Chapter: Essentials of Psychiatry: Somatoform Disorders
Body Dysmorphic Disorder
Body Dysmorphic Disorder
Definition
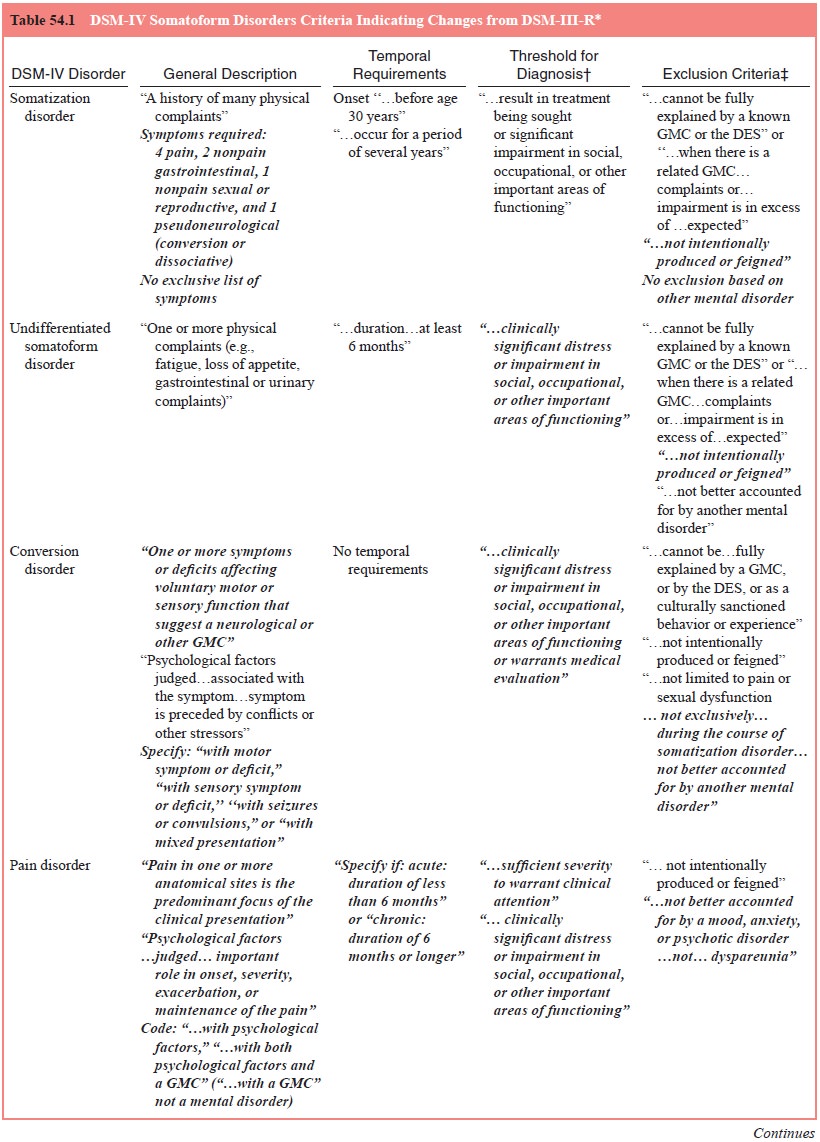
The essential feature of this disorder is preoccupation with an imagined
defect in appearance or a markedly excessive concern with a minor anomaly (see
Table 54.1). In body dysmorphic dis-order, a person could be preoccupied with
an imagined defect while she or he actually had some other anomaly and was not
normal appearing. To exclude conditions with trivial or minor symptoms, the
preoccupation must cause clinically significant distress or impairment. By
definition, body dysmorphic disorder is not diagnosed if symptoms are limited
to preoccupation with body weight, as in anorexia nervosa or bulimia nervosa,
or to perceived inappropriateness of sex characteristics, as in gender identity
disorder.
Preoccupations most often involve the nose, ears, face, or sexual
organs. Common complaints include a diversity of imag-ined flaws of the face or
head, including defects in the hair (e.g., too much or too little), skin (e.g.,
blemishes), and shape or sym-metry of the face or facial features (e.g., nose
is too large and deformed). However, any body part may be the focus, including
genitals, breasts, buttocks, extremities, shoulders and even over-all body
size.
Body dysmorphic disorder has been well described in the European and
Japanese literature, generally designated dys-morphophobia, often under the
rubric of the monosymptomatic hypochondriacal psychoses. Until recently, it had
been virtually ignored in the US literature as well as clinically.
