Chapter: Essentials of Psychiatry: Somatoform Disorders
Hypochondriasis
Hypochondriasis
Definition
The essential feature in hypochondriasis is preoccupation with fears or
the idea of having a serious disease based on the “mis-interpretation of bodily
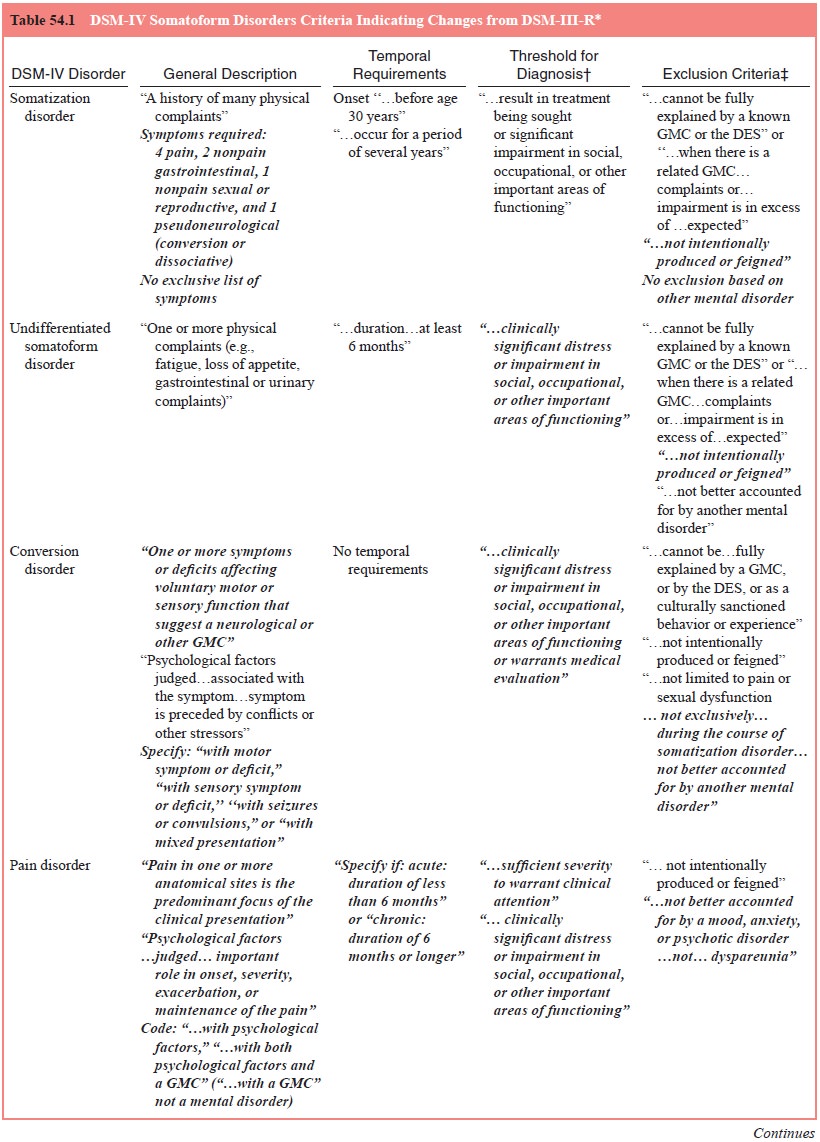
symptoms”. (see Table 54.1). This is in contrast to somatization disorder,
conversion disorder and pain disorder, in which the symptoms themselves are the
predominant focus. There was some debate in the development of DSM-IV as to
whether it was necessary that a body complaint be present. On the basis of
empirical data, however, it was determined that this requirement was a valid
one and helped to distinguish the “disease conviction” of hypochondriasis from
“disease fear” as in phobic disorder. Bodily symptoms may be interpreted
broadly to include misinterpretation of normal body functions. In hypo-chondriasis,
the preoccupation persists despite reassurance from physicians and the
accumulation of evidence to the contrary. As in the other somatoform disorders,
symptoms must result in clinically significant distress or impairment in
important areas of functioning. The duration must be at least 6 months.
Hypochon-driasis is not diagnosed if the hypochondriacal concerns are bet-ter
accounted for by another psychiatric disorder, such as major depressive
episodes or various psychotic disorders with somatic delusions.
Throughout the modern period, there has been contro-versy as to whether
hypochondriasis represented an independent, discrete disease entity. Some
maintain that hypochondriasis is virtually always secondary to another
psychiatric disorder, usu-ally depression. A number of studies suggested that
of the many patients with hypochondriacal complaints, few meet criteria for the
full diagnosis. Moreover, the lack of bimodality to the com-plaints suggests a
continuum rather than a discrete entity.
