Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Hearing and Balance Disorders
Assessment of Patients With Hearing and Balance Disorders
Assessment
The
external ear is examined by inspection and direct palpation, and the tympanic
membrane is inspected with an otoscope and indirect palpation with a pneumatic
otoscope. Until the advent of middle ear endoscopy, inspection of the middle
ear was im-possible. Evaluation of gross auditory acuity also is included in
every physical examination.
INSPECTION OF THE EXTERNAL EAR
Inspection
of the external ear is a simple procedure, but it is often overlooked. The
auricle and surrounding tissues should be in-spected for deformities, lesions,
and discharge, as well as size, symmetry, and angle of attachment to the head.
Manipulation of the auricle does not normally elicit pain. If this maneuver is
pain-ful, acute external otitis is suspected. Tenderness on palpation in the
area of the mastoid may indicate acute mastoiditis or inflam-mation of the
posterior auricular node. Occasionally, sebaceous cysts and tophi (ie,
subcutaneous mineral deposits) are present on the pinna. A flaky scaliness on
or behind the auricle usually indi-cates seborrheic dermatitis and can be
present on the scalp and facial structures as well.
OTOSCOPIC EXAMINATION
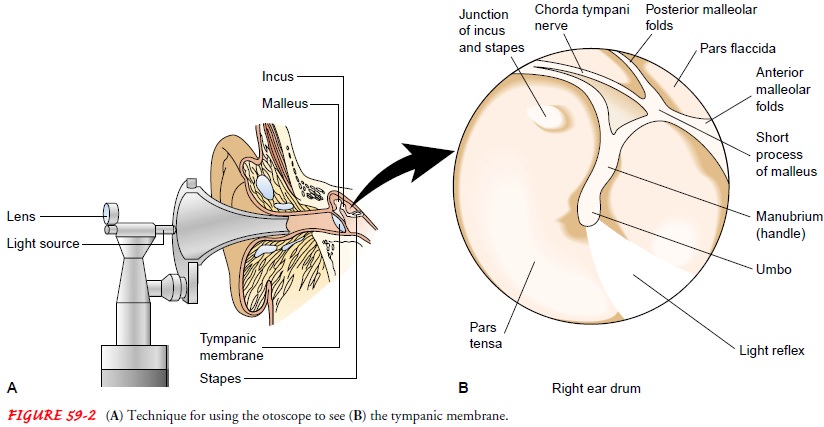
To
examine the external auditory canal and tympanic membrane, the otoscope should
be held in the examiner’s right hand, in a pencil-hold position, with the
bottom of the scope pointing up (Fig. 59-4). This position prevents the
examiner from inserting the otoscope too far into the external canal. Using the
opposite hand, the auricle is grasped and gently pulled back to straighten the
canal in the adult. If the canal is not straightened with this technique, the
tympanic membrane is harder to visualize because of the canal obstructing the
view.

The speculum is slowly inserted into the ear canal,
with the examiner’s eye held close to the magnifying lens of the otoscope to
visualize the canal and tympanic membrane. The largest specu-lum that the canal
can accommodate (usually 5 mm in an adult) is guided gently down into the canal
and slightly forward. Be-cause the distal portion of the canal is bony and
covered by a sen-sitive layer of epithelium, only light pressure can be used
without causing pain. The examiner looks for any discharge, inflammation, or
foreign body in the external auditory canal.
The
healthy tympanic membrane is pearly gray and is posi-tioned obliquely at the
base of the canal. The landmarks are iden-tified, if visible (see Fig. 59-2):
the pars tensa, the umbo, the manubrium of the malleus, and its short process.
A slow, circular movement of the speculum allows further visualization of the
malle-olar folds and periphery. The position and color of the membrane and any
unusual markings or deviations from normal are docu-mented. The presence of
fluid, air bubbles, blood, or masses in the middle ear also are noted.
Proper otoscopic examination of the external auditory canal and tympanic membrane requires that the canal be free of large amounts of cerumen. Cerumen is normally present in the exter-nal canal, and small amounts should not interfere with otoscopic examination. If the tympanic membrane cannot be visualized because of cerumen, the cerumen may be removed by gently irri-gating the external canal with warm water (if there are no contra-indications to this). If adherent cerumen is present, a small amount of mineral oil or over-the-counter cerumen softener may be instilled within the ear canal, and the patient is instructed to return for subsequent removal of the cerumen and inspection of the ear.
The use of instruments such as a cerumen curette for
ceru-men removal is reserved for otolaryngologists and nurses with spe-cialized
training because of the danger of perforating the tympanic membrane or
excoriating the external auditory canal. Cerumen buildup is a common cause of
hearing loss and local irritation.