The definition of the disorder was reexamined for DSM-IV on several
counts, but especially as to its relationship to other psychiatric disorders
(Phillips and Hollander, 1996). After much deliberation, it was determined that
body dysmorphic disorder, although often comorbid with anxiety and mood
disorders, was sufficiently discrete to be maintained as a separate disorder.
As discussed in the differential diagnosis section, it can be distin-guished
from depressive disorders and from most anxiety dis-orders, although it
resembles obsessive–compulsive disorder in phenomenology, course and even
response to treatment. It was also decided to keep it with the somatoform
disorders grouping, although it does not share much with the other disorders in
this grouping (with the exception of hypochondriasis), beyond the fact that
affected patients are generally referred to psychiatrists from other physicians
and that they also present with medically unexplained physical complaints
(defects in appearance in body dysmorphic disorder).
As De Leon and colleagues (1989) pointed out, it is ex-tremely difficult
to determine whether a dysmorphic concern is delusional as in that with body
dysmorphic disorder, for a continuum exists from clearly nondelusional
preoccupations to unequivocal delusions such that defining a discrete boundary
between the two ends of the spectrum would be artificial. Fur-thermore,
individual patients seem to move back and forth along this continuum. Support
for rejecting the exclusion is prelimi-nary evidence that dysmorphic
preoccupations may respond to the same pharmacotherapy (SSRIs), regardless of
whether the concerns are delusional. Perhaps as a reflection of the state of
knowledge at this point, both body dysmorphic disorder and de-lusional
disorder, somatic type, can be diagnosed on the basis of the same symptoms, in
the same individual, at the same time. Thus, the definition of body dysmorphic
disorder differs from hypochondriasis, which is not diagnosed if
hypochondriacal concerns are determined to be delusional.
Epidemiology
Knowledge of such parameters is still incomplete. In general, patients
with body dysmorphic disorder first present to nonpsy-chiatrists such as
plastic surgeons, dermatologists and internists because of the nature of their
complaints and are not seen psy-chiatrically until they are referred (De Leon et al., 1989). Many resist or refuse
referral because they do not see their problem as psychiatric; thus, study of
psychiatric clinic populations may un-derestimate the prevalence of the
disorder. It has been estimated that 2% of patients seeking corrective cosmetic
surgery suffer from this disorder. Although women outnumber men in this
pop-ulation, it is not known whether this sex distribution holds true in the
general population.
Etiology and Pathophysiology
A number of sociological, psychological and neurobiological theories
have been proposed. Body dysmorphic disorder has been explained, at least in
part, as an exaggerated incorporation of societal ideals of physical perfection
and acceptance of cos-metic plastic surgery to attain such goals. A high
frequency of insecure, sensitive, obsessional, schizoid, anxious, narcissistic,
introverted and hypochondriacal personality traits in body dys-morphic patients
have been described (Phillips, 1991). Various psychodynamic mechanisms and
symbolic meanings of dysmor-phic symptoms have been suggested (Phillips, 1991),
going back to Freud’s case of the Wolfman who had dysmorphic preoccupa-tions
regarding his nose.
Some interesting neurobiological possibilities have emerged,
particularly concerning observations that hypochon-driasis, body dysmorphic
disorder and a number of other con-ditions involving compelling repetitive
thoughts or behaviors may respond preferentially to SSRIs, not to other
antidepressant drugs. An obsessive–compulsive spectrum disorders grouping, the
pathological process of which is mediated by serotoninergic dysregulation, has
been suggested. As further evidence, symp-toms of body dysmorphic disorder as
well as those of obsessive– compulsive disorder may be aggravated by the
partial serotonin agonist m-chlorophenylpiperazine.
Diagnosis and Differential Diagnosis
The preoccupations of body dysmorphic disorder must first be
differentiated from usual concerns with grooming and appear- ance. Attention to
appearance and grooming is universal and socially sanctioned. However,
diagnosis of body dysmorphic disorder requires that the preoccupation cause
clinically sig-nificant distress or impairment. In addition, in body
dysmor-phic disorder, concerns focus on an imaginary or exaggerated defect,
often of something, such as a small blemish, that would warrant scant attention
even if it were present. Persons with histrionic personality disorder may be
vain and excessively concerned with appearance. However, the focus in this
disor-der is on maintaining a good or even exceptional appearance, rather than
preoccupation with a defect. Such concerns are probably unrelated to body
dysmorphic disorder. In addition, by nature, the preoccupations in body
dysmorphic disorder are essentially unamenable to reassurance from friends or
fam-ily or consultation with physicians, cosmetologists, or other
professionals.
