Chapter: Medicine and surgery: Musculoskeletal system
Osteoarthritis - Bone and joint infections
Osteoarthritis
Definition
Previously thought of as a degenerative joint disorder of ageing, osteoarthritis is now considered to be a joint disorder resulting from damage and repair to cartilage and reaction in the surrounding bone.
Prevalence
Radiological changes universal in old age, symptomatic disease occurs in 20%.
Age
Peak onset 45–60 years.
Sex
F > M
Aetiology
Primary osteoarthritis: Risk factors include obesity, increasing age, female sex, wear of cartilage through repeated trauma.
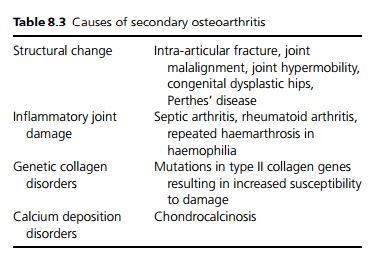
Secondary osteoarthritis: Osteoarthritis may result from damage to the joint or changes to the way forces are transmitted through the cartilage (see Table 8.3).
Pathophysiology
Normal cartilage consists of chondrocytes, collagen and extracellular matrix. The damage seen in osteoarthritis is initiated by trauma, which may be a single event or repeated microtrauma. Any underlying collagen defect will predispose to damage. There is resultant increased proliferation and activity of chondrocytes under the influence of monocytederived growth peptides. Once the process of osteoarthritis has begun a number of factors are involved in the continued disease process:
Mechanical forces can be causative, preventative or therapeutic.
Proteases that are involved with cartilage degradation. It has been suggested that protease activation is important.
Cytokines including IL-1 and TNF-α, have a role in cartilage degradation. Growth factors mediating collagen repair include insulinlike growth factor and transforming growth factor β(TGF-β), which reduces the activity of proteases and therefore limits cartilage degradation.
Other factors implicated include crystals and nitric oxide.
Clinical features
Patients tend to present with gradual onset of joint pain, which is exacerbated by exercise and relieved by rest. As the disease progresses, pain occurs with less activity and eventually occurs at rest. Stiffness occurs after a period of rest, but is less severe than rheumatoid arthritis and lasts 5–15 minutes in morning. On examination there may be joint line tenderness, joint effusion, crepitus and bony enlargement due to osteophyte development. There is gradual limitation of movement with resultant muscle wasting and deformity.
Hands: An enlargement of the distal (Heberden’s nodes) and proximal interphalangeal (Bouchard’s nodes) joints results in a square appearance of the hands. The development of Heberden’s nodes appears to have a genetic predisposition.
Feet/ankles: The first metatarsophalangeal joint is commonly affected; subtalar joint involvement may cause difficulty with walking.
Knees: The medial part of the knee joint may be affected more than the lateral causing a genu varum. Knee involvement often results in osteophyte formation, joint effusion, crepitus and a Baker’s cyst palpable in the popliteal fossa.
Hips are commonly affected, although some apparent hip pain may be referred from other areas.
Spine: Particularly the cervical and lumbar region.
Investigations
The first radiological finding is narrowing of the joint space. In weight-bearing joints narrowing is maximal in the areas subjected to the greatest pressures. As the cartilage is worn away, friction causes the exposed sub-chondral bone to become sclerotic (subarticular bony sclