Chapter: Essentials of Psychiatry: Somatoform Disorders
Somatization disorder: Course, Natural History and Prognosis
Course, Natural History and Prognosis
Somatization disorder is rare in children younger than 9 years of age.
Characteristic symptoms of somatization disorder usually begin during
adolescence, and the criteria are met by the mid-twenties. Somatization
disorder is a chronic illness characterized by fluctuations in the frequency
and diversity of symptoms. Full remissions occur rarely, if ever. Whereas the
most active sympto-matic phase is in early adulthood, aging does not appear to
lead to total remission. Pribor and colleagues (1994) found that women with
somatization disorder older than 55 years did not differ from younger
somatization patients in the number of somatic symp-toms. Longitudinal
follow-up studies have confirmed that 80 to 90% of patients initially diagnosed
with somatization disorder will maintain a consistent clinical picture and be
rediagnosed similarly after 6 to 8 years. Women with somatization disorder seen
in psychiatric settings are at increased risk for attempted suicide, although
such attempts are usually unsuccessful and may reflect manipulative gestures
more than intent to die. It is not clear whether such risk is true for patients
with somatization disorder seen only in general medical settings.
Treatment
First, a “management” rather than a “curative” strategy is rec-ommended
for somatization disorder. With the current absence of an identified definitive
treatment, a modest, practical, em-pirical approach should be taken. This
should include efforts to minimize distress and functional impairments
associated with the multiple somatic complaints; to avoid unwarranted
diagnos-tic and therapeutic procedures and medications; and to prevent
potential complications including chronic invalidism and drug dependence.
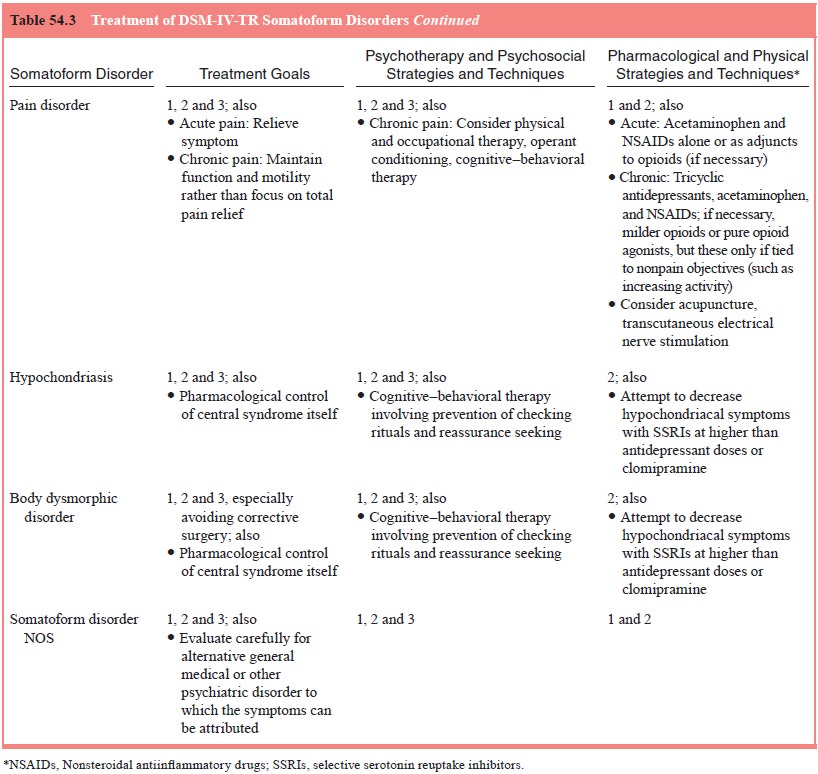
In such regard, the general recommendations outlined for somatoform
disorders should be followed (see Table 54.3). The patient should be encouraged
to see a single physician with an understanding of and, preferably, experience
in treating somatization disorder. This helps limit the number of unneces-sary
evaluations and treatments. Most clinicians advocate rou-tine, brief,
supportive office visits scheduled at regular intervals to provide reassurance
and prevent patients from “needing to develop” symptoms to obtain care and
attention. This “medical” management can well be provided by a primary care
physician, perhaps with consultation with a psychiatrist. The study by Smith
and colleagues (1986) demonstrated that such a regimen led to markedly
decreased health care costs, with no apparent decre-ments in health or
satisfaction of patients.