EVALUATION OF GROSS AUDITORY ACUITY
A
general estimation of hearing can be made by assessing the pa-tient’s ability
to hear a whispered phrase or a ticking watch, test-ing one ear at a time. The
Weber and Rinne tests may be used to distinguish conductive loss from
sensorineural loss when hearing is impaired. These tests are part of the usual
screening physical examination and are useful if a more specific assessment is
needed, if hearing loss is detected, or if confirmation of audiometric results
is desired.
Whisper Test
To
exclude one ear from the testing, the examiner covers the untested ear with the
palm of the hand. Then the examiner whis-pers softly from a distance of 1 or 2
feet from the unoccluded ear and out of the patient’s sight. The patient with
normal acuity can correctly repeat what was whispered.
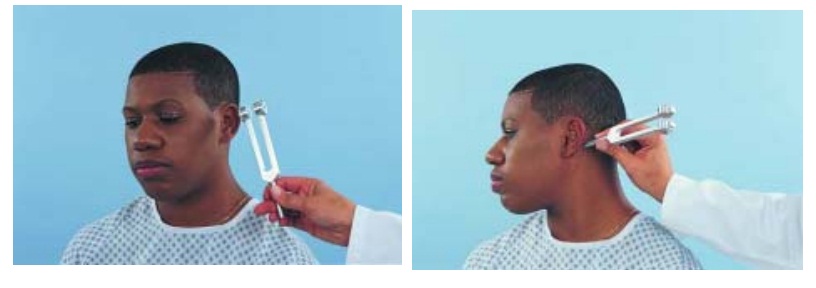
Weber Test
The Weber test uses bone conduction to test lateralization of sound. A tuning fork (ideally, 512 Hz), set in motion by grasping it firmly by its stem and tapping it on the examiner’s knee or hand, is placed on the patient’s head or forehead (Fig. 59-5). A person with normal hearing will hear the sound equally in both ears or describe the sound as centered in the middle of the head. In cases of conductive hearing loss, such as from otosclerosis or otitis media, the sound is heard better in the affected ear.

In cases of sensorineural hearing loss,
resulting from damage to the cochlear orvestibulocochlear nerve, the sound
lateralizes to the better-hearing ear. The Weber test is useful for detecting
unilateral hearing loss (Table 59-1).
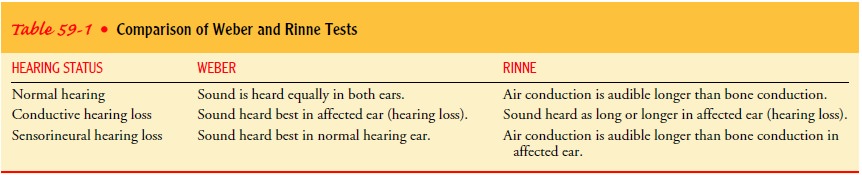
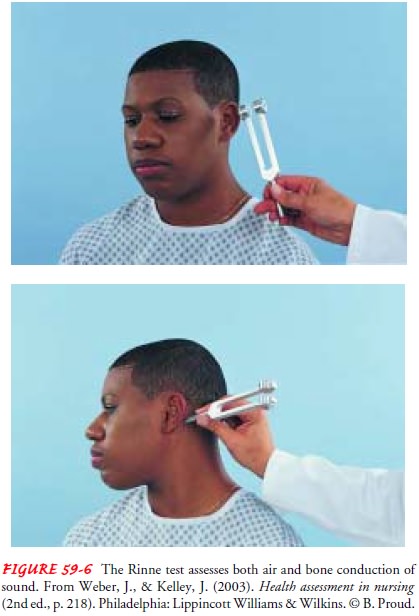
Rinne Test
In
the Rinne test (pronounced rin-ay), the examiner shifts the stem of a vibrating
tuning fork between two positions: 2 inches from the opening of the ear canal
(ie, for air conduction) and against the mastoid bone (ie, for bone conduction)
(Fig. 59-6). As the position changes, the patient is asked to indicate which
tone is louder or when the tone is no longer audible. Normally, sound heard by
air conduction is audible longer than sound heard by bone conduction. The Rinne
test is useful for distinguishing between conductive and sensorineural hearing
losses. With a con-ductive hearing loss, bone-conducted sound is heard as long
as or longer than air-conducted sound, whereas with a sensorineural hearing
loss, air-conducted sound is audible longer than bone-conducted sound. In a
normal hearing ear, air-conducted sound is louder than bone-conducted sound.
Related Topics