Chapter: Essentials of Psychiatry: Somatoform Disorders
Conversion Disorder
Conversion Disorder
Definition
As defined in DSM-IV, conversion disorders are characterized by symptoms
or deficits affecting voluntary motor or sensory func-tion that suggest yet are
not fully explained by a neurological or other general medical condition or the
direct effects of a substance (see Table 54.1). The diagnosis is not made if
the presentation is explained as a culturally sanctioned behavior or
experience, such as bizarre behaviors resembling a seizure during a religious
cer-emony. Symptoms are not intentionally produced or feigned, that is, the
person does not consciously contrive a symptom for exter-nal rewards, as in
malingering, or for the intrapsychic rewards of assuming the sick role, as in
factitious disorder.
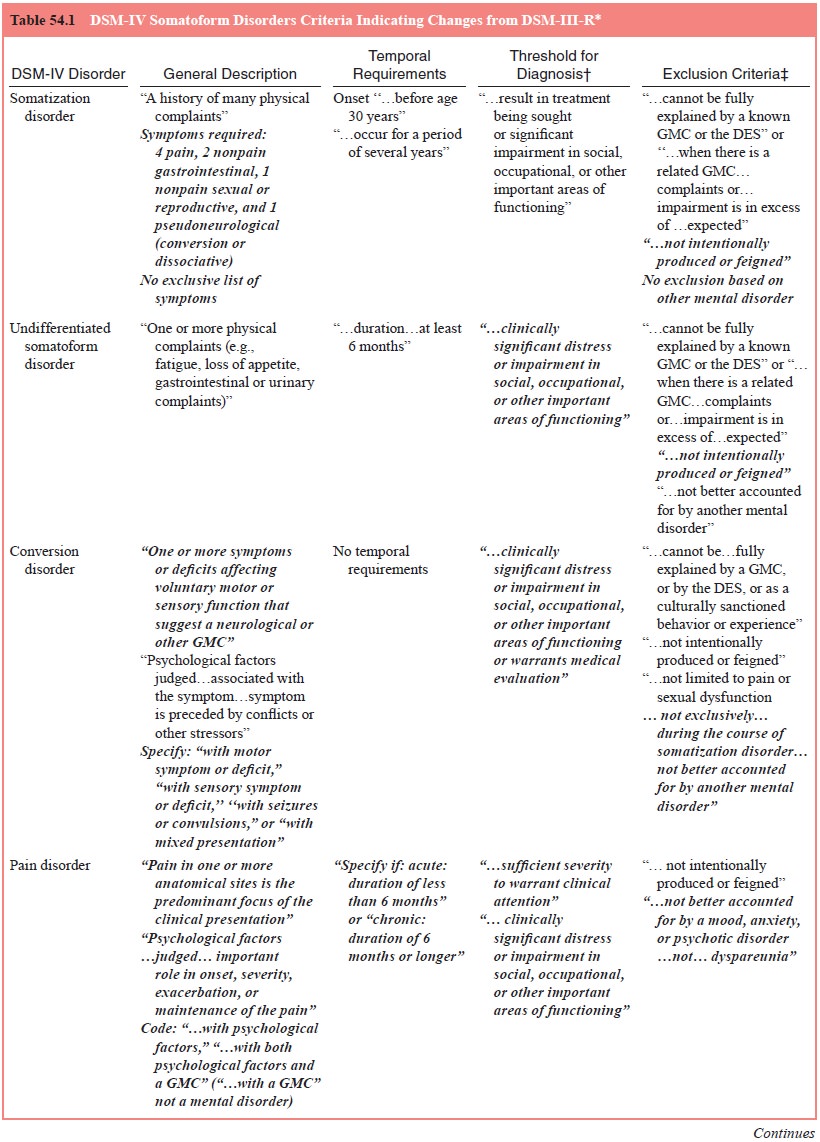
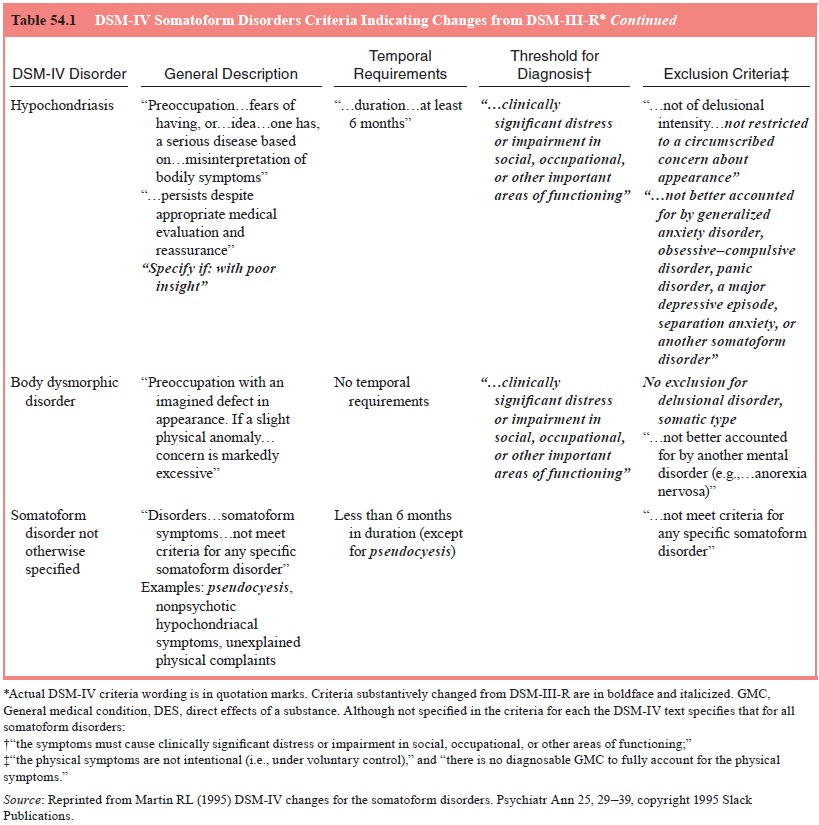
Four subtypes with specific examples of symptoms are de-fined: with
motor symptom or deficit (e.g., impaired coordination or balance, paralysis or
localized weakness, difficulty swallow-ing or lump in throat, aphonia and
urinary retention); with sen-sory symptom or deficit (e.g., loss of touch or
pain sensation, dou-ble vision, blindness, deafness and hallucinations); with
seizures or convulsions; and with mixed presentation (i.e., has symptoms of
more than one of the other subtypes). The list of examples is also contained
among the pseudoneurological symptoms listed in the diagnostic criteria for
somatization disorder. Although deter-mination is highly subjective and of
questionable reliability and validity, association with psychological factors
is required.
Whereas conversion symptoms are among the most dra-matic symptoms,
somatization disorder is characterized by mul-tiple unexplained symptoms in
many organ systems; in conver-sion disorder, even a single symptom affecting
voluntary motor or sensory function may suffice. Such nosological
inconsisten-cies have resulted in a great deal of confusion, both in research
and in clinical practice.
The relationship of conversion disorder to the dissociative disorders
warrants comment. Long recognized as related, they were subsumed as subtypes of
