Chapter: Essentials of Psychiatry: Somatoform Disorders
Undifferentiated Somatoform Disorder
Undifferentiated Somatoform Disorder
Definition
As defined in DSM-IV, this category includes disturbances of at least 6
months’ duration, with one or more unintentional, clini-cally significant,
medically unexplained physical complaints (see Table 54.1). In a sense, it is a
residual category, subsuming syn-dromes with somatic complaints that do not
meet criteria for any of the “differentiated” somatoform disorders yet are not
better accounted for by any other mental disorder. On the other hand, it is a
less residual category than somatoform disorder NOS, in that the disturbance
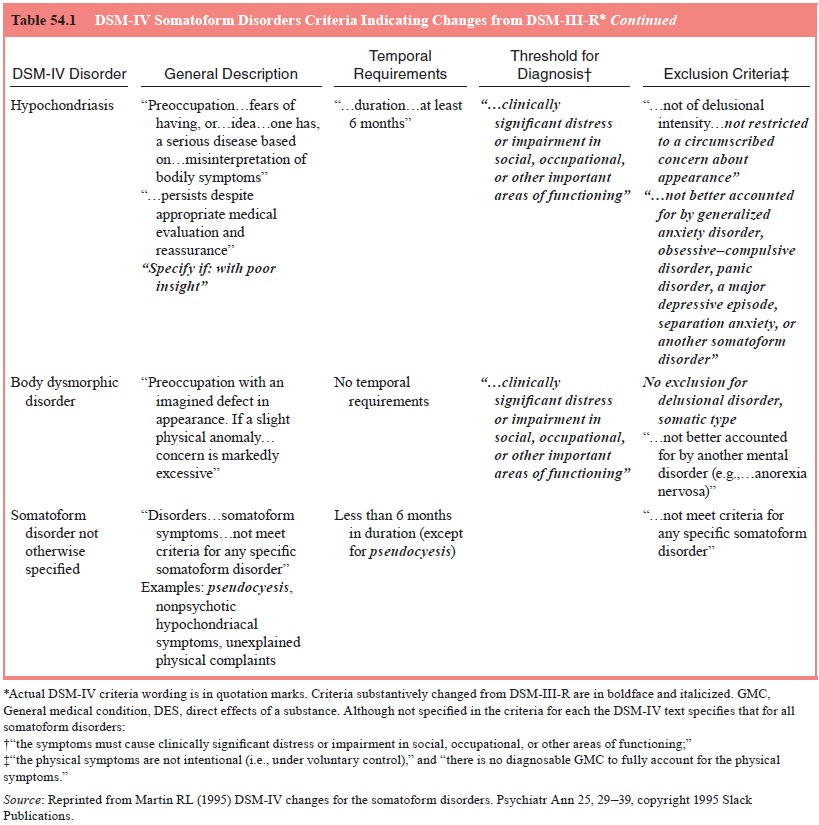
must last at least 6 months (see Figure 54.1). Vir-tually any unintentional,
medically unexplained physical symp-toms causing clinically significant
distress or impairment can be considered. In effect, this category serves to
capture syndromes that resemble somatization disorder but do not meet full
criteria.
