Chapter: Medicine and surgery: Musculoskeletal system
Systemic lupus erythematosus - Connective tissue disorders
Connective tissue disorders
Systemic lupus erythematosus
Definition
Systemic lupus erythematosus (SLE) is a multisystem disorder characterised by inflammation and profound immunological disturbance.
Prevalence
40 per 100,000 in United Kingdom, wide geographic variation (1:250 American black women).
Age
Usually 16–55 years with a peak in early twenties.
Sex
9F : 1M
Geography
Commoner in West Indies, Singapore and Far East.
Aetiology
Genetics: Up to 60% concordance in monozygotic twins. 5–10% risk in first-degree relatives. HLA-B8, DR2 and DR3 are associated with increased incidence of SLE as are deficiencies in complement factors such as C1q, C2 and C4. Currently studies are underway into a number of chromosomal loci in relation to SLE.
Hormonal: There is evidence that females are predominantly affected and there are commonly premenstrual and puerperium exacerbations. It is suggested that oestrogen may be involved in the aetiology of SLE.
Immunological factors: Significant disturbance of normal immunology is seen in patients with SLE; how-ever, it is unclear if these are aetiological factors for, or the consequence of the disorder:
i. Polyclonal activation of B cells in the early stages of the disease resulting in hypergammaglobulinaemia. B cells also have an increased life span.
ii. T-cell regulation is also affected resulting in decreased cytotoxic T-cell reactions, increased helper T cells and abnormalities in the cytokine balance.
iii. There are also abnormalities in cell-to-cell signaling and in apoptosis within the immune system.
It is thought that these defects may trigger a cascade of events resulting in the production of autoantibodies. Over time these antibodies undergo maturation of affinity resulting in high affinity antibodies to DNA, Smooth muscle (Sm), RNP, Ro, La, nucleosomes and other nuclear antigens.
Environmental factors: Suggested factors include viruses, ultraviolet light and reactions to medication.
Pathophysiology
The mechanism by which the aetiological factors inter-act to cause the disease is still unclear; however, many of the clinical manifestions are the result of the formation of immune complexes and subsequent complement activation (e.g. lupus nephritis).
Clinical features
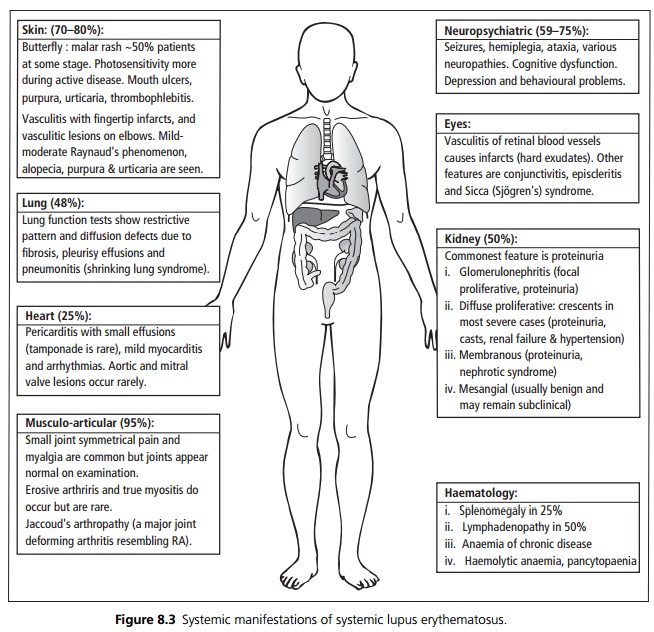
Systemic lupus erythematosus is a multisystem disorder affecting skin, joints, kidneys, lungs, nervous system, mucous membranes and other organs. The presentation is very variable between individuals. The clinical course is characterised by relapses, which may be prolonged, and remissions. Systemic symptoms include general malaise, fever (sometimes high and swinging) and depression (see Fig. 8.3).
Microscopy
Fibrinoid necrosis around blood vessels (usually arterioles, venules and capillaries) pleura and joint capsules.
Immune complex deposition in skin at the dermal– epidermal junction, kidney and blood vessels.
Investigations
ANAs seen in 95–99% of SLE. Anti-double stranded DNA antibodies are relatively specific but only 50% sensitive. Other autoantibodies seen include anti-RNP, anti-smooth muscle, anti-Ro (SSa) and anti-La (SSb). Rheumatoid factor is seen in 50%.
Complement is low during active disease suggesting complement activation and consumption by immune complexes.
False positive tests for syphilis are found in approximately 10% of patients (positive WR or VDRL because cardiolipin is a component of the antigenic mixture used in these assays). The fluorescentTreponema pallidum antibody test is negative.
ESR is raised in active disease, with normal CRP levels. Immunoglobulins usually polyclonal increase in gammaglobulins.
Haematological abnormalities:
1 Normochromic, normocytic anaemia in 75%.
2 Direct antiglobulin test positive haemolytic anaemia in 10–20%.
3 Leucopenia and mild thrombocytopaenia.
4 Antibodies to clotting factors especially lupus anti-coagulant directed against prothrombin activator (see below).
Management
Most patients with mild disease are treated conservatively.
Nonsteroidal anti-inflammatory drugs are first-line treatment for articular disease.
Antimalarials are used for systemic symptoms, refractory arthritis and skin disease.
· Hydroxychloroquine for skin and joint problems. Mepacrine causes yellow pigmentation but is useful. Six monthly eye-checks are recommended.
Corticosteroids:
· High dose for widespread vasculitis, acute nephritis, severe CNS vasculitis.
· Moderate dose for pleural effusions or moderate thrombocytopenia.
Immunosuppressive agents:
· Azathioprine is used as a steroidsparing agent. Cyclophosphamide is more toxic but may be used in severe diffuse proliferative nephritis or severe neuropsychiatric lupus.
Prognosis
Generally a good prognosis, chronic forms of the disease are seen. Patients with renal or neuropsychiatric involvement have a worse prognosis.
Related Topics