hysterical neurosis in DSM-II: conversion involving voluntary motor and sensory
functioning, and dissociation affecting memory and identity. DSM-IV-TR text
acknowledges the symptomatic, epidemiological and prob-able pathogenetic
similarities between conversion and dissocia-tive symptoms. Such symptoms have
been attributed to similar psychological mechanisms, and they often occur in
the same in-dividual, sometimes during the same episode of illness. DSM-IV-TR
does suggest that patients with conversion disorder be care-fully scrutinized
for dissociative symptoms.
Hallucinations are included among the sensory nervous symptoms in
DSM-IV. The concept of conversion hallucinations has a long tradition and its
inclusion as a conversion symptom was supported by the somatization disorder
field trial, in which one-third of a large sample of nonpsychotic women with
evi-dence of unexplained somatic complaints reported a history of
hallucinations. Among the 40% who had symptoms that met criteria for
somatization disorder, more than half reported hal-lucinations. Women with
other conversion symptoms were more likely to report hallucinations than were
those with no other conversion symptoms.
In general, conversion hallucinations (referred to by some as
pseudohallucinations) differ in several ways from those in psy-chotic
conditions. Conversion hallucinations typically occur in the absence of other
psychotic symptoms, insight that the halluci-nations are not real may be
retained, and they often involve more than one sensory modality, whereas
hallucinations in psychoses generally involve a single sensory modality,
usually auditory. Conversion hallucinations also often have a naive, fantastic,
or childish content, as if they are part of a fairy tale, and are de-scribed
eagerly, sometimes even provocatively, as an interesting story (e.g., “I was
driving downtown and a flying saucer flew over my car and I saw you [the
psychiatrist] in a window and I heard your voice calling to me”). They often
bear some understandable psychological purpose, although the patient may not be
aware of intent. In the example given, the “sighting” was reported at the time
that no further sessions were scheduled.
