Chapter: Medicine and surgery: Hepatic, biliary and pancreatic systems
Acute pancreatitis - Disorders of the pancreas
Acute pancreatitis
Definition
Acute inflammation of the pancreas with variable involvement of local tissue and other organs.
Incidence
Almost 5–25 per 100,000 per year and rising.
Age
More common >40 years.
Sex
M > F
Aetiology
Biliary tract disease (80%), especially cholelithiasis, gallstones are present in up to half of all cases although often in the gallbladder rather than impacted. Alcoholism is the second most common cause (20% in the United Kingdom). Causes are as follows:
· Obstruction: Gallstones, biliary sludge, carcinoma of the pancreas.
· Drugs/toxins: Alcohol, azathioprine, steroids, diuretics.
· Metabolic: Hypercalcaemia, hyperlipidaemia. Infections: Coxsackie, mumps, Mycoplasma.
· Trauma: Blunt or penetrating injury, postsurgery, post-ERCP.
· Autoimmune: Polyarteritis nodosa, systemic lupus erythematosus.
Pathophysiology
The pancreatic acini and ducts become damaged, this leads to release and activation of the digestive enzymes of the pancreas which autolyse the tissues. Proteolysis due to proteases, fat necrosis due to lipases and phos-pholipases and haemorrhage occur. Translocation of gut bacteria can result in local infection and septicaemia. Shock may result from the release of bradykinin and prostaglandins, or secondary to sepsis.
Clinical features
Patients present with severe abdominal pain, which is continuous epigastric pain radiating to the upper back, often associated with vomiting. On examination there is epigastric guarding. Less commonly, the patient may be jaundiced and shocked. Haemorrhage may cause Grey– Turner’s sign, which is bruising around the left loin and/or Cullen’s sign, bruising around the umbilicus.
Macroscopy/microscopy
The pancreas appears oedematous with grey-white necrotic patches. Bacterial infection leads to inflammation and pus formation. Healing results in fibrosis with calcification.
Complications
In the most severe cases there is systemic organ failure:
· Cardiovascular system: Shock (hypotension, tachycardia, arrhythmias).
· Respiratory system: Adult respiratory distress syndrome, respiratory failure.
· Kidney: Acute renal failure.
· Metabolic: Hypocalcaemia, hypoglycaemia.
· Haematology: Altered haematocrit (raised or lowered), clotting abnormalities (thrombosis, disseminated intravascular coagulation).
· Central nervous system: Neurological symptoms include confusion and irritability.
· Local complications include pancreatic haemorrhage, pseudocyst (a collection of fluid and pancreatic enzymes walled off by compressed tissue), pancreatic abscesses (which may contain gas indicating infection with gas-forming bacteria) and duodenal obstruction.
Investigations
When supportive clinical features are present the diagnosis can be made with a serum amylase more than four times normal, or by a lipase activity greater than twice normal. Patients with acute on chronic pancreatitis may have a smaller rise in serum amylase, in such cases a urinary amylase may be useful to confirm the diagnosis.
Ultrasound (to look for gallstones) of the gallbladder and biliary tract should be performed, but CT scanning is the most useful imaging modality for the pancreas.
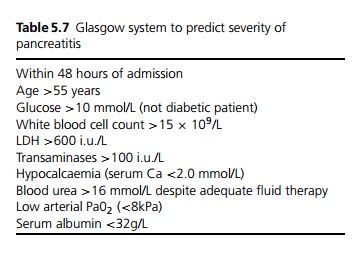
Other investigations are required to assess the severity and to monitor for complications: full blood count, clotting screen, urea and electrolytes, liver function tests, lactate dehydrogenase, calcium levels, blood glucose, C reactive protein and arterial blood gas (see Table 5.7).
Management
The early management depends on the severity of the disease, and later management depends on the aetiology and any complications.
· Mild attacks can be admitted to a general ward. Initial treatment is supportive with correction of hypo-volaemia and electrolyte imbalances, insertion of a nasogastric tube and analgesia (opiates are often required). Antibiotics should only be given if there are focal signs of infection, e.g. biliary sepsis or pneumonia.
· Severe cases should be managed on a high dependency unit (or intensive care unit if they require respiratory support). Patients require careful fluid balance using central venous pressure monitoring and urinary catheterisation to allow accurate urine output measurement. Regular arterial blood gases are needed to detect early respiratory compromise. Prophylactic broad-spectrum antibiotics are given to reduce the risk of infective complications.
· Gallstone-associated pancreatitis: in mild cases which settle with supportive therapy, early (within 2–4 weeks) cholecystectomy should be performed, with operative cholangiography if ERCP is not performed perioperatively. In cases which do not settle, particularly those with biliary obstruction or sepsis, urgent ERCP and papillotomy is indicated.
· Laparotomy may be required to drain retroperitoneal collections of pus, resect any necrotic pancreatic and peripancreatic tissue, and perform peritoneal irrigation. Pancreatic pseudocysts which do not resolve with conservative management require laparoscopic drainage into the stomach.
Prognosis
Pancreatitis is a serious condition: overall mortality is 10%. The prognostic factors are listed in Table 5.7. If less than three criteria are met then the pancreatitis is considered mild and has <3% mortality. If more than three criteria are met the pancreatitis is considered severe and has >60% mortality.
Related Topics