The foundations of treatment for this disorder are: 1) es-tablishment of
a strong physician–patient relationship or bond; 2) education of the patient
regarding the nature of the psychiatric condition; and 3) provision of support
and reassurance.
The first component, establishing a strong therapeutic bond, is
important in the treatment of somatization disorder. Without it, it will be
difficult for the patient to overcome skepti-cism deriving from past experience
with many physicians and other therapists who “never seemed to help”. In
addition, trust must be strong enough to withstand the stress of withholding
unwarranted diagnostic and therapeutic procedures that the pa-tient may feel
are indicated. The cornerstone of establishing a therapeutic relationship is
laid when the psychiatrist indicates an understanding of the patient’s pain and
suffering, legitimizing the symptoms as real. This demonstrates a willingness
to provide direct compassionate assistance. A full investigation of the
medi-cal and psychosocial histories, including extensive record review, will
illustrate to patients the willingness of the psychiatrist to gain the fullest
understanding of them and their plight. This also provides another opportunity
to evaluate for the presence of an underlying medical disorder and to obtain a
fuller picture of psychosocial difficulties that may relate temporally to
somatic symptoms.
Only after the diagnosis has been clearly established and the
therapeutic alliance is firmly in place can the psychiatrist confidently limit
diagnostic evaluations and therapies to those performed on the basis of
objective findings as opposed to merely subjective complaints. Of course, the
psychiatrist should remain aware that patients with somatization disorder are
still at risk for development of general medical illnesses so that a vigilant
per-spective should always be maintained.
The second component is education. This involves advis-ing patients that
they suffer from a “medically sanctioned ill-ness”, that is, a condition
recognized by the medical community and one about which a good deal is known.
Ultimately, it may be possible to introduce the concept of somatization
disorder, which can be described in a positive light (i.e., the patient does
not have a progressive, deteriorating, or potentially fatal medical disorder,
and the patient is not “going crazy” but has a condition by which many symptoms
will be experienced). A realistic discussion of prognosis and treatment options
can then follow.
The third component is reassurance. Patients with soma-tization disorder
often have control and insecurity issues, which often come to the forefront
when they perceive that a particular physical complaint is not being adequately
addressed. Explicit reassurance should be given that the appropriate inquiries
and investigations are being performed and that the possibility of an
underlying physical disorder as the explanation for symptoms is being
reasonably considered.
In time, it may be appropriate gradually to shift emphasis away from
somatic symptoms to consideration of personal and interpersonal issues. In some
patients, it may be appropriate toposit a causal theory between somatic
symptoms and “stress”, that is, that there may be a temporal association
between symp-toms and personal, interpersonal and even occupational prob-lems.
In patients for whom such “insight” is difficult, behavioral techniques may be
useful.
Even following such therapeutic guidelines, patients with somatization
disorder are often difficult to treat. Attention-seek-ing behavior, demands and
manipulation are common, necessi-tating firm limits and careful attention to
boundary issues. This, again, is a management rather than a curative approach.
Thus, such behaviors should generally be dealt with directively rather than
interpreted to the patient.
Pharmacological and Other Somatic Treatments
No effective somatic treatments for somatization disorder itself have
been identified.
Patients with somatization disorder may complain of anxi-ety and
depression, suggesting readily treatable comorbid psy-chiatric disorders. As
previously discussed, it is often difficult to distinguish actual comorbid
conditions from aspects of somato-form disorder itself. Pharmacological
interventions are likely to be helpful in the former but not in the latter. At
times, such discrimination will be impossible, and an empirical trial of such
treatments may be indicated. Patients with somatization disor-der are often
inconsistent and erratic in their use of medications. They will often report
unusual side effects that may not be ex-plained pharmacologically. This makes
evaluation of treatment response difficult. In addition, drug dependence and
suicide ges-tures and attempts are not uncommon.
Related Topics