Chapter: Modern Medical Toxicology: Chemical Poisons: Heavy Metals
Thallium - Chemical Poisons
Thallium
Thallium
is a soft and pliable metal which is acquiring an increasingly notorious
reputation as an ideal homicidal poison. Important derivatives include thallous
sulfate, acetate, chloride, iodide, nitrate, and carbonate. Most of these salts
(particularly thallous sulfate), are odourless, tasteless, and freely soluble
in water.
Uses
■■ Glass
and dye industry
■■ Rodenticide
■■ Depilatory
■■ Fireworks
■■ Cardiac
perfusion imaging.
Mode of Action
·
Thallium is a cellular toxin. It
behaves as a potassium analogue and is distributed intracellularly to all the
tissues of the body, but changes in distribution occur with the passage of
time. At low levels, thallium replaces potassium in the sodium-potassium ATPase
pump; at high levels it competitively inhibits sodium potassium ATPase.
·
Thallium also has an affinity for
sulfhydryl groups. The blocking of sulfhydryl cross-linking in keratin causes
alopecia and abnormalities in nail growth which are mani-fested as Mees’ lines.
Usual Fatal Dose
Average
fatal dose of thallium sulfate varies from 12 to 15 mg/ kg. The reported adult
fatal dose is approximately 1 gram of absorbed thallium.
Clinical Features
Absorption
can occur through inhalation, ingestion, or even across intact skin.
Acute Poisoning:
·
Abdominal pain, gastroenteritis
(sometimes with haematemesis, and haematochezia), tachycardia, and headache,
followed by confusion, paraesthesias, hallucinations, convulsions, retrobulbar
neuritis, and ophthalmoplegia. Death results from respiratory failure.
·
Occasionally, patients develop
hepatic or renal failure.
·
There may be bone marrow depression.
·
A characteristic, dark pigmented
band is often noticed in the scalp hair in about 3 to 4 days.
·
Urine that is first voided after
poisoning may show a green discolouration.
Chronic Poisoning:
· Alopecia (Fig 9.23)—One of the pathognomonic signs ofchronic thallium intake, it begins about 10 days after the first dose and may lead to total scalp hair loss in about a month if the intake is continued. Apart from scalp hair, the lateral halves of the eyebrows is (peculiarly) affected. Regrowth of the hair occurs if the patient survives the poisoning.
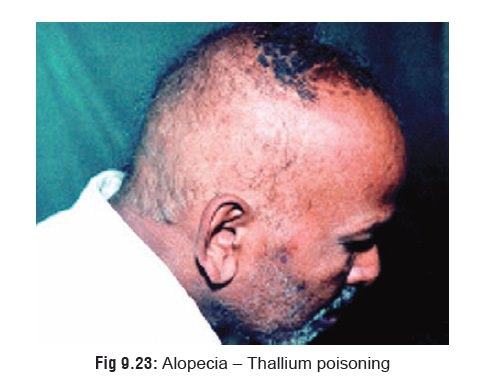
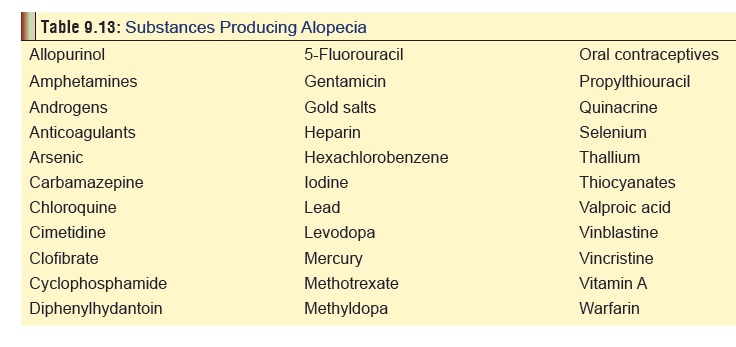
Table 9.13 lists some important substances which produce alopecia.
·
Skin
rash—This is in the form of a papulomacular rashwhich often
assumes a “butterfly” distribution on the face. There may be acneiform
eruptions.
·
Dystrophy
of the nails (Mees’ stripes or lines)*
·
Painful ascending peripheral sensorimotor neuropathy. Pain
and paraesthesias are most pronounced in the lower limbs, particularly the
soles. Painful peripheral neuropathy and paraesthesia, primarily of the legs
and feet, are among the first symptoms noted. Pain may be described as aching,
tingling or burning and may be so severe as to prohibit walking. Paraesthesias
may develop within 2 to 6 days in severe poisoning. Loss of pain, temperature,
vibratory and position sense may all occur and an unsteady gait may develop.
·
Ataxia.
· Other neurological manifestations—cranial nerve palsies, optic neuropathy, choreoathetosis, tremor, and encephalopathy. Psychotic behaviour may be noted.
·
Ophthalmological
manifestations—ptosis, ophthal-moplegia, nystagmus, keratitis, lens
opacities, optic atrophy. Functional changes include abnormal colour vision
(tritanomaly), impaired visual acuity, and central scotomas.
·
Cardiovascular
and haematological manifestations—hypertension, cardiomyopathy, ECG
changes, leuko-cytosis, and thrombocytopenia. Cardiac arrhythmias, bradycardia,
and T wave abnormalities have been reported. Severe cases of acute poisoning
may result in refractory cardiogenic shock.
·
Other
symptoms and signs—autonomic dysfunction,testicular
toxicity, hypokalaemia, renal failure, and hepatic dysfunction. A bluish line
in the gums may appear 3 to 4 weeks post-ingestion. Respiratory failure often
develops in patients with severe motor neurop-athy. Prolonged ventilatory
support may be required.
