Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Endocrine Disorders
Hyperparathyroidism - Management of Patients With Parathyroid Disorders
HYPERPARATHYROIDISM
Hyperparathyroidism, which is caused by overproduction of parathyroid hormone by the parathyroid glands, is characterized by bone decalcification and the development of renal calculi (kid-ney stones) containing calcium.
Primary
hyperparathyroidism occurs two to four times more often in women than in men
and is most common in patients be-tween 60 and 70 years of age. About 100,000
new cases of hyper-parathyroidism are detected each year in the United States.
The disease is rare in children younger than 15 years, but the inci-dence
increases tenfold between the ages of 15 and 65 years. Half of the patients
diagnosed with hyperparathyroidism do not have symptoms.
Secondary
hyperparathyroidism, with manifestations similar to those of primary
hyperparathyroidism, occurs in patients with chronic renal failure and
so-called renal rickets as a result of phos-phorus retention, increased
stimulation of the parathyroid glands, and increased parathyroid hormone
secretion.
Clinical Manifestations
The
patient may have no symptoms or may experience signs and symptoms resulting
from involvement of several body sys-tems. Apathy, fatigue, muscle weakness,
nausea, vomiting, con-stipation, hypertension, and cardiac dysrhythmias may
occur; all are attributable to the increased concentration of calcium in the
blood. Psychological manifestations may vary from irri-tability and neurosis to
psychoses caused by the direct effect of calcium on the brain and nervous
system. An increase in cal-cium produces a decrease in the excitation potential
of nerve and muscle tissue.
The
formation of stones in one or both kidneys, related to the increased urinary
excretion of calcium and phosphorus, is one of the important complications of
hyperparathyroidism and occurs in 55% of patients with primary hyperparathy-roidism.
Renal damage results from the precipitation of calcium phosphate in the renal
pelvis and parenchyma, resulting in renal calculi (kidney stones), obstruction,
pyelonephritis, and renal failure.
Musculoskeletal
symptoms accompanying hyperparathyroidism may result from demineralization of
the bones or bone tumors composed of benign giant cells resulting from
overgrowth of osteoclasts. The patient may develop skeletal pain and
tender-ness, especially of the back and joints; pain on weight bearing;
pathologic fractures; deformities; and shortening of body stature. Bone loss
attributable to hyperparathyroidism increases the risk for fracture.
The
incidence of peptic ulcer and pancreatitis is increased with
hyperparathyroidism and may be responsible for many of the gastrointestinal
symptoms that occur.
Assessment and Diagnostic Findings
Primary
hyperparathyroidism is diagnosed by persistent eleva-tion of serum calcium
levels and an elevated level of parathor-mone. Radioimmunoassays for parathormone
are sensitive and differentiate primary hyperparathyroidism from other causes
of hypercalcemia in more than 90% of patients with elevated serum calcium
levels. An elevated serum calcium level alone is a nonspecific finding because
serum levels may be altered by diet, medications, and renal and bone changes.
Bone changes may be detected on x-ray or bone scans in advanced disease. The
double antibody parathyroid hormone test is used to distin-guish between
primary hyperparathyroidism and malignancy as a cause of hypercalcemia.
Ultrasound, MRI, thallium scan, and fine-needle biopsy have been used to
evaluate the function of the parathyroids and to localize parathyroid cysts,
adenomas, or hyperplasia.
Complications: Hypercalcemic Crisis
Acute
hypercalcemic crisis can occur with extreme elevation of serum calcium levels.
Serum calcium levels higher than 15 mg/dL (3.7 mmol/L) result in neurologic,
cardiovascular, and renal symptoms that can be life-threatening. Treatment
includes rehy-dration with large volumes of intravenous fluids, diuretic agents
to promote renal excretion of excess calcium, and phosphate therapy to correct
hypophosphatemia and decrease serum cal-cium levels by promoting calcium
deposit in bone and reducing the gastrointestinal absorption of calcium.
Cytotoxic agents (mithramycin), calcitonin, and dialysis may be used in
emergency situations to decrease serum calcium levels quickly.
A
combination of calcitonin and corticosteroids has been ad-ministered in
emergencies to reduce the serum calcium level by increasing calcium deposition
in bone. Other agents that may be administered to decrease serum calcium levels
include bisphos-phonates (eg, etidronate [Didronel], pamidronate).