Epidemiology
Vastly different estimates of the incidence and prevalence of conversion
disorder have been reported. Much of this differencemay be attributable to
methodological differences from study to study, including the changing
definition of conversion disorder, ascertainment procedures and populations
studied. General pop-ulation estimates have generally been derived indirectly,
extrapo-lating from clinic or hospital samples.
Conversion symptoms themselves may be common; it was reported that 25%
of normal postpartum and medically ill women had a history of conversion
symptoms at some time dur-ing their life (Cloninger, 1993), yet in some
instances, there may have been no resulting clinically significant distress or
impair-ment. Lifetime prevalence rates of treated conversion symptoms in
general populations are much more modest, ranging from 11 to 500 per 100 000
(see Table 54.1). About 5 to 24% of psychiatric outpatients, 5 to 14% of
general hospital patients and 1 to 3% of outpatient psychiatric referrals reported
a history of conversion symptoms, although their current treatment was not
necessar-ily for conversion symptoms. A rate of nearly 4% of outpatient
neurological referrals and 1% of neurological admissions (Ziegler and Paul,
1954) involved conversion disorder. In virtually all studies, an excess (to the
extent of 2:1 to 10:1) of women reported conversion symptoms relative to men.
In part, this may relate to the simple fact that women seek medical evaluation
more often than men do, but it is unlikely that this fully accounts for the sex
difference. There is a predilection for lower socioeconomic status; less
educated, less psychologically sophisticated and ru-ral populations are
overrepresented. Consistent with this, higher rates (nearly 10%) of outpatient psychiatric
referrals are for con-version symptoms in “developing” countries. As countries
de-velop, there may be a declining incidence in time, which may relate to
increasing levels of education, and medical and psycho-logical sophistication.
Etiology and Pathophysiology
The term conversion implies etiology because it is derived from hypothesized
mechanism of converting psychological conflicts into somatic symptoms, often
symbolically (e.g., repressed rage is converted into paralysis of an arm that
could be used to strike). A number of psychological factors have been promoted
as part of such an etiological process, but evidence for their essential
involvement is scanty at best. Theoretically, anxiety is reduced by keeping an
internal conflict or need out of awareness by sym-bolic expression of an
unconscious wish as a conversion symp-tom (primary gain). However, individuals
with active conversion symptoms often continue to show marked anxiety,
especially on psychological tests. Symbolism is infrequently evident, and its
evaluation involves highly inferential and unreliable judgments.
Overinterpretation of symbolism in persons with occult medi-cal disorder may
contribute to misdiagnosis. Secondary gain, whereby conversion symptoms allow
avoidance of noxious ac-tivities or the procurement of otherwise unavailable
support, may also occur in persons with medical conditions, who may take
advantage of such benefits.
Individuals with conversion disorder may show a lack of concern out of
keeping with the nature or implications of the symptom (the so-called la belle indifférence). However,
indifference to symptoms is not invariably present in conversion disorder and
is also seen in individuals with general medical con-ditions, on the basis of
denial or stoicism. Conversion symptoms may present in a dramatic or histrionic
fashion and may be highly suggestible. A dramatic presentation is also seen in
distressed individuals with medical conditions. Even symptoms based on an
underlying medical condition may respond to suggestion, at leasttemporarily. In
many instances, preexisting personality disorders (in particular histrionic
personality disorder) are evident and may predispose to conversion disorder.
Persons with conversion dis-order may often have a history of disturbed
sexuality many (one-third) report a history of sexual abuse, especially
incestuous.
If not directly etiological, many psychosocial factors have been
suggested as predisposing to conversion disorder. At a minimum, many persons
with conversion disorder are in cha-otic domestic and occupational situations.
As previously men-tioned, individuals from rural backgrounds and those who are
psychologically and medically unsophisticated appear to be pre-disposed, as are
those with existing neurological disorders. In the last case, a tendency to
conversion symptoms has been attrib-uted to “modeling”, that is, patients with
neurological disorders are likely to have observed in others, as well as in
themselves, various neurological symptoms, which they then may simulate as
conversion symptoms.
Available data suggest a genetic contribution. Conver-sion symptoms are
more frequent in relatives of individuals with conversion disorder. In a
nonblinded study, rates of conversion disorder were found to be elevated
tenfold in female (fivefold in male) relatives of patients with conversion
disorder. Nongenetic familial factors, particularly incestuous childhood sexual
abuse, may also be involved in some. Nearly one-third of individuals with
medically unexplained seizures reported childhood sex-ual abuse, compared with
less than 10% of those with complex partial epilepsy.
