Chapter: Essentials of Psychiatry: Somatoform Disorders
Pain Disorder
Pain Disorder
Definition
As defined in DSM-IV, the essential feature of pain disorder is pain
with which psychological factors “have an important role in the onset,
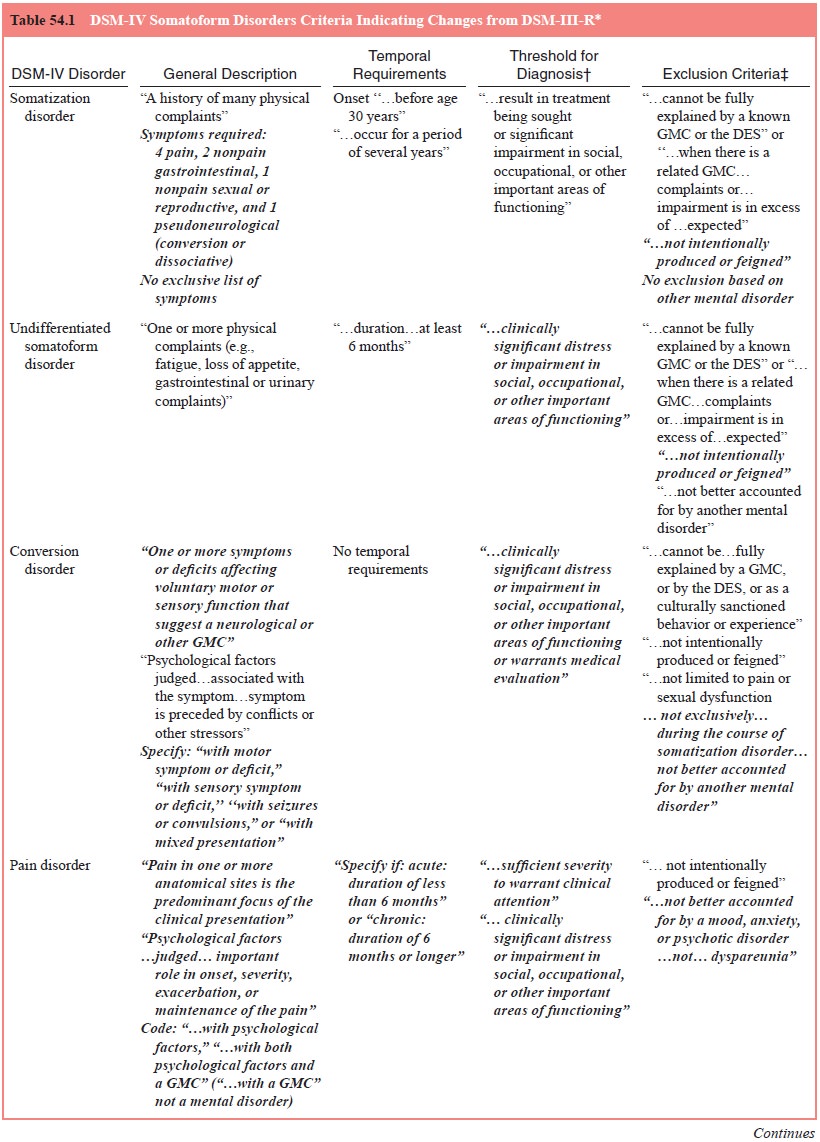
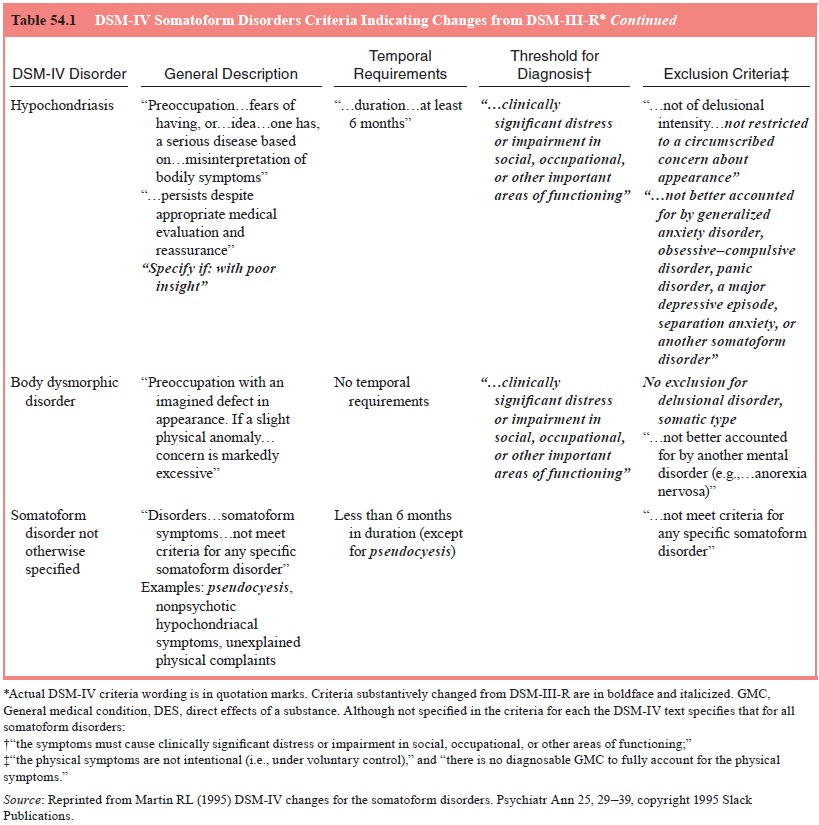
severity, exacerbation, or maintenance” (see Table 54.1). Pain disorder is
subtyped as pain disorder associated with psychological factors and pain
disorder associated with both psycho-logical factors and a general medical
condition. The third possibility, pain disorder associated with a general
medical condition, is not con-sidered to be a mental disorder, because the
requirement is not met that psychological factors play an important role. Thus,
the DSM-IV concept of pain disorder allows the psychiatrist greater specifi-city
in considering etiological factors and a more useful schema for differential
diagnosis. The focus is placed on the presence of psychological factors rather
than the exasperating determination of whether the pain is attributable to
organic disease.
In addition, DSM-IV requires that pain be the predominant focus of the
clinical presentation and that it cause clinically sig-nificant distress or
impairment. Specifiers of acute (duration of less than 6 months) and chronic
(duration of 6 months or longer) are provided.
Epidemiology
As to pain itself, some empirical studies suggest that it is com-mon.
Perhaps as indirect evidence of this is the proliferation of pain clinics
nationally. Of course, many patients attending these clinics fall into the category
of pain disorder associated with a general medical condition, but undoubtedly,
some also have in-volvement of psychological factors as required for a
diagnosis of pain disorder as a mental disorder. The same would apply to the 10
to 15% of adults in the USA in any given year who have work disability because
of back pain. Pain has been found to be a predominant symptom in 75% of
consecutive general medical patients, with 75% of these (thus 50% overall)
judged as hav-ing no identifiable physical cause. No apparent physical basis is
found in 40 to 50% of patients presenting with nonspecific ab-dominal pain. At
least half of such patients show major personal-ity problems in addition, with
such aberrations associated with poor outcome. Whereas primary care and other
nonpsychiatric physicians probably see most pain patients, 38% of psychiatric
inpatient admissions and 18% attending a psychiatric outpatient clinic report
pain as a significant problem.
Etiology and Pathophysiology
In considering the etiology of pain disorder, possible mecha-nisms of
pain itself must be considered. The definition of pain sanctioned by the
International Association for the Study of Pain Subcommittee on Taxonomy is “an
unpleasant sensory and emo-tional experience associated with actual or
potential tissue dam-age”. It goes on to acknowledge that pain is not simply
“activity induced in the nociceptor and nociceptive pathways by a noxious
stimulus” but “is always a psychological state…”. Thus, it accepts the
hypothesis that pain involves psychological as well as physi-cal factors.
Many theories of the etiology and pathophysiology of pain involving both
biological and psychological factors have been proposed. It is known that a
neuropathway descends from the cerebral cortex and medulla, which inhibits the
firing of pain transmission neurons when it is activated. This system is
appar-ently mediated by the endogenous opiate-like compounds, en-dorphins and
by serotonin. Indeed, metabolites of both of these neurotransmitters may be
reduced in the cerebrospinal fluid of chronic pain patients.
The gate
control theory links biological and psychological factors. It hypothesizes a
gate-like mechanism involving the dor-sal horn of the spinal cord by which
large A-beta fibers as well as small A-delta and C fibers carry impulses from
the periphery to the substantia gelatinosa and T-cells in the spinal cord.
Activation of the large fibers inhibits, whereas activation of the small fibers
facilitates transmission to the T-cells. In addition, impulses de-scending from
the brain, influenced by cognitive processes, may either inhibit or facilitate
transmission of pain impulses. Such a
mechanism may explain how psychological processes affect pain perception.
By definition, both pain disorder associated with psycho-logical factors
and pain disorder associated with both psychologi-cal factors and a general
medical condition involve psychological factors. In the case of the former, it
is presumed that there is little contribution from general medical conditions;
in the latter, both physical and psychological factors contribute. A plethora
of not necessarily mutually exclusive theories has been proposed to ex-plain
how this takes place.
Psychological constructs involving learning theories, both operant and
classical conditioning, may apply. In operant paradigms, pain-related
complaints are reinforced by increased attention, relief from obligations,
monetary compensation and the pleasurable effects of analgesics. In classical
conditioning, originally neutral settings such as a workplace or bedroom where
pain was experienced come to evoke pain-related behavior. So-cial and cultural
attitudes may also have effects. Patients with un-explained pain are more
likely than others to have close relatives with chronic pain. Although findings
have differed from study to study, ethnic differences may also have effects,
such as greater pain tolerance in Irish and Anglo-Saxon groups in comparison to
southern Mediterranean groups.
Diagnosis and Differential Diagnosis
As shown in Figure 54.1, the diagnostic approach begins with assessment
of whether the presentation is fully explained by a general medical condition.
If not, it may be assumed that psycho-logical factors play a major role. If it
is judged that psychological factors do not play a major role, a diagnosis of
pain disorder asso-ciated with a general medical condition may apply. As
previously mentioned, this does not have a mental disorder code.
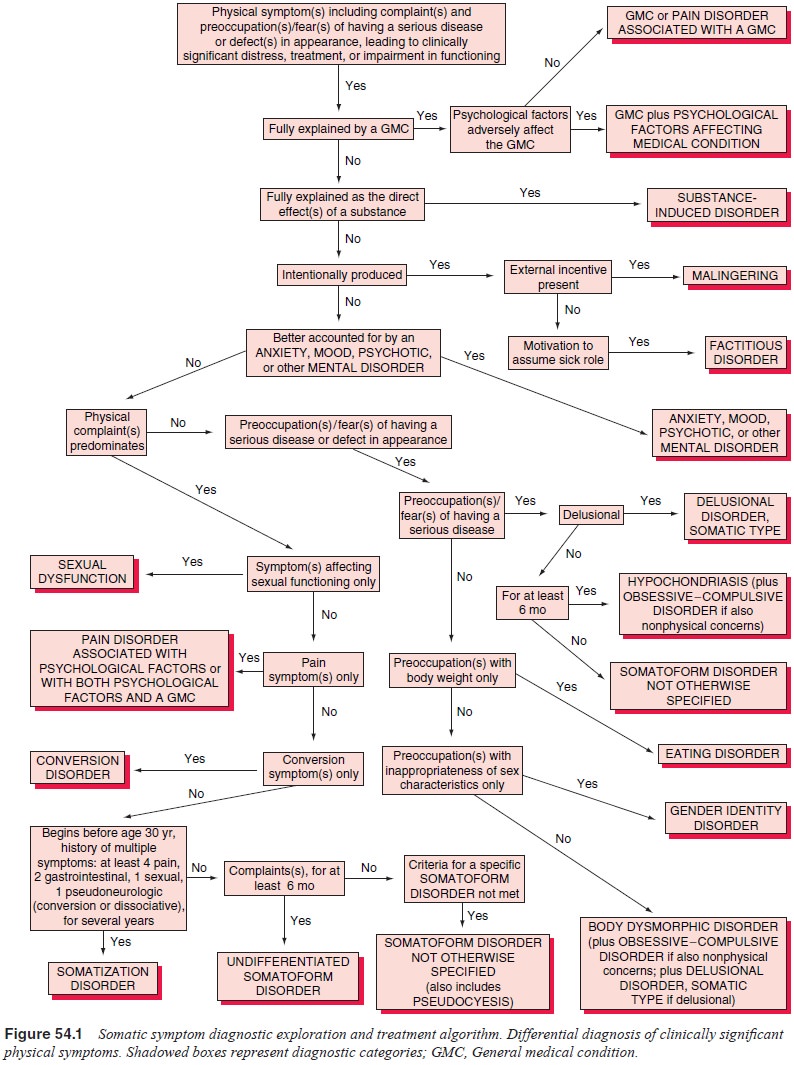
If psychological factors are involved, the first considera-tion is
whether the pain is feigned. If so, either malingering or factitious disorder
is diagnosed, depending on whether external incentives or assumption of the
sick role is the motivation. Evi-dence of malingering includes consideration of
external rewards relative to the chronology of the development and maintenance
of the pain. In factitious disorder, a pattern of successive hospi-talizations
and medical evaluations is evident. Inconsistency in presentation, lack of
correspondence to known anatomical path-ways or disease patterns, and lack of
associated sensory or mo-tor function changes suggest malingering or factitious
disorder, but pain disorder associated with psychological factors may show this
pattern as well. The key question is whether the patient is experiencing rather
than feigning the pain.
Determination of the relative contributions of psychologi-cal and
general medical factors is difficult. Of course, careful assessment of the
nature and severity of the potential underlying medical condition and the nature
and degree of pain that would be expected should be made. Traditionally, the
so-called conver-sion V or neurotic triad (consisting of elevation of the
hypochon-driasis and hysteria scales with a lower score on the depression
scale) on the Minnesota Multiphasic Personality Inventory has been purported to
indicate emotional indifference to the somatic concerns as might be expected if
the symptom is attributable to psychological factors rather than organic
disease. However, evidence indicates that this configuration may also occur as
an adjustment to chronic illness.
A diagnosis of pain disorder requires that the pain be of sufficient
severity to warrant clinical attention, that is, it causes clinically
significant distress or impairment. A number of instruments have been developed
to assess the degree of distress associated with the pain. Such measures
include the numerical rating scale and visual analog scale as described by
Scott and Huskisson (1976), the McGill Pain Questionnaire and the West
Haven-Yale Multidimensional Pain Inventory (Osterweis et al., 1987).
DSM-IV includes a number of exclusionary conventions. By definition, if
pain is restricted to pain with sexual intercourse, the sexual disorder,
dyspareunia, not pain disorder, is diagnosed. If pain occurs in the context of
a mood, anxiety, or psychotic disorder, pain disorder is diagnosed only if it
is an independent focus of clinical attention and is not better accounted for
by the other disorder, a highly subjective judgment.
If pain occurs exclusively during the course of somatiza-tion disorder,
pain disorder is not diagnosed because pain symp-toms are part of the criteria
for somatization disorder and are thereby subsumed under the more comprehensive
diagnosis. Because somatization disorder is virtually a lifelong condition,
this exclusion generally applies in someone with somatization disorder by
history. Important here is that, in addition to pain, somatization disorder
involves multiple symptoms of the gas-trointestinal system, the reproductive
system, and the central and peripheral nervous systems; whereas in pain
disorder, the focus is on pain symptoms only.
Specification of acute versus chronic pain disorder on the basis of
whether the duration is less than or greater than 6 months is an important
distinction. Whereas acute pain, in most cases, will be linked with physical
disorders, when pain remains unex-plained after 6 months, psychological factors
are often involved (Cloninger, 1993). However, the psychiatrist must remember
that a significant minority (in one study 19%) of patients with chronic pain of
no apparent physical origin will ultimately be found to have occult organic
disease (Cloninger, 1993).
In patients with unexplained pelvic pain, psychiatrists should be warned
about cavalier conclusions regarding the ab-sence of physical disease. With
laparoscopy, a high frequency of occult organic disease has been identified in
several stud-ies. Thus, laparoscopy may be indicated in patients with pelvic
pain. Electromyography may be helpful in distinguishing muscle contraction
headaches. Failure to show coronary artery spasm with provocative procedures
and failure to respond to nitroglyc-erin may be useful in distinguishing
patients with pain disorder from those in whom the pain is attributable to
coronary artery disease.
Course, Natural History and Prognosis
Given the heterogeneity of conditions subsumed under the pain disorder
rubric, course and prognosis vary widely. The subtyp-ing at 6 months is of
significance. The prognosis for total remis-sion is good for pain disorders of
less than 6 months’ duration. However, for syndromes of greater than 6 months’
duration, chronicity is common. The site of the pain may be another fac-tor.
Certain anatomically differentiated pain syndromes can be distinguished, and
each has its own characteristic pattern. These include syndromes characterized
primarily by headache, facial pain, chest pain, abdominal pain and pelvic pain.
In such syn-dromes, symptoms tend to be recurrent, with relapses occurring in
association with stress. A high rate of depression has been ob-served among
patients with unexplained facial pain. Facial pain is often alleviated by
antidepressant medication. This effect has been observed in both patients with
depressive symptoms and those without.
Other
factors affecting course and prognosis include as-sociated psychiatric illness
and external reinforcement. Employ-ment at the outset of treatment predicts
improvement. Chronicity is more likely in the presence of certain personality
diagnoses or traits, such as pronounced passivity and dependency. External
re-inforcement includes litigation involving potential financial com-pensation
or disability. Continuation of the pain disorder may prove more lucrative than
its resolution and return to work. Level of activity, which is generally
associated with improvement, is discouraged by fears of losing compensation.
Thus, although out-right malingering may be rare pain behaviors are often
reinforced and maintained. Habituation with addictive drugs is associated with
greater chronicity.
Treatment
An
overriding guideline is that the psychiatrist does not do any-thing that will
actually perpetuate and even promote “pain-re-lated behavior”. Thus, a major
goal is to encourage activity. Other guidelines include avoidance of
sedative–antianxiety drugs, ju-dicious use of analgesics on a fixed interval
schedule so as not to reinforce pain-related behaviors, avoidance of opioids
and con-sideration of alternative treatment approaches such as relaxation
therapy. Depression should be treated with appropriate antide-pressant drugs,
not sedative–antianxiety medications. The dif-ficulties in managing pain
disorder patients have resulted in the establishment of many clinics and
programs especially designed for pain. Referral to such a service may be
indicated. Interven-tion should best be provided early in the course of the
syndrome, before pain-related behaviors become entrenched. Once continu-ing
disability compensation is established, therapeutic efforts become much more
difficult.
The
preceding general guidelines apply whether or not a general medical basis for
the pain is involved. Of course, if only pain disorder associated with
psychological factors is involved, psychological management will be the mainstay.
For patients with pain associated with general medical factors (not a mental
disorder) in which psychological factors do not play a major role, efforts
should be made to prevent the development of psycho-logical problems in
response to the resulting distress, isolation and loss of function, and
iatrogenic effects such as exposure to potentially addicting drugs.
In acute
pain, the major goal is to relieve the pain. Thus, pharmacological agents
generally play a more significant role than in chronic syndromes. Whereas the
risk of developing opi-oid dependence appears to be surprisingly low (four per
12 000) among patients without a prior history of dependence, nonopioid agents
should be used whenever they can be expected to be ef-fective. As discussed for
chronic pain, these include particularly acetaminophen and the nonsteroidal
antiinflammatory drugs (NSAIDs), of which aspirin is considered a member. Even
if an opioid analgesic is employed, these drugs should be continued as
adjuncts; often, they lessen the required dose of the opioid.
It is
with the chronic syndromes that proper management is crucial to ease distress
and prevent the development of addi-tional problems. As advised by King (1994),
the overriding goal is to maintain function, because total relief of the pain
may not be possible. Physical and occupational therapy may play a major role.
There may be resistance to the involvement of a psychia-trist as an indication
that the pain is not seen as real. Such issues must first be resolved. An attempt
should be made to ascertain the roles that psychological and general medical
factors play in the maintenance of the pain.
A large variety of psychotherapies including individual, group and
family strategies have been employed. Two techniques that warrant special
attention are operant conditioning and cog-nitive–behavioral therapy. In
operant conditioning, the pattern of reinforcement of pain behavior by
medication, attention and ex-cuse from responsibilities is to be interrupted
and reinforcement shifted to usual daily activities. To assess the role of
operant con-ditioning, it may be necessary to have patients keep a diary and to
interview family members to identify any conditioning patterns. In
cognitive–behavioral therapies, the goal is the identification and correction
of attitudes, beliefs and expectations. Biofeedback and relaxation techniques
may be used to minimize muscle ten-sion that may aggravate if not cause pain.
Hypnosis may also be used to achieve muscle relaxation and to help the patient
“dissoci-ate” from the pain.
Pharmacological intervention may also be useful in chronic syndromes.
Effort should be made to avoid opioids if possible. Agents to be tried first
include antidepressants, aceta-minophen, NSAIDs (including aspirin) and anticonvulsants
such as carbamazepine. Antidepressants seem particularly useful for neuropathic
pain, headache, facial pain, fibrositis and arthri-tis (including rheumatoid
arthritis). Analgesic action seems to be independent of antidepressant effects.
Most work has been done with the tricyclic antidepressants; other classes, such
as the monoamine oxidase inhibitors (MAOIs) and the selective serotonin
reuptake inhibitors (SSRIs), may be effective as well. Although it was thought
that the action is mediated by serotonin-ergic effects, agents such as
desipramine with predominantly noradrenergic activity seem to be effective as
well. NSAIDs, of which aspirin, ibuprofen, naproxen and piroxicam are commonly
used examples, may alleviate pain through inhibition of prostag-landin
synthesis. Unfortunately, this effect may also contribute to side effects, such
as aggravation of peptic or duodenal ulcers and interference with renal
function. For patients unable to tolerate NSAIDs, acetaminophen should be
tried.
If opioid analgesics are used, it is recommended that use be tied to
objectives such as increasing level of activity rather than simply pain
alleviation. Milder opioids, such as codeine, oxycodone and hydrocodone, should
be implemented first. The once widely used propoxyphene has less analgesic
effect than these drugs; it is not devoid of abuse potential as once thought
and is not recommended. Pure opioid agonists such as morphine, methadone and
hydromorphone should be tried next. Meperidine, also in this class, is contraindicated
for prolonged use because accumulation of the toxic metabolite, normeperidine,
a cerebral irritant, may result in anxiety, psychosis, or seizures. Meperidine
may also have a lethal interaction with MAOIs. There are no ad-vantages to
mixed opioid agonist–antagonists. The commonly used pentazocine should be
avoided because it has abuse poten-tial and psychotomimetic effects in some
patients. It remains to be seen whether newer agents (buprenorphine,
butonphanol and nalbuphine) have lower abuse potential as claimed. Above all,
psychiatrists should be judicious in the use of opioid analgesics, considering
not only their abuse potential but their large number of side effects including
constipation, nausea and vomiting, ex-cessive sedation and, in higher doses,
respiratory depression that may be fatal.
In addition to pharmacotherapy, a number of other “physi-cal” techniques
have been used, such as acupuncture and trans-cutaneous electrical nerve
stimulation. These carry little risk of adverse effects or aggravation of the
pain disorder. Other proce-dures such as trigger point injections, nerve blocks
and surgicalablation may be recommended if specifically indicated by an
un-derlying general medical disorder.
As can be seen in the preceding discussion, the man-agement of pain
disorders is not monomodal. A great number of psychological and physical
factors and interventions may be considered.
Related Topics