial nerve (C5 – C8) (A – C). The main nerve of the posterior cord supplies the ex- tensor muscles of upper arm and forearm.
The nerve trunk extends from the axilla into the proximal third of the medial bicipital sulcus and then spirals around the dorsal surface of the humerus, to which it is directly apposed in the sulcus of the radial nerve. In the distal third of the upper arm, it passes to the flexor side between brachial muscle and brachioradial muscle. In the sul- cus of the radial nerve, the nerve can easily be injured by pressure or by bone fractures because of its proximity to the bone. The nerve crosses the elbow joint on the flexor side and divides at the level of the head of radius into two terminal branches, the su-perficial branch and the deep branch. The su- perficial branch continues in the forearm on the medial surface of the brachioradial muscle and then runs in the lower third be- tween brachioradial muscle and radius to the extensor side in order to reach the back of the hand. The deep branch obliquely penetrates the supinator muscle, gives off numerous muscular branches, and extends as the thin posterior interosseous nerve of the forearm to the wrist.
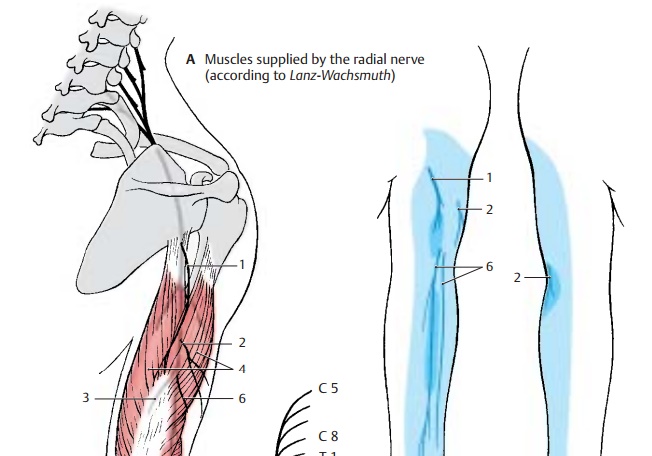
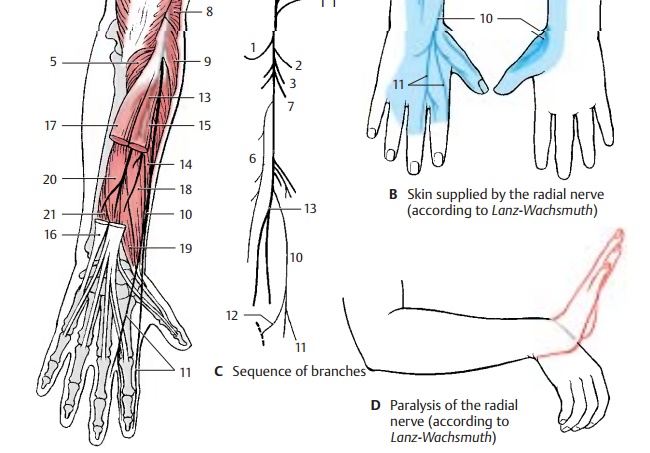
For the upper arm, the radial nerve gives off the posterior cutaneous nerve of the arm (A – C1), which supplies a skin area on the extensor side of the upper arm with sensory fibers, and the inferior lateral cutaneous nerve of the arm (A – C2). In the middle third of the upper arm, it gives off muscular branches (AC3) for the long head, the lateral head, andthe medial head of the triceps muscle (A4). The branch for the medial head gives off also the branch for the anconeus muscle (A5).
The posterior cutaneous nerve of the forearm(A – C6) branches off in the region of thethen ramifies into its two major branches in the forearm. At the back of the hand, the superficial branch (A – C10) gives off the dorsal digital nerves (A – C11); they supply sensory fibers to the radial back of the hand, the extensor side of the thumb, the proximal phalanges of index and middle fingers, and the radial half of the extensor side of the ring finger. The ulnar communicating branch of the radial nerve connects with the ulnar nerve (C12).
The deep branch (AC13) gives off muscular branches to the short radial extensor muscle of the wrist (A14) and to the supinator muscle, while passing through the supina- tor muscle. Thereafter, it gives off motor branches to the hand extensor muscles, namely, to the common extensor muscle of the fingers (A15), the extensor muscle of the little finger (A16), the ulnar extensor muscleof the wrist (A17), the long abductor muscle of the thumb (A18), and the short extensor muscle of the thumb (A19). Finally, the ter- minal branch of the deep branch, the poste- rior interosseous nerve, gives off branches to the long extensor muscle of the thumb (A20) and to the extensor muscle of the index finger (A21).
The nerve sends sensory branches to the shoulder joint and wrist.
Clinical Note: Injury to the main nerve trunk in the area of the upper arm results in paralysis of the extensor muscles. This mainly affects the hand, leading to the so-called wristdrop (D) characteristic for radial paralysis: extension is possible neither in the wrist nor in the fingers, thus making the hand drop down limply.
Innervation of the skin (B).Autonomic zone (dark blue) and maximum zone (light blue).
Related Topics