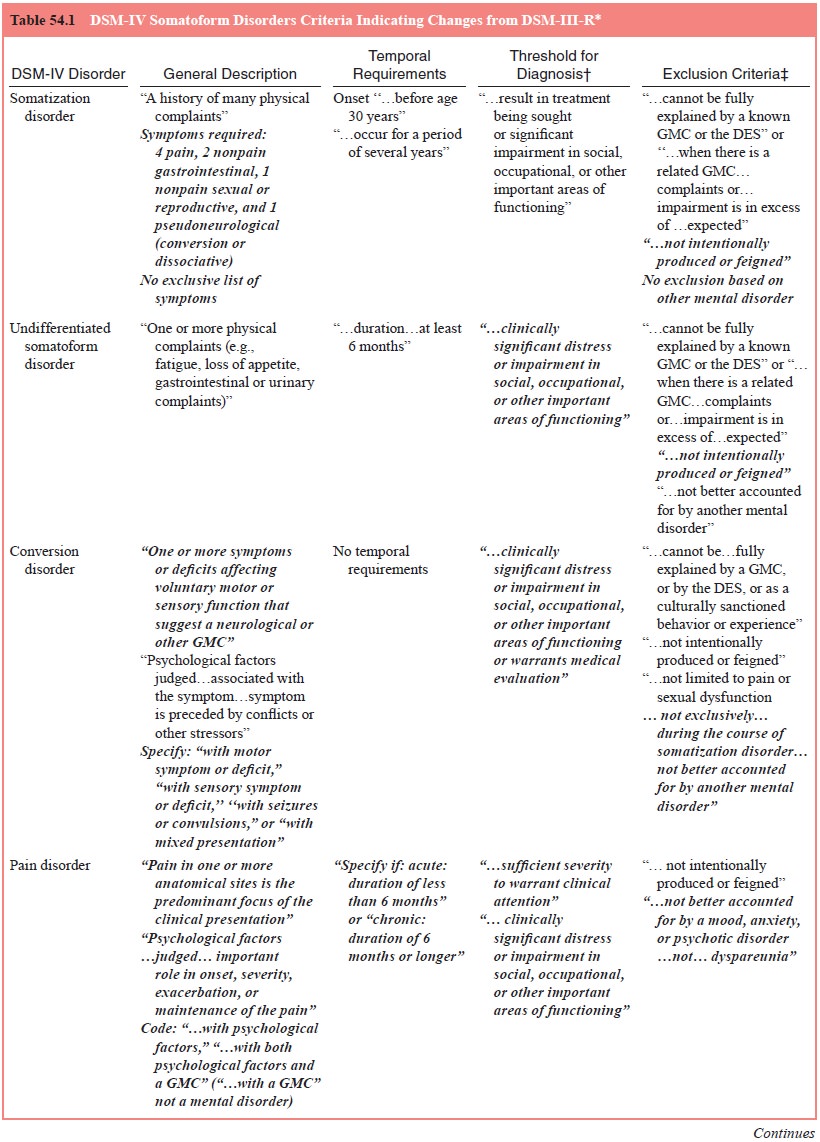
Epidemiology
Some have argued that undifferentiated somatoform disorder is the most
common somatoform disorder. Escobar and coworkers (1991), using an abridged
somatization disorder construct requir-ing six somatic symptoms for women and
four for men, reported that 11% of nonHispanic US whites and Hispanics, 15% of
US blacks and 20% of Puerto Ricans in Puerto Rico fulfilled criteria. A
preponderance of women was evident in all groups except the Puerto Rican sample
(see Table 54.1). According to Escobar, such an abridged somatoform syndrome is
100 times more prevalent than a full somatoform syndrome
Diagnosis and Differential Diagnosis
In comparison to when the full criteria for the well-validated
so-matization disorder are met, exclusion of an as yet undiscovered general
medical or substance-induced explanation for physical symptoms is far less
certain when the less stringent criteria for undifferentiated somatoform
disorder are met. Thus, the diagno-sis of undifferentiated somatoform disorder
should remain tenta-tive, and new symptoms should be carefully investigated.
Because undifferentiated somatoform disorder represents somewhat of a
residual category, the major diagnostic process, once occult general medical
conditions and substance-induced explanations have been considered, is one of
exclusion. As shown in Figure 54.1, whether the somatic symptoms are
intentionally produced as in malingering and factitious disorder must be
ad-dressed. Here, motivation for external rewards (for malingering) and a
pervasive intent to assume the sick role (for factitious dis-order) must be
assessed. The next consideration is whether the somatic symptoms are the
manifestation of another psychiatric disorder. Anxiety and mood disorders
commonly present with somatic symptoms; high rates of anxiety and major
depressive disorders are reported in patients with somatic complaints
at-tending family medicine clinics. Of course, undifferentiated somatoform
disorder could be diagnosed in addition to one of these disorders, so long as
the symptoms are not accounted for by the other psychiatric disorder. Crucial
in this determination is whether the symptoms are present during periods in
which the anxiety or mood disorders are not actively present.