The
patient requires expert assessment and care to minimize complications and
reverse the life-threatening hypercalcemia. Medications are administered with
care, and attention is given to fluid balance to promote return of normal fluid
and electrolyte bal-ance. Supportive measures are necessary for the patient and
family.
Medical Management
The
insidious onset and chronic nature of hyperparathyroidism and its diverse and
commonly vague symptoms may result in de-pression and frustration. The family
may have considered the pa-tient’s illness to be psychosomatic. An awareness of
the course of the disorder and an understanding approach by the nurse may help
the patient and family to deal with their reactions and feel-ings. The
recommended treatment of primary hyperparathyroidism is the surgical removal of
abnormal parathyroid tissue. In some patients without symptoms and with only
mildly elevated serum calcium levels and normal renal function, surgery may be
delayed and the patient followed closely for worsening of hypercalcemia, bone
deterioration, renal impairment, or the development of kid-ney stones.
HYDRATION THERAPY
Because
kidney involvement is possible, patients with hyper-parathyroidism are at risk
for renal calculi. Therefore, a fluid in-take of 2,000 mL or more is encouraged
to help prevent calculus formation. Cranberry juice is suggested because it may
lower the urinary pH. It can be added to juices and ginger ale for variety. The
patient is instructed to report other manifestations of renal calculi, such as
abdominal pain and hematuria. Thiazide diuret-ics are avoided because they
decrease the renal excretion of cal-cium and further elevate serum calcium
levels. Because of the risk of hypercalcemic crisis, the patient is instructed
to avoid dehy-dration and to seek immediate health care if conditions that com-monly
produce dehydration (eg, vomiting, diarrhea) occur.
MOBILITY
Mobility
of the patient, with walking or use of a rocking chair for those with limited
mobility, is encouraged as much as possible because bones subjected to normal
stress give up less calcium. Bed rest increases calcium excretion and the risk
for renal calculi. Oral phosphates lower the serum calcium level in some
patients. Long-term use is not recommended because of the risk for ectopic
cal-cium phosphate deposits in soft tissues.
DIET AND MEDICATIONS
Nutritional
needs are met, but the patient is advised to avoid a diet with restricted or
excess calcium. If the patient has a coexist-ing peptic ulcer, prescribed
antacids and protein feedings are nec-essary. Because anorexia is common, efforts
are made to improve the appetite. Prune juice, stool softeners, and physical
activity, along with increased fluid intake, help to offset constipation, which
is common postoperatively.
Nursing Management
The
nursing management of the patient undergoing parathy-roidectomy is essentially
the same as that of a patient undergoing thyroidectomy. However, the previously
described precautions about dehydration, immobility, and diet are particularly
impor-tant in the patient awaiting and recovering from parathyroidec-tomy.
Although not all parathyroid tissue is removed during surgery in an effort to
control the calcium–phosphorus balance, the nurse closely monitors the patient
to detect symptoms of tetany (which may be an early postoperative
complication). Most patients quickly regain function of the remaining
parathyroid tis-sue and experience only mild, transient postoperative
hypocal-cemia. In patients with significant bone disease or bone changes, a
more prolonged period of hypocalcemia should be anticipated. The nurse reminds
the patient and family about the importance of follow-up to ensure return of
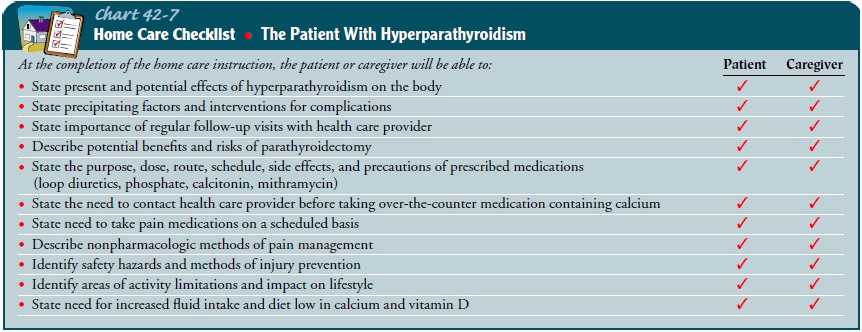
serum calcium levels to normal (Chart 42-7).
Related Topics