The
outstanding combination of alopecia and
skin rash,painful peripheral neuropathy, and mental confusion with lethargy (thallium triad), in any clinical case
must immediatelyarouse the suspicion of chronic thallium poisoning. A high
level of suspicion should be kept for thallium poisoning in patients with
painful peripheral neuropathy and gastrointestinal symptoms, which appear much
earlier than alopecia, since the prognosis is much better with early diagnosis and
treatment.
The
progression of symptoms may sometimes mimic other conditions, particularly
Guillain Barre syndrome (Landry’s paralysis, acute infectious polyneuritis),
acute porphyria, psychosis, or thiamine deficiency.
Sequelae,
including mental retardation, psychosis, abnormal reflexes, ataxia, tremor,
flaccid paraparesis, cerebellar ataxia, and mental impairment have been
reported. There are reports of neurological sequelae lasting more than 30
years.
Diagnosis
·
X-ray: may reveal opacities in the
GIT or liver.
·
Tests of contrast sensitivity and
colour vision are useful in the early detection of optic neuropathy in thallium
poisoning.
·
Abnormal EEG and delayed peripheral
nerve conduction.
·
Microscopy of scalp hair may reveal
a diagnostic pattern of black pigmentation of hair roots.
·
Urine test: Combine a few drops of
urine with 3 drops of saturated bromine water, 3 drops of sulfosalicylic acid,
1 drop of HCl, 2 drops of a solution of 0.05 gram of rhoda-mine B in 100 ml of
concentrate HCl. Mixture add 1 ml of benzene, shake, centrifuge, and examine
the benzene layer. A bright yellow or fluorescent red colour indicates a
positive result.
Preparation of reagents:
Bromine solution—Dissolve 10 gram of sodium bromide in 10 ml
of water. Add 20 ml of 6N HCl followed by 2.5 ml of liquid bromine.
Sulfosalicylic acid—Mix 1 part saturated sulfosalicylic acid
with 2 parts of 6N HCl. Atomic absorption spectroscopy.
·
Urinary excretion of thallium in
excess of 10–20 mg in 24 hours is considered diagnostic. Although less reliable
for diagnosis than 24 hour urinary thallium excretion, whole blood thallium
exceeding 100 mcg/dL indicates potential poisoning.
·
Hypocalcaemia—Monitor calcium levels
during the acute phase.
Treatment
· In acute poisoning, stomach wash can
be done with Prussian Blue [potassium ferric ferrocyanide or potassium ferric
hexacyanoferrate i.e. KFe(Fe(CN)6)] which prevents the absorption of
thallium by binding with it, exchanging potas-sium for thallium in its crystal
lattice network. Prussian Blue is then instilled through a duodenal tube (125
mg/kg twice a day, with 50 ml of 15% mannitol).* This is continued until the
urinary excretion falls below 0.5 mg/day.
· Activated charcoal may be
beneficial. Thallium is thought to undergo enterohepatic recirculation, and
multiple dose activated charcoal may enhance its elimination.
· Forced diuresis in conjunction with
potassium chloride. Potassium chloride therapy has been reported to enhance
excretion of thallium, but there are conflicting reports as to its efficacy in
enhancing elimination.
· Haemodialysis along with
haemoperfusion can remove significant amounts of thallium from the blood.
· Chelating agents such as BAL, EDTA,
etc. are not effec-tive.
· Diethyldithiocarbamate (Dithiocarb)
was till recently advocated as an antidote. However it sometimes leads to a
worsening of the patient’s condition and is therefore not recommended today.
· Physiotherapy, to prevent muscle
contractures.
·
Shaving the patient’s head may reduce the psychological
stress of hair loss, and improve the patient’s morale.
· Special attention must be paid to
oral hygiene, otherwise a severe stomatitis may result.
If
treatment is instituted in time, recovery from thallium![]() poisoning is the rule, though this may take a
long time. There may be residual effects such as amnesia, ataxia, tremor, and
foot drop.
poisoning is the rule, though this may take a
long time. There may be residual effects such as amnesia, ataxia, tremor, and
foot drop.
Autopsy Features
·
Alopecia.
·
Stomatitis.
·
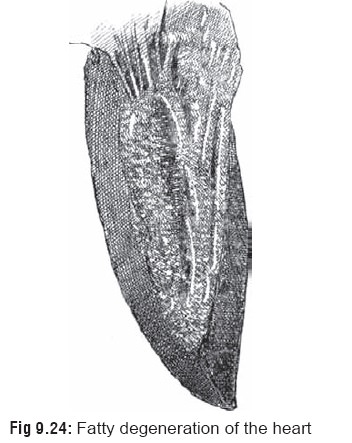
Fatty degeneration of heart (with
“tabby cat striation” of the ventricles) (Fig
9.24).
·
Fatty degeneration of liver.
·
Renal damage.
·
Pulmonary oedema.
·
Cerebral oedema with widespread
degeneration of nerve cells and axons.
Forensic Issues
■■ Accidental poisoning
occurs due to industrial or occupa-tional exposure. It can also occur
inadvertently from its use as a rodenticide. Several instances of accidental
poisoning have been reported in children who have consumed cock-roach or rat
bait containing thallium.
■■ Suicides
with thallium have always been rare in India, though they were relatively
common abroad until the 1960s when legislation was passed in most Western
countries greatly restricting its availability for use as pesticides. In 1975,
USA banned its use altogether as a rodenticide.
■■The most disturbing aspect about thallium today is its
increasing deployment by poisoners to commit murder. There have been several
celebrated cases of murder reported over a period of time, especially in
Western countries.
Related Topics