In the development of DSM-IV, owing to observations that the disease
conviction resembled disease phobia or the incorrigi-ble ideas of
obsessive–compulsive disorder, placement of hypo-chondriasis with the anxiety
disorders was considered. Similarly, a case can be made that disease conviction
is on a continuum with somatic delusions of disease, suggesting inclusion with
the delu-sional disorders. In the end, such considerations were resolved by
keeping hypochondriasis with the somatoform disorders, de-fining it in terms of
an idea that one already has a particular ill-ness rather than fears of
acquiring one to distinguish it from a disease phobia, and by excluding cases
in which the idea was of delusional proportions to differentiate
hypochondriasis from delusional disorder, somatic type.
Epidemiology
Some degree of preoccupation with disease is apparently com-mon. As
reviewed by Kellner (1991), 10 to 20% of “normal” and 45% of “neurotic” persons
have intermittent unfounded worries about illness, with 9% of patients doubting
reassurances given by physicians. Kellner also estimated that 50% of all
patients attend-ing physicians’ offices “suffer either primary hypochondriacal
symptoms or have minor somatic disorders with hypochondriacal
overlay”. How these relate to hypochondriasis as a disorder is difficult to
assess because these estimates do not appear to dis-tinguish between a focus on
the symptoms themselves (as in somatization disorder) and preoccupation with
the implications of the symptoms (as in hypochondriasis). The Epidemiological
Catchment Area study (Robins et al., 1984) did not consider hy-pochondriasis. A 1965
study reported prevalence figures ranging from 3 to 13% in different cultures,
but it is not clear whether this represents a syndrome comparable to the current
definition or just hypochondriacal symptoms. As already noted, many pa-tients
manifest some hypochondriacal symptoms as part of other psychiatric disorders,
and others have transient hypochondriacal symptoms in response to stresses such
as serious physical illness yet never fulfill the inclusion criteria for DSM-IV
hypochondria-sis. Assessment of the incidence and prevalence of
hypochondria-sis undoubtedly requires study of general or primary care rather
than psychiatric populations, because patients with hypochon-driasis are
convinced that they suffer from some physical illness. To date, study of such
populations suggests that 4 to 9% of pa-tients in general medical settings
suffer from hypochondriasis.
It does appear that hypochondriasis is equally common in males and
females.
Etiology and Pathophysiology
Until recently, psychoanalytic hypotheses of etiology predomi-nated.
Freud hypothesized that hypochondriasis represented “the return of object
libido onto the ego with cathexis of the body” (Viederman, 1985). Subsequently,
the cathexis to the body hy-pothesis was elaborated on to include
interpretations involving disturbed object relations – displacement of
repressed hostility to the body to communicate anger indirectly to others.
Dynamic mechanisms involving masochism, guilt, conflicted dependency needs and
a need to suffer and be loved at the same time have also been suggested
(Stoudemire, 1988). The presence of such “narcissistic” mechanisms has been
suggested as the reason that patients with hypochondriasis were “unanalyzable”.
Other psy-chological theories involve defense against feelings of low
self-esteem and inadequacy, perceptual and cognitive abnormalities, and operant
conditioning involving reinforcement for assump-tion of the sick role.
Biological theories have been suggested as well. Hypo-chondriacal ideas
have been attributed to a hypervigilance to insult, including overperception of
physical problems. This has been posited in particular in reference to
hypochondriasis as an aspect of depression or anxiety disorders.
Hypochondriasis has been included by some in the posited obsessive–compulsive
spectrum disorders along with obsessive–compulsive and body dysmorphic
disorders, anorexia nervosa, Tourette’s disorder, tri-chotillomania, pathological
gambling and other impulsive disor-ders. All these disorders involve repetitive
thoughts or behaviors that patients are unable to delay or inhibit without
great difficulty. Evidence for this clustering includes observations of
clinical im-provement with SSRIs such as fluoxetine even in nondepressed
patients with hypochondriasis, body dysmorphic disorder, obses-sive–compulsive
disorder and anorexia nervosa. Because such a response is not evident with
nonSSRI antidepressants, some type of common serotonin dysregulation is
suggested for these disorders.
