Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Endocrine Disorders
Hypothyroidism - Management of Patients With Thyroid Disorders
HYPOTHYROIDISM
Hypothyroidism results from suboptimal levels of thyroid hor-mone. Thyroid deficiency can affect all body functions and can range from mild, subclinical forms to myxedema, an advanced form. The most common cause of hypothyroidism in adults is autoimmune thyroiditis (Hashimoto’s disease), in which the immune system attacks the thyroid gland.
Symptoms of hyper thyroidism
may later be followed by those of hypothyroidism and myxedema. Hypothyroidism
also commonly occurs in patients with previous hyperthyroidism who have been
treated with radio-iodine or antithyroid medications or who have had surgery.
It oc-curs most frequently in older women. Radiation therapy for head and neck
cancer can also cause hypothyroidism in older men; therefore, testing of
thyroid function is recommended for all pa-tients who receive such treatment.
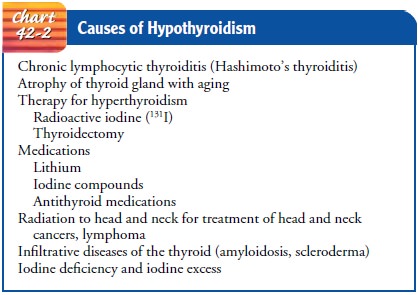
Other causes of hypothyroid-ism are presented in Chart 42-2.
Pathophysiology
More
than 95% of patients with hypothyroidism have primary or thyroidal
hypothyroidism, which refers to dysfunction of the thyroid gland itself. When
thyroid dysfunction is caused by fail-ure of the pituitary gland, the
hypothalamus, or both, it is known as central hypothyroidism. It may be
referred to as pituitary or secondary hypothyroidism if it is caused entirely
by a pituitary disorder, and hypothalamic or tertiary hypothyroidism if it is
at-tributable to a disorder of the hypothalamus resulting in inade-quate
secretion of TSH because of decreased stimulation by TRH. When thyroid
deficiency is present at birth, the condition is known as cretinism. In such
instances, the mother may also suffer from thyroid deficiency.
The
term myxedema refers to the accumulation of mucopoly-saccharides in
subcutaneous and other interstitial tissues. Al-though myxedema occurs in
long-standing hypothyroidism, the term is used appropriately only to describe
the extreme symptoms of severe hypothyroidism.
Clinical Manifestations
Early
symptoms of hypothyroidism are nonspecific, but extreme fatigue makes it
difficult for the person to complete a full day’s work or participate in usual
activities. Reports of hair loss, brittle nails, and dry skin are common, and
numbness and tingling of the fingers may occur. On occasion, the voice may
become husky, and the patient may complain of hoarseness. Menstrual
disturbances such as menorrhagia or amenorrhea occur, in addition to loss of
libido. Hypothyroidism affects women five times more frequently than men and
occurs most often between 30 and 60 years of age.
Severe hypothyroidism results in a subnormal temperature and pulse rate. The patient usually begins to gain weight even without an increase in food intake, although severely hypothyroid patients may be cachectic. The skin becomes thickened because of an accumulation of mucopolysaccharides in the subcutaneous tissues (the origin of the term myxedema). The hair thins and falls out; the face becomes expressionless and masklike. The patient often complains of being cold even in a warm environment.
At
first, the patient may be irritable and may complain of fa-tigue, but as the
condition progresses, the emotional responses are subdued. The mental processes
become dulled, and the patient appears apathetic. Speech is slow, the tongue
enlarges, and hands and feet increase in size. The patient frequently complains
of con-stipation. Deafness may also occur.
Advanced
hypothyroidism may produce personality and cog-nitive changes characteristic of
dementia. Inadequate ventilation and sleep apnea can occur with severe
hypothyroidism. Pleural ef-fusion, pericardial effusion, and respiratory muscle
weakness may also occur.
Severe
hypothyroidism is associated with an elevated serum cholesterol level,
atherosclerosis, coronary artery disease, and poor left ventricular function.