Next, other somatoform disorders must be considered. In general,
undifferentiated somatoform disorders are characterized by unexplained somatic
complaints; the most common accord-ing to Escobar and coworkers (Escobar et al., 1989) are female reproductive
symptoms, excessive gas, abdominal pain, chest pain, joint pain, palpitations
and fainting, rather than preoccupa-tions or fears as in hypochondriasis or
body dysmorphic disor-der. However, a patient with some manifestations of these
two disorders but not meeting full criteria could conceivably receive a
diagnosis of undifferentiated somatoform disorder. An exam-ple is a patient with
recurrent yet shifting hypochondriacal con-cerns that do respond to medical
reassurance. If symptoms are restricted to those affecting the domains of
sexual dysfunction, pain, or pseudoneurological symptoms, and the specific
criteria for a sexual dysfunction, pain disorder and/or conversion disor-der
are met, the specific disorder or disorders should be diag-nosed. If other
types of symptoms or symptoms of more than one of these disorders have been
present for at least 6 months, yet criteria for somatization disorder are not
met, undifferentiated somatoform disorder should be diagnosed. By definition,
undif-ferentiated somatoform disorder requires a duration of 6 months. If this
criterion is not met, a diagnosis of somatoform disorder NOS should be considered.
Patients
with an apparent undifferentiated somatoform disorder should be carefully
evaluated for somatization disorder. Typically, patients with somatization
disorder are inconsistent his-torians, at one evaluation reporting a large
number of symptoms fulfilling criteria for the full syndrome, at another time
endorsing fewer symptoms. In addition, with follow-up, additional symp-toms may
become evident, and criteria for somatization disorder will be satisfied.
Patients with multiple somatic complaints not diagnosed with somatization
disorder because of a reported onset later than 30 years of age may be
inaccurately reporting a later age at onset. If the late age at onset is
accurate, the patient should be carefully scrutinized for an occult general
medical disorder.
In addition to the range of symptoms specified in the other somatoform
disorders, patients complaining primarily of fatigue (chronic fatigue
syndrome), bowel problems (irritable bowel syn-drome), or multiple muscle
aches/weakness (fibromylagia) can be considered for undifferentiated somatoform
disorder. Substantial controversy exists regarding the etiology of such
syndromes. Even if an explanation on the basis of a known pathophysiological
mechanism cannot be established, many argue that the syndromes should be
considered general medical conditions. However, for the time being, these
syndromes could be considered in a highly tentative manner under the
undifferentiated somatoform disorder rubric. Careful reconsideration of the
psychiatric label should be undertaken at regular intervals if the symptoms
persist. The psy-chiatrist should remain ever vigilant to the emergence of
another general medical or psychiatric condition. When patients are di-agnosed
with chronic fatigue syndrome, careful evaluation pro-cedures are recommended.
Course, Natural History and Prognosis
As shown in Table 54.1, it appears that the course and prognosis of
undifferentiated somatoform disorder are highly variable. This is not
surprising, because the definition of this disorder allows a great deal of
heterogeneity.
Treatment
In view of the broad inclusion and minimal exclusion criteria for
undifferentiated somatoform disorder, it is difficult to make treat-ment
recommendations beyond the generic guidelines outlined for the somatoform
disorders in general. More definitive recom-mendations await a more extensive
empirical database. A sub-stantial proportion of patients with undifferentiated
somatoform disorders improve or recover with no formal therapy. However,
appropriate psychotherapy and pharmacological intervention may accelerate the
process.
Some recommendations for patients with symptoms of headache,
fibromyalgia, and chronic fatigue syndrome, condi-tions that some would include
under undifferentiated somatoform disorder. Generally recommended are brief
psychotherapy of a supportive and educative nature. As with somatization
disorder, the physician–patient relationship is of great importance. Judi-cious
use of pharmacotherapy may also be of benefit, particularly if the somatoform
syndrome is intertwined with an anxiety or depressive syndrome. Here, usual
antianxiety and antidepressant medications are recommended. Patients with
unexplained pains may benefit from pain management strategies as outlined in
the pain disorder section.
Related Topics