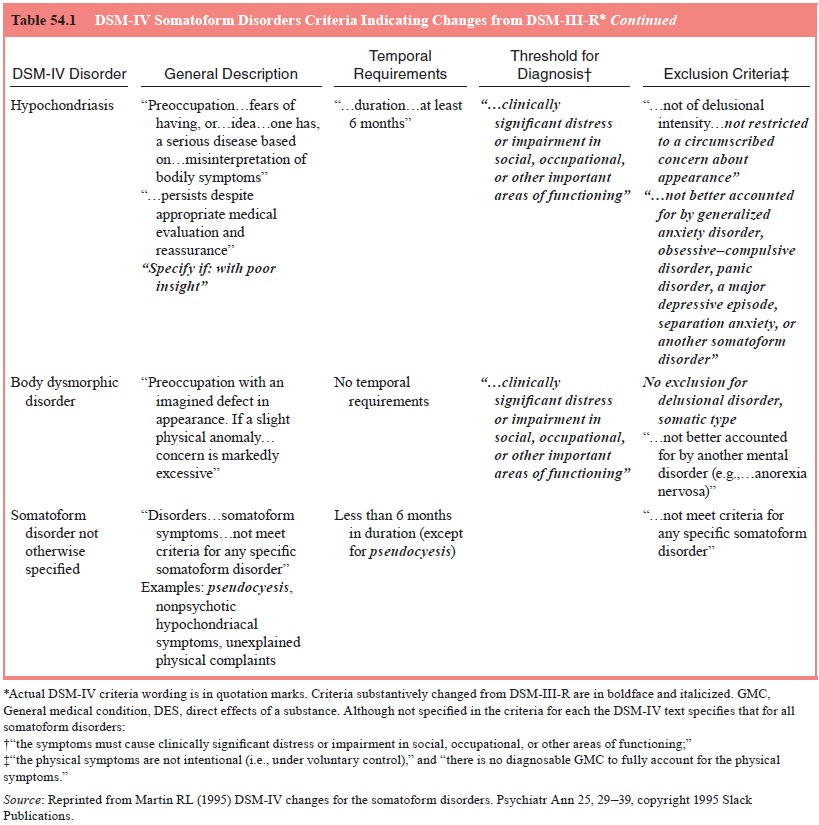
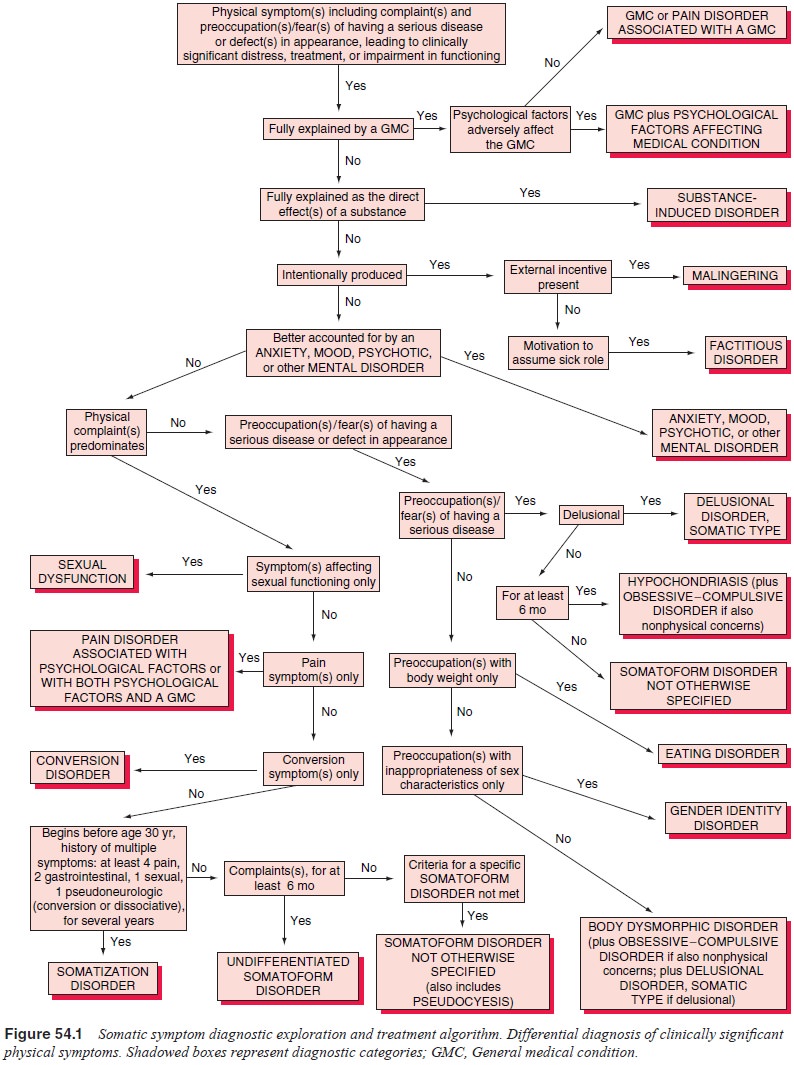
Next, the possibility of an explanation by a general medi-cal condition
must be considered (see Figure 54.1). As mentioned, patients with this disorder
often first present to plastic surgeons, oral surgeons and others, seeking
correction of defects. By the time a mental health professional is consulted,
it has generally been ascertained that there is no physical basis for the
degree of concern. As with other syndromes involving somatic preoccupa-tions
(or delusions), such as olfactory reference syndrome and delusional parasitosis
(both included under delusional disorder, somatic type), occult medical
disorders, such as an endocrine dis-turbance or a brain tumor, must be
excluded.