Diagnosis and Differential Diagnosis
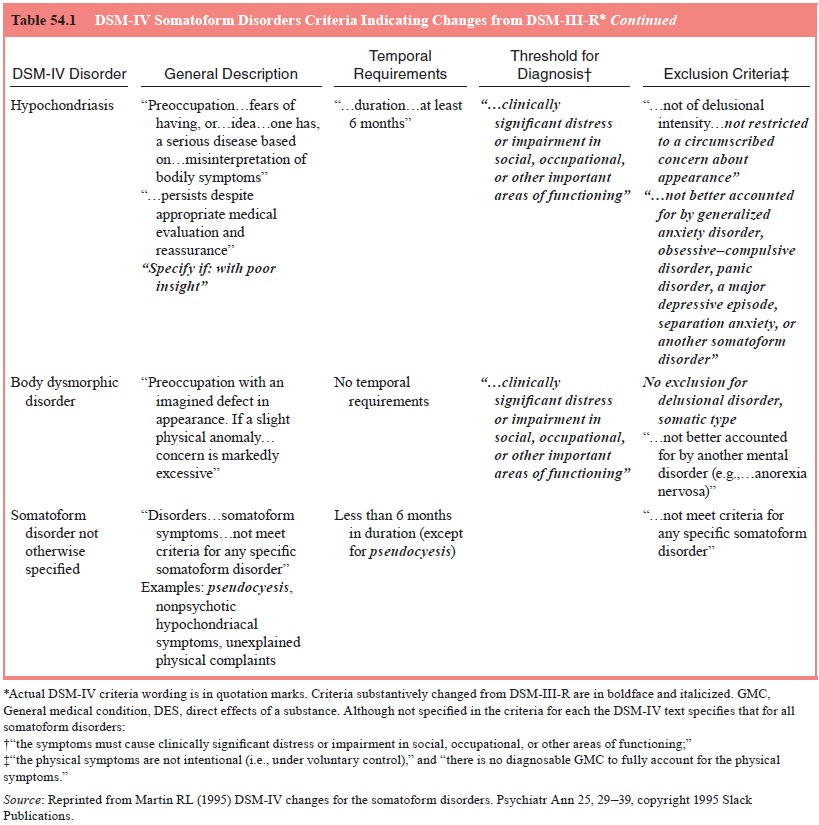
As shown in Figure 54.1, the first step in approaching patients with
distressing or impairing preoccupation with or fears of having a serious
disease is to exclude the possibility of explanation on the basis of a general
medical condition. Fears that may seem excessive may also occur in patients
with general medical conditions with vague and subjective symptoms early in
their disease course. These include neurological diseases, such as myasthenia
gravis and multiple scle-rosis; endocrine diseases; systemic diseases that
affect several organ systems, such as systemic lupus erythematosus; and occult
malignant neoplasms. The disease conviction of hypochondriasis may actually be
less amenable to medical reassurance than the fears of patients, with general
medical illnesses, who may at least temporally accept such encouragement.
Hypochondriacal complaints are not often in-tentionally produced such that
differentiation from malingering and factitious disorder is seldom a problem.
Exclusion is made if the preoccupation is better accounted for by
another psychiatric disorder. DSM-IV lists generalized anxiety disorder,
obsessive–compulsive disorder, panic disorder, a major depressive episode,
separation anxiety, or another so-matoform disorder as candidates. Chronology
will be of utmost importance in such discriminations. Hypochondriacal concerns
occurring exclusively during episodes of another disturbance, such as an
anxiety or depressive disorder, do not warrant an ad-ditional diagnosis of
hypochondriasis. The presence of other psy-chiatric symptoms will also be
helpful. For example, a patient with hypochondriacal complaints as part of a
major depressive episode will show other symptoms of depression, such as sleep
and appetite disturbance, feelings of worthlessness and self-reproach, although
depressed elderly patients may deny sadness or other expressions of depressed
mood. A confounding factor is that patients with hypochondriasis often have
comorbid anxiety or depressive syndromes. Again, characterizing the symptoms by
chronology will be useful. Treatment trials may also have diag-nostic
significance. Depressed patients who are hypochondriacal may respond to nonSSRI
antidepressant medications or elec-troconvulsive therapy (often necessary to
reverse a depressive state of sufficient severity to lead to such profound
symptoms), with resolution of the hypochondriacal as well as the depressive
symptoms.
Hypochondriasis is differentiated from other somatoform disorders such
as pain, conversion and somatization disorders by its predominant feature of
preoccupation with and fears of having an underlying illness based on the
misinterpretation of body symptoms, rather than the physical symptoms
themselves. Patients with these other somatoform disorders at times are
con-cerned with the possibility of underlying illness, but this will gen-erally
be overshadowed by a focus on the symptoms themselves.
The next consideration is whether the belief is of delu-sional
proportions. Patients with hypochondriasis, although preoccupied, generally
acknowledge the possibility that their concerns are unfounded. Delusional
patients do not. Somatic de-lusions of serious illness are seen in some cases
of schizophrenia and in delusional disorder, somatic type. In general, patients
with schizophrenia that have such delusions also show other signs of
schizophrenia, such as disorganized speech, peculiarities of thought and
behavior, hallucinations and other delusions. Belief that an underlying illness
is being caused by some bizarre proc-ess may also be seen (e.g., “I’m trying
not to defecate because it will cause my brain to turn to jelly”).