The patient with advanced hypo-thyroidism is hypothermic and abnormally
sensitive to sedatives, opioids, and anesthetic agents. Therefore, these
medications are administered only with extreme caution.
Patients
with unrecognized hypothyroidism who are under-going surgery are at increased
risk for intraoperative hypotension and postoperative heart failure and altered
mental status.
Myxedema
coma describes the most extreme, severe stage of hypothyroidism, in which the
patient is hypothermic and un-conscious. Myxedema coma may follow increasing
lethargy, pro-gressing to stupor and then coma. Undiagnosed hypothyroidism may
be precipitated by infection or other systemic disease or by use of sedatives
or opioid analgesic agents. The patient’s respira-tory drive is depressed,
resulting in alveolar hypoventilation, pro-gressive CO2 retention, narcosis,
and coma. These symptoms, along with cardiovascular collapse and shock, require
aggressive and intensive therapy if the patient is to survive. Even with early
vigorous therapy, however, mortality is high.
Gerontologic Considerations
Most
patients with primary hypothyroidism are 40 to 70 years of age and present with
long-standing mild to moderate hypothy-roidism. Subclinical disease is common
among older women and can be asymptomatic or mistaken for other medical
conditions. Subtle symptoms of hypothyroidism, such as fatigue, muscle aches,
and mental confusion, may be attributed to the normal aging pro-cess by the
patient, family, and health care provider. The higher prevalence of
hypothyroidism in elderly people may be related to alterations in immune
function with age. Regular screening of TSH levels is recommended for people
older than 60 because they are at high risk for hypothyroidism (Ladenson et
al., 2000).
The
signs and symptoms of hypothyroidism are often atypi-cal in elderly people; the
elderly patient may have few or no symp-toms until the dysfunction is severe.
Depression, apathy, or decreased mobility or activity may be the major initial
symptom. The major symptoms of hypothyroidism may be depression and apathy, and
may be accompanied by significant weight loss. One fourth of affected elderly
patients experience constipation
Medical Management
The
primary objective in the management of hypothyroidism is to restore a normal
metabolic state by replacing the missing hormone.
PHARMACOLOGIC THERAPY
Synthetic
levothyroxine (Synthroid or Levothroid) is the pre-ferred preparation for
treating hypothyroidism and suppressing nontoxic goiters. The dosage for
hormone replacement is based on the patient’s serum TSH concentration.
Desiccated thyroid is used less frequently because it often results in
transient elevated serum concentrations of T3, with occasional symptoms of
hyper-thyroidism. If replacement therapy is adequate, the symptoms of myxedema
disappear and normal metabolic activity is resumed.
Prevention of Cardiac Dysfunction.
Any patient
who has hadhypothyroidism for a long period is almost certain to have ele-vated
serum cholesterol levels, atherosclerosis, and coronary artery disease. As long
as metabolism is subnormal and the tissues, including the myocardium, require
relatively little oxygen, a re-duction in blood supply is tolerated without
overt symptoms of coronary artery disease. When thyroid hormone is administered,
however, the oxygen demand increases, but oxygen delivery can-not be increased
unless, or until, the atherosclerosis improves. This occurs very slowly, if at
all. The occurrence of angina is the signal that the oxygen needs of the
myocardium exceed its blood supply. Angina or dysrhythmias may occur when
thyroid replace-ment is initiated because thyroid hormones enhance the
cardio-vascular effects of catecholamines.
Obviously,
if angina or dysrhythmias occur, thyroid hormone administration must be discontinued
immediately. Later, when it can be resumed safely, thyroid hormone replacement
should be prescribed cautiously at a lower dosage and under the close
ob-servation of the physician and the nurse.
Prevention of Medication Interactions.
Precautions must be takenduring the course of therapy because of the
interaction of thyroid hormones with other medications. Thyroid hormones may
in-crease blood glucose levels, which may necessitate adjustment in the dosage
of insulin or oral antidiabetic agents in patients with di-abetes. The effects
of thyroid hormone may be increased by phenytoin (Dilantin) and tricyclic
antidepressant agents. Thyroid hormones may also increase the pharmacologic
effects of digitalis glycosides, anticoagulant agents, and indomethacin,
requiring careful observation and assessment by the nurse for side effects.