In terms of explanation on the basis of another psychi-atric disorder,
there is little likelihood that symptoms of body dysmorphic disorder will be
intentionally produced as in ma-lingering or factitious disorder. Unlike in
other somatoform disorders, such as pain, conversion and somatization disor-ders,
preoccupation with appearance predominates. Somatic preoccupations may occur as
part of an anxiety or mood disor-der. However, these preoccupations are
generally not the pre-dominant focus and lack the specificity of dysmorphic
symp-toms. Because patients with body dysmorphic disorder often become
isolative, social phobia may be suspected. However, in social phobia, the
person may feel self-conscious gener-ally but will not focus on a specific
imagined defect. Indeed, the two conditions may coexist, warranting both
diagnoses. Diagnostic problems may present with the mood-congruent ruminations
of major depression, which sometimes involve concern with an unattractive
appearance in association with poor self-esteem. Such preoccupations generally
lack the fo-cus on a particular body part that is seen in body dysmorphic
disorder. On the other hand, patients with body dysmorphic disorder commonly
have dysphoric affects described by them variously as anxiety or depression. In
some cases, these affects can be subsumed under body dysmorphic disorder; but
in other instances, comorbid diagnoses of anxiety or mood disorders are
warranted.
Differentiation from schizophrenia must also be made. At times, a
dysmorphic concern will seem so unusual that such a psychosis may be
considered. Furthermore, patients with this disorder may show ideas of
reference in regard to defects in their appearance, which may lead to the
consideration of schizophre-nia. However, other bizarre delusions, particularly
of persecu-tion or grandiosity, and prominent hallucinations are not seen in
body dysmorphic disorder. From the other perspective, schizo-phrenia with
somatic delusions generally lacks the focus on a particular body part and
defect. Also in schizophrenia, bizarre interpretations and explanations for
symptoms are often present, such as “this blemish was a sign from Jesus that I
am to pro-tect the world from Satan”. Other signs of schizophrenia, such as
hallucinations and disorganization of thought, are also absent in body dysmorphic
disorder. As previously mentioned, the preoc-cupations in body dysmorphic
disorder appear to be on a con-tinuum from full insight to delusional intensity
whereby the pa-tient cannot even consider the possibility that the
preoccupation is groundless. In such instances, both body dysmorphic disorder
and delusional disorder, somatic type, are to be diagnosed.
Body dysmorphic disorder is not to be diagnosed if the con-cern with
appearance is better accounted for by another psychiat-ric disorder. Anorexia nervosa,
in which there is dissatisfaction with body shape and size, is specifically
mentioned in the crite-ria as an example of such an exclusion. Although not
specifically mentioned in DSM-IV, if a preoccupation is limited to discomfort
or a sense of inappropriateness of one’s primary and secondary sex
characteristics, coupled with a strong and persistent cross-gender
identification, body dysmorphic disorder is not diagnosed.
The preoccupations of body dysmorphic disorder may resemble obsessions
and ruminations as seen in obsessive– compulsive disorder. Unlike the
obsessions of obsessive–com-pulsive disorder, the preoccupations of body
dysmorphic disor-der focus on concerns with appearance. Compulsions are limited
to checking and investigating the perceived physical defect and attempting to
obtain reassurance from others regarding it. Still, the phenomenology is
similar, and the two disorders are often comorbid. If additional obsessions and
compulsions not related to the defect are present, obsessive–compulsive
disorder can be diagnosed in addition to body dysmorphic disorder.