Schizophrenic patients may also show improvement with neuroleptic treatment, at
least in the “active” symptoms of their illness, under which somatic delusions
are included.
Differentiation
from delusional disorder, somatic type, may be more difficult. It is often a
thin line between preoccupation and fear that is a conviction
and that which is a delusion. Often, the distinction is made on the basis of
whether the patient can consider the possibility that the conviction is
erroneous. Yet, patients with hypochondriasis vary in the extent to which they
can do this. DSM-IV acknowledges this by its inclusion of the specifier with
poor insight. In the past, some argued that differ-entiation could be made on
the basis of response to neuroleptics, especially pimozide; patients with
delusional disorder, but not hypochondriasis, respond.
If it is concluded that the preoccupations are not delusional, the next
consideration is whether the duration requirement of 6 months has been met (see
Figure 54.1). Syndromes of less than 6 months’ duration are diagnosed under
either somatoform dis-order NOS or adjustment disorder if the symptoms are an
abnor-mal response to a stressful life event. The reason to make such a
distinction is to distinguish hypochondriasis from transient syn-dromes, the
longitudinal course of which have been shown to be more variable, suggesting
heterogeneity.
Other diagnostic considerations include whether the pre-occupations or
fears are restricted to preoccupations with being overweight, as in anorexia
nervosa; with the inappropriateness of one’s sex characteristics, as in a
gender identity disorder; or with defects in appearance, as in body dysmorphic
disorder. The pre-occupations of hypochondriasis resemble the obsessions, and
the health checking and efforts to obtain reassurance resemble the compulsions
of obsessive–compulsive disorder. However, if such manifestations are health
centered only, obsessive–compulsive disorder is not diagnosed. If, on the other
hand, nonhealth related obsessions and compulsions are present, obsessive–compulsive
disorder may be diagnosed in addition to hypochondriasis.
Course, Natural History and Prognosis
Data are conflicting, but it appears that the most common age at onset
is in early adulthood. Available data suggest that approxi-mately 25% of patients
with a diagnosis of hypochondriasis do poorly, 65% show a chronic but
fluctuating course and 10% re-cover. This pertains to the full syndrome. A much
more variable course is seen in patients with just some hypochondriacal
con-cerns. It appears that acute onset, absence of a personality disor-der and
absence of secondary gain are favorable prognostically.
Treatment
Until recently, it appeared that patients with hypochondriasis as a
primary condition benefited, but only modestly, from psychiatric intervention.
Patients referred early for psychiatric evaluation and treatment showed a
slightly better prognosis than those continu-ing with only medical evaluations
and treatments. Of course, the first step in treatment is getting the patient
to a psychiatrist. Pa-tients with hypochondriasis generally present initially
to nonpsy-chiatric physicians and are often reluctant to see a psychiatrist.
Referral should be done sensitively, with the referring physician stressing to
the patient that his or her distress is real and that psy-chiatric evaluation
will be a supplement to, not a replacement for, continued medical care.
Initially, the generic techniques outlined for the somato-form disorders
in general should be followed. However, it has not been demonstrated that a
specific psychotherapy for hypo-chondriasis is available. Dynamic psychotherapy
is of minimal effectiveness; supportive–educative psychotherapy is only
some-what helpful, and primarily for those with syndromes of less than 3 years’
duration; and cognitive–behavioral therapy, especially response prevention of
checking rituals and reassurance seeking, is of only moderate effectiveness at
best. All of these techniques seem to lack definitive effects on
hypochondriasis itself.
Until recently, this could also be said of pharmacological approaches.
Pharmacotherapy of comorbid depressive or anxiety syndromes was often
effective, and control of such syndromes aided in general management, yet
hypochondriasis itself was not ameliorated. Although controlled trials are
lacking, anecdotal and open-label studies suggest that serotoninergic agents
such as clomipramine and the SSRI fluoxetine may be effective in amel-iorating
hypochondriasis. Similar effects are expected from the other SSRIs. Response to
fluoxetine has been reported with doses recommended for obsessive–compulsive
disorder, rather than usual antidepressant doses (i.e., 60–80 mg rather than
20–40 mg/ day). Such pharmacotherapy is best combined with the generic
psychotherapy recommendations for somatoform disorders, as well as with
cognitive–behavioral techniques to disrupt the coun-terproductive checking and
reassurance-seeking behaviors.
Related Topics