Diagnosis and Differential Diagnosis
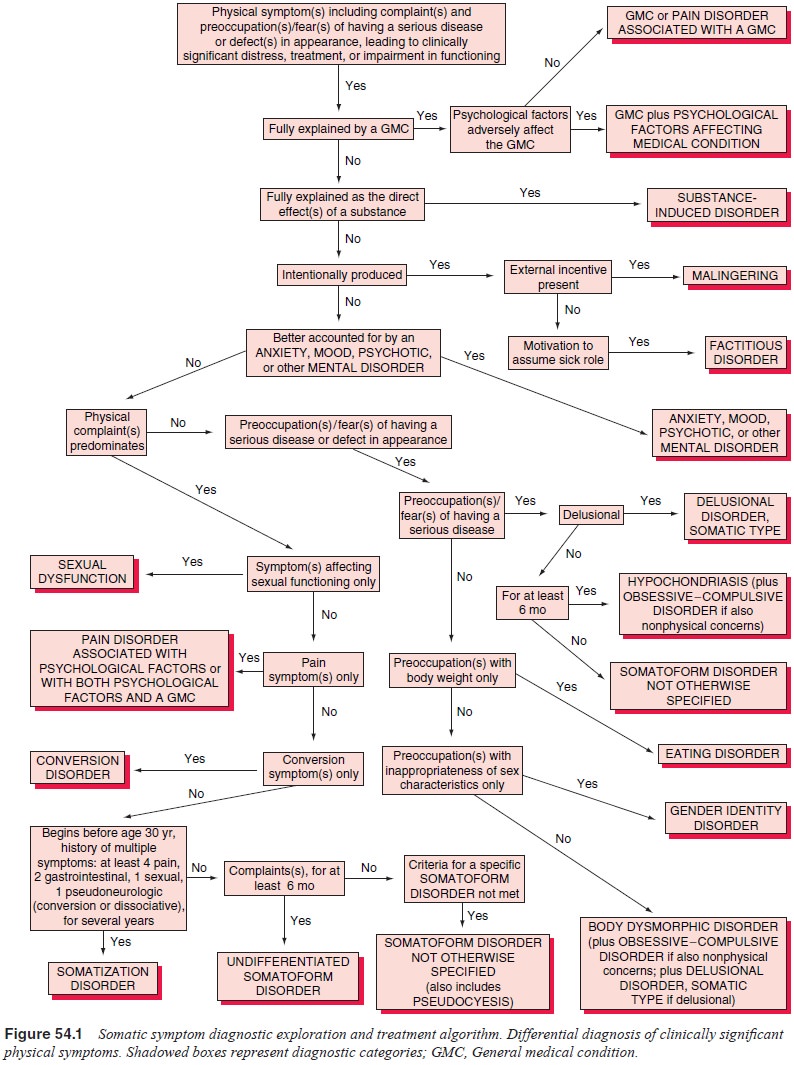
As shown in Figure 54.1, the first consideration is whether the
conversion symptoms are explained on the basis of a general medical condition.
Because conversion symptoms by definition affect voluntary motor or sensory
function (thus pseudoneuro-logical), neurological conditions are usually
suggested, but other general medical conditions may be implicated as well.
Neurolo-gists are generally first consulted by primary care physicians for
conversion symptoms; psychiatrists become involved only after neurological or
general medical conditions have been reasonably excluded. Nonetheless,
psychiatrists should have a good appre-ciation of the process of making such
exclusions. More than 13% of actual neurological cases are diagnosed as
functional before the elucidation of a neurological illness (Perkin, 1989).
Even after referral, vigilance for an emerging general medical condi-tion should
continue. A significant percentage – 21 to 50% – of patients diagnosed with
conversion symptoms are found to have neurological illness on follow-up.
Apparent
conversion symptoms mandate a thorough eval-uation for possible underlying
physical explanation. This evalua-tion must include a thorough medical history;
physical (especially neurological) examination; and radiographical, blood,
urine and other tests as clinically indicated. Reliance should not be placed on
determination of whether psychological factors explain the symptom. Such
determinations are unreliable except, perhaps, in cases in which there is a
clear and immediate temporal rela-tionship between a psychosocial stressor and
the symptom, or in cases in which similar situations led to conversion symptoms
in the past. A history of previous conversion or other unexplained symptoms,
particularly if somatization disorder is diagnosable, lessens the probability
that an occult medical condition will be identified. Although conversion
symptoms may occur at any age, symptoms are most often first manifested in late
adolescence or early adulthood. Conversion symptoms first occurring in middle age or later should increase suspicion of an occult physical illness.
