Chapter: Clinical Cases in Anesthesia : Ambulatory Surgery
What is total intravenous anesthesia (TIVA), and what are its advantages and disadvantages?
What is total intravenous
anesthesia (TIVA), and what are its advantages and disadvantages?
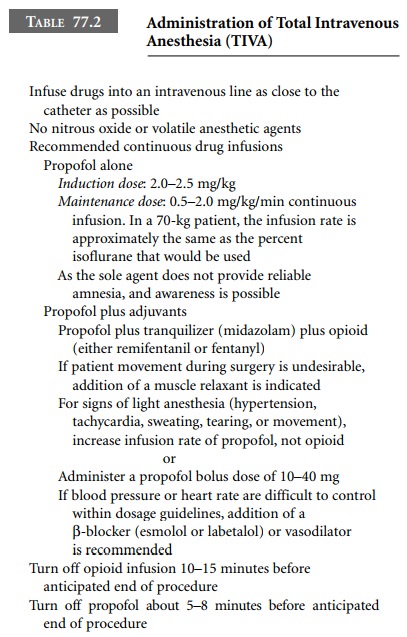
TIVA is a technique in which continuous or
bolus doses of intravenous infusions of anesthetic drugs are administered for
induction and maintenance of anesthesia (Table 77.2). The various components of
a general anesthetic—hypnosis, amnesia, analgesia, as well as muscle
relaxation—can be individually provided and controlled by varying the rates of
infusion, thereby influencing serum concentrations. The depth of anesthesia can
be controlled in a similar manner to dialing in desired concentrations on a
vaporizer.
TIVA avoids the use of all gases with the
exception of oxygen, compressed air, or helium. Therefore, contami-nation of
the operating room suite that invariably occurs when using volatile agents,
despite the use of scavenger systems, may be eliminated entirely. Intravenous
drugs are used to provide unconsciousness, anesthesia, and muscle relaxation,
if desired. Because nonflammable gases may be employed, the technique is ideal
for laser surgery. For procedures on the upper airway, TIVA is perfect for use
with jet Venturi ventilation. Additionally, intravenous anesthesia does not
depend on normal pulmonary func-tion for either wash-in or washout of active
agent.
The further refinement of computer-assisted
infusion systems will allow the anesthesiologist to achieve therapeu-tic blood
concentrations of various anesthetic and sedative drugs. Episodes of “light”
anesthesia can be treated with bolus doses or increased rate of infusion.
Additional benefits of the technique are the potential for attainment of rapid
awakening at the conclusion of the surgical procedure and decreased nausea and
vomiting in the postoperative period in patients who receive propofol.
Since few facilities have monitors that measure
the blood concentration of the intravenous anesthetics, a potential
disadvantage of the technique may include the risk of patient awareness during
surgery. However, presently there are sev-eral monitors that use processed
electroencephalography (EEG) data to monitor the depth of sedation, and may in
fact decrease the risk of awareness during a general anes-thetic. Each monitor
uses a proprietary algorithm to ana-lyze EEG data to derive a linear score of
0–100. A score of 0 usually denotes complete EEG suppression while a score of
100 usually correlates with the awake unsedated state. Each monitor has its own
range of numbers that correlate with general anesthesia. These monitors have
proven to be very helpful intraoperatively in the decision-making tree of the
anesthesiologist.
Traditionally, when a patient became
hypertensive or tachycardic intraoperatively, the anesthesiologist would
usually deepen the anesthetic. However, this change in vital signs can be
attributed to several causes, and has been repeatedly shown to correlate very
poorly with anesthetic depth. The most common of these causes are “light”
anes-thesia, pain, or intrinsic hypertension. If during this period of
increased heart rate and blood pressure there is a con-comitant rise in the score
to above the general anesthesia level, the most likely cause is “light”
anesthesia. Thus, the appropriate response would be to deepen the depth of
anesthesia with a bolus of propofol. If, however, the score on the monitor of
anesthetic depth remains within the range for general anesthesia, the response
would be to give an opi-oid for pain. The choice of opioid would be either an
ultra-short-acting opioid, such as remifentanil, for a short-lived painful
stimulus (i.e., esophagoscopy) or a longer acting opioid, such as fentanyl, for
a persistent painful stimulus (i.e., an incision). However, care must be taken
to utilize the information gleaned from a depth of anesthesia moni-tor in
conjunction with all clinical data, including the pro-cedure being done, the
medical condition of the patient, the patient’s need for perfusion to the vital
organs, as well as hemodynamic variables.
Monitors of anesthetic depth are particularly
useful in the ambulatory setting since they have been associated with decreases
in times to extubation, postoperative nausea and vomiting, and time to home
readiness. Whether or not it is cost-effective to utilize this monitor on all
patients has been heatedly debated in the anesthesia community.
Related Topics