Course, Natural History and Prognosis
Age at onset appears to peak in adolescence or early adulthood. Body
dysmorphic disorder is generally a chronic condition, with a waxing and waning
of intensity but rarely full remission. In a lifetime, multiple preoccupations
are typical; in one study, the average was four (Phillips et al., 1993). In some, the same preoc-cupation remains unchanged.
In others, new perceived defects are added to the original ones. In others
still, symptoms remit, only to be replaced by others. The disorder is often
highly in-capacitating, with many patients showing marked impairment in social
and occupational activities. Perhaps a third becomes housebound. Most attribute
their limitations to embarrassment concerning their perceived defect, but the
attention and time-consuming nature of the preoccupations and attempts to
inves-tigate and rectify defects also contribute. The extent to which patients
with body dysmorphic disorder receive surgery or medi-cal treatments is
unknown. Superimposed depressive episodes are common, as are suicidal ideation
and suicide attempts. Actual suicide risk is unknown.
In view of the nature of the defects with which patients are preoccupied,
it is not surprising that they are found most com-monly among patients seeking
cosmetic surgery. Preoccupations persist despite reassurance that there is no
defect to correct surgi-cally. Surgery or other corrective procedures rarely if
ever lead to satisfaction and may even lead to greater distress with the
per-ception of new defects attributed to the surgery.
Treatment
First, the generic goals and treatments as outlined for the so-matoform
disorders overall should be instituted. These are beneficial in interrupting an
unending procession of repeated evaluations and the possibility of needless
surgery, which may lead to additional perceptions that surgery has resulted in
fur-ther disfigurement.
Traditional insight-oriented therapies have not generally proved to be
effective. Results with traditional behavioral tech-niques, such as systematic
desensitization and exposure therapy, have been mixed. At least without
amelioration with effective pharmacotherapy, the preoccupations do not
extinguish as would be expected with phobias. A cognitive–behavioral approach
similar to what was recommended for hypochondriasis may be more effective. This
includes response prevention techniques whereby the patient is not permitted
repetitively to check the perceived defect in mirrors. In addition, patients
are advised not to seek reassurance from family and friends, and these persons
are instructed not to respond to such inquiries. Some patients adopt such
behaviors spontaneously, avoiding mirrors and other reflecting surfaces,
refusing even to allude to their perceived de-fects to others. Such
“self-techniques” may be encouraged and refined.
Biological treatments have long been used but until re-cently were of
limited benefit to patients with body dysmorphic disorder. Approaches have
included electroconvulsive therapy, tricyclic and MAOI antidepressants, and
neuroleptics, particu-larly pimozide. In most reports of positive response to
tricyclic or MAOI antidepressant drugs, it is unclear whether response was
truly in terms of the dysmorphic syndrome or simply represented improvement in
comorbid depressive or anxiety syndromes. Re-sponse to neuroleptic treatment
has been suggested as a diagnos-tic test to distinguish body dysmorphic
disorder from delusional disorder, somatic type. The delusional syndromes often
respond to neuroleptics; body dysmorphic disorders, even when the body
preoccupations are psychotic, generally do not. Pimozide has been singled out
as a neuroleptic with specific effectiveness for somatic delusions, but this
specificity does not appear to apply to body dysmorphic disorder.
An exception to this uninspiring picture is the observa-tion of a
possible preferential response to antidepressant drugs with serotonin reuptake
blocking effects, such as clomipramine, or SSRIs, such as fluoxetine and
fluvoxamine (Hollander et al., 1992).
Phillips and coworkers (1993) reported that more than 50% of patients with body
dysmorphic disorder showed a partial or complete remission with either
clomipramine or fluoxetine, a response not predicted on the basis of coexisting
major depres-sive or obsessive–compulsive disorder. As with hypochondria-sis,
effectiveness is generally achieved at levels recommended for
obsessive–compulsive disorder rather than for depression (e.g., 60–80 mg rather
than 20–40 mg/day of fluoxetine). The SSRIs appear to ameliorate delusional as
well as nondelusional dysmorphic preoccupations. Successful augmentation of
clomi-pramine or SSRI therapy has been suggested with buspirone, another drug with
serotoninergic effects. Neuroleptics, particu-larly pimozide, may also be
helpful adjuncts, particularly if de-lusions of reference are present. Little
seems to be gained with the addition of anticonvulsants, or benzodiazepines to
the SSRI therapy.
As yet, rigorous studies have not been conducted, but anecdotal
observations and open-label studies show promise for effective treatment with
SSRIs and other serotoninergic agents for this, until now, therapeutically
exasperating disor-der. If such approaches fulfill their initial promise,
integratedapproaches using pharmacotherapy and other modalities such as
cognitive–behavioral therapy may provide effective treat-ment options.
Related Topics