Symptoms of many neurological illnesses may appear in-consistent with
known neurophysiological or neuropathological processes, suggesting conversion
and posing diagnostic prob-lems. These illnesses include multiple sclerosis, in
which blind-ness due to optic neuritis may initially present with normal fundi;
myasthenia gravis, periodic paralysis, myoglobinuric myopathy, polymyositis and
other acquired myopathies, in which marked weakness in the presence of normal
deep tendon reflexes may occur; and Guillain–Barré syndrome, in which early
extremity weakness may be inconsistent.
Complicating diagnosis is the fact that physical illness and conversion
or other apparent psychiatric overlay are not mutually exclusive. Patients with
physical illnesses that are incapacitating and frightening may appear to be
exaggerating symptoms. Also, patients with actual neurological illness will
also have “pseudo” symptoms. For example, patients with actual seizures may
have pseudoseizures as well. Considering these observations, psychia-trists
should avoid a rash and hasty diagnosis of conversion disor-der when faced with
symptoms that are difficult to interpret.
As with the other somatoform disorders, symptoms of conversion disorder
are not intentionally produced, in distinc-tion to malingering or factitious
disorder. To a large part, this determination is based on assessment of the
motivation for exter-nal rewards (as in malingering) or for the assumption of
the sick role (as in factitious disorder). The setting is often an important
consideration. For example, conversion-like symptoms are fre-quent in military
or forensic settings, in which obvious potential rewards make malingering a
serious consideration.
A diagnosis of conversion disorder should not be made if a conversion
symptom is fully accounted for by a mood disorder or by schizophrenia (e.g.,
disordered motility as part of a cata-tonic syndrome of a psychotic mood
disorder or schizophrenia). If the symptom is a hallucination, it must be
remembered that the descriptors differentiating conversion from psychotic
hallu-cinations should be seen only as rules of thumb. Differentiation should
be based on a comprehensive assessment of the illness. In the case of
hallucinations, post traumatic stress disorder and dis-sociative identity
disorder (multiple personality disorder) must also be excluded. If the
conversion symptom cannot be fully ac-counted for by the other psychiatric
illness, conversion disorder should be diagnosed in addition to the other
disorder if it meets criteria (e.g., an episode of unexplained blindness in a
patient with a major depressive episode). In hypochondriasis, neurologi-cal
illness may be feared (“I have strange feelings in my head; it must be a brain
tumor”), but the focus here is on preoccupation with fear of having the illness
rather than on the symptom itself as in conversion disorder.
By definition, if symptoms are limited to sexual dysfunc-tion or pain,
conversion disorder is not diagnosed. Criteria for so-matization disorder
require multiple symptoms in multiple organ systems and functions, including
symptoms affecting motor or sensory function (conversion symptoms) or memory or
identity (dissociative symptoms). Thus, it would be superfluous to make an
additional diagnosis of conversion disorder in the context of a somatization
disorder.
A last consideration is whether the symptom is a culturally sanctioned
behavior or experience. Conversion disorder should not be diagnosed if symptoms
are clearly sanctioned or even ex-pected, are appropriate to the sociocultural
context, and are not associated with distress or impairment. Seizure-like
episodes, such as those that occur in conjunction with certain religious
ceremonies, and culturally expected responses, such as women “swooning” in
response to excitement in Victorian times, qualify as examples of these
symptoms.
Course, Natural History and Prognosis
Age at onset is typically from late childhood to early adulthood. Onset
is rare before the age of 10 years and after 35 years, but cases with an onset
as late as the ninth decade have been reported. The likelihood of a
neurological or other medical condition is increased when the age at onset is
in middle or late life. Develop-ment is generally acute, but symptoms may
develop gradually as well. The course of individual conversion symptoms is
generally short; half to nearly all symptoms remit by the time of hospital
discharge. However, symptoms relapse within 1 year in one-fifth to one-fourth
of patients. Typically, one symptom is present in a single episode, but
multiple symptoms are generally involved longitudinally. Factors associated
with good prognosis include acute onset, clearly identifiable precipitants, a
short interval be-tween onset and institution of treatment, and good
intelligence. Conversion blindness, aphonia and paralysis are associated with
relatively good prognosis, whereas patients with seizures and tremor do more
poorly. Some patients diagnosed initially with conversion disorder will have a
presentation that meets criteria for somatization disorder when they are
observed longitudinally.
Individual conversion symptoms are generally self-limited and do not
lead to physical changes or disabilities. Rarely, physi-cal sequelae such as
atrophy may occur. Marital and occupational problems are not as frequent in
patients with conversion disorder as they are in those with somatization
disorder.
Treatment
Reports of the treatment of conversion disorder date from those of
Charcot, which generally involved symptom removal by sug-gestion or hypnosis.
Breuer and Freud, using such psychoana-lytic techniques as free association and
abreaction of repressed affects, had more ambitious objectives in their
treatment of Anna O, including the resolution of unconscious conflicts. To
date, whereas some recommend long-term, intensive, insight-oriented
psychodynamic psychotherapy in pursuit of such goals, most psychiatrists
advocate a more pragmatic approach, espe-cially for acute cases.
Therapeutic approaches vary according to whether the conversion symptom
is acute or chronic. Whichever the case, di-rect confrontation is not
recommended. Such a communication may cause a patient to feel even more
isolated. An undiscovered physical illness may also underlie the presentation.
In acute cases, the most frequent initial aim is removal of the symptom.
The pressure behind accomplishing this de-pends on the distress and disability
associated with the symptom (Ford, 1995). If the patient is not in great
distress and the need to regain function is not immediate, a conservative
approach of re-assurance, relaxation and suggestion is recommended. With this
technique, the patient is reassured that on the basis of evaluation the symptom
will disappear completely and, in fact, is already be-ginning to do so. The
patient can then be encouraged to ventilate about recent events and feelings,
without any causal relationships being suggested. This is in contrast to
attempts at abreaction, by which repressed material, particularly regarding a
painful experience or a conflict, is brought back to consciousness.
If symptoms do not resolve with such conservative ap-proaches, a number
of other techniques for symptom resolu-tion may be instituted. It does
appear that prompt resolution of conversion symptoms is important because the
duration of con-version symptoms is associated with a greater risk of
recurrence and chronic disability. The other techniques include narcoanalysis
(e.g., amobarbital interview), hypnosis and behavioral therapy. In
narcoanalysis, amobarbital or another sedative–hypnotic medi-cation such as
lorazepam is given intravenously to the point of drowsiness. Sometimes this is
followed by administration of a stimulant medication, such as methamphetamine.
The patient is then encouraged to discuss stressors and conflicts. This
tech-nique may be effective acutely, leading to at least temporary symptom
relief as well as expansion of the information known about the patient. This
technique has not been shown to be especially effective with more chronic
conversion symptoms. In hypnotherapy, symptoms may be removed with the
suggestion that the symptoms will gradually improve posthypnotically.
Infor-mation regarding stressors and conflicts may be explored as well. Formal
behavioral therapy, including relaxation training and even aversive therapy,
has been proposed and reported by some to be ef-fective. In addition, simply
manipulating the environment to inter-rupt reinforcement of the conversion
symptom is recommended.
Anecdotally, somatic treatments including phenothiazines, lithium and
electroconvulsive therapy have been reported effec-tive. However, in many
cases, this may be attributable to sim-ple suggestion. In other cases,
resolution of another psychiatric disorder, such as a psychotic disorder or a
mood disorder, may have led to the symptom’s removal. It should be evident from
the preceding discussion that in acute conversion disorders, it may be not the
particular technique but the influence of suggestion that is specifically
associated with symptom relief. It is likely that in various rituals, such as
exorcism and other religious ceremonies, immediate “cures” are based on
suggestion. Suggestion seems to play a major role in the resolution of “mass
hysteria”, in which a group of individuals who believe that they have been
exposed to some noxious influence such as a “toxin” or even a “spell”
expe-rience similar symptoms that do not appear to have any organic basis.
Often, the epidemic can be contained if affected individu-als are segregated.
Simple announcements that no such factor has been identified and that symptoms
experienced by the group have been linked to mass hysteria have been effective.
Thus far, this discussion has centered on acute treatment primarily for
symptom removal. Longer-term approaches include strategies previously discussed
for somatization disorder – a pragmatic, conservative approach involving
support and explo-ration of various conflict areas, particularly of
interpersonal re-lationships. A certain degree of insight may be attained, at
least in terms of appreciating relationships between various conflicts and
stressors and the development of symptoms. Others advocate long-term,
intensive, insight-oriented dynamic psychotherapy.
Related Topics