Bone loss and osteoporosis may also occur with thyroid therapy.
Even
in small doses, hypnotic and sedative agents may induce profound somnolence,
lasting far longer than anticipated. Moreover, they are likely to cause
respiratory depression, which can easily be fatal because of decreased
respiratory reserve and alveo-lar hypoventilation. If their use is necessary,
the dose is one-half or one-third that ordinarily prescribed in patients of
similar age and weight with normal thyroid function. If these medications must
be used, the patient must be monitored closely for signs of impending narcosis
(stupor-like condition) or respiratory failure.
Gerontologic Considerations
In the
elderly patient with mild to moderate hypothyroidism, thyroid hormone
replacement must be started with low dosages and increased gradually to prevent
serious cardiovascular and neurologic side effects. Angina, for example, may
occur with rapid thyroid replacement in the presence of coronary artery disease
secondary to the hypothyroid state. Heart failure and tachydys-rhythmias may
worsen during the transition from the hypothy-roid state to the normal
metabolic state. Dementia may become more apparent during early thyroid hormone
replacement in the elderly patient.
Elderly
patients with severe hypothyroidism and atheroscle-rosis may also become
confused and agitated if their metabolic rates are raised too quickly. Marked
clinical improvement follows the administration of hormone replacement; such
medication must be continued for life, even though signs of hypothyroidism
disappear within 3 to 12 weeks.
Myxedema
and myxedema coma generally occur exclusively in patients older than 50 years.
The high mortality rate of myxedema coma mandates immediate intravenous
administration of high doses of thyroid hormone as well as supportive care.
SUPPORTIVE THERAPY
In
severe hypothyroidism and myxedema coma, management includes maintaining vital functions. Arterial blood gases
may be measured to determine CO2 retention and to guide the use of
assisted ventilation to combat hypoventilation. Pulse oximetry may also be
helpful in monitoring oxygen saturation levels. Fluids are administered
cautiously because of the danger of water intox-ication. Application of
external heat (eg, heating pads) is avoided because it increases oxygen
requirements and may lead to vas-cular collapse. If hypoglycemia is evident,
concentrated glucose may be prescribed to provide glucose without precipitating
fluid overload. Thyroid hormone (usually Synthroid) is administered intravenously
until consciousness is restored if myxedema has progressed to myxedema coma.
The patient is then continued on oral thyroid hormone therapy. Because of an
associated adreno-cortical insufficiency, corticosteroid therapy may be
necessary.
Nursing Management
Nursing
care of the patient with hypothyroidism and myxedema is summarized in the Plan
of Nursing Care.
MODIFYING ACTIVITY
The patient with hypothyroidism experiences decreased energy and moderate to severe lethargy. As a result, the risk for compli-cations from immobility increases. The patient’s ability to exer-cise and participate in activities is further limited by the changes in cardiovascular and pulmonary status secondary to hypothy-roidism. A major role of the nurse is assisting with care and hygiene while encouraging the patient to participate in activities within established tolerance levels to prevent the complications of immobility.
MONITORING PHYSICAL STATUS
The
nurse closely monitors the patient’s vital signs and cognitive level to detect
the following:
· Deterioration of
physical and mental status
· Signs and symptoms indicating
that treatment has resulted in the metabolic rate exceeding the ability of the
cardio-vascular and pulmonary systems to respond
· Continued limitations or
complications of myxedema
PROMOTING PHYSICAL COMFORT
The
patient often experiences chilling and extreme intolerance to cold, even if the
room feels comfortable or hot to others. Extra clothing and blankets are
provided, and the patient is protected from drafts. Use of heating pads and
electric blankets is avoided because of the risk of peripheral vasodilation,
further loss of body heat, and vascular collapse. Additionally, the patient
could be burned by these items without being aware of it because of de-layed
responses and decreased mental status.
PROVIDING EMOTIONAL SUPPORT
The
patient with moderate to severe hypothyroidism may expe-rience severe emotional
reactions to changes in appearance and body image and the frequent delay in
diagnosis. The nonspecific, early symptoms may produce negative reactions by
family mem-bers and friends, and the family and friends may have labeled the
patient mentally unstable, uncooperative, or unwilling to partic-ipate in
self-care activities.
As
hypothyroidism is treated successfully and symptoms subside, the patient may
experience depression and guilt as a re-sult of the progression and severity of
symptoms that occurred. The nurse informs the patient and family that the
symptoms and inability to recognize them are common and part of the dis-order
itself. The patient and family may require assistance and counseling to deal
with the emotional concerns and reactions that result.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care.
Because most
hypothyroidism treat-ment takes place at home, the patient and family require
infor-mation and instruction that will enable them to monitor the patient’s
condition and response to therapy. The nurse instructs the patient about the
desired actions and side effects of medications and about how and when to take
prescribed medications. The importance of continuing to take medications as
prescribed even after symptoms improve is stressed to the patient. Because of
the slowed mental processes that occur with hypothyroidism, it is im-portant
that a family member also be informed and instructed about treatment goals, medication
schedules, and side effects to be reported to the physician. The nurse provides
written instruc-tions and guidelines for the patient and family.
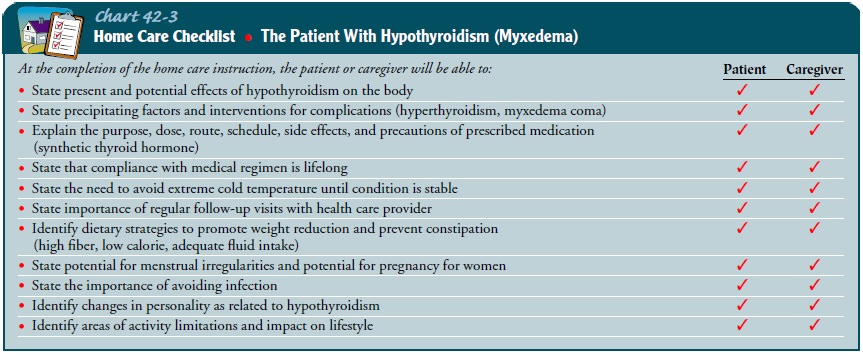
Dietary
instruction is provided to promote weight loss once medication has been
initiated and to promote return of normal bowel patterns. The patient and
family are often very concerned about the changes they have observed as a
result of the hypothy-roid state. It is often reassuring to the patient and
family to be in-formed that many of the symptoms will disappear with effective
treatment (Chart 42-3).
Continuing Care.
The patient
with hypothyroidism and myx-edema coma needs considerable follow-up and health
care. Be-fore hospital discharge, arrangements are made to ensure that the
patient returns to an environment that will promote adherence to the prescribed
treatment plan. Assistance in devising a sched-ule or record ensures accurate
and complete administration of medications. The nurse reinforces the importance
of continued thyroid hormone replacement and periodic follow-up testing and
instructs the patient and family members about the signs of over-medication and
undermedication.
If indicated, a referral is made for home care. The home care nurse assesses the patient’s progress toward recovery and ability to cope with the recent changes, along with the patient’s physical and cognitive status and the patient’s and family’s understanding of the importance of prescribed long-term medication therapy and compliance with the medication schedule and recommended follow-up tests and appointments. The nurse documents, and re-ports to the patient’s primary health care provider, subtle signs and symptoms that may indicate either inadequate or excessive thyroxine hormone.
Gerontologic Considerations
The
elderly patient requires periodic follow-up monitoring of serum TSH levels
because poor compliance with therapy may occur or the patient may take the
medications erratically. A careful history may identify the need for further
teaching about the im-portance of the medication. Because of the prevalence of
hypothy-roidism, testing of serum TSH levels in elderly people every 5 years
has been recommended (Smallridge, 2000). In addition, the pa-tient is reminded
of the importance of participating in general health promotion activities and
recommended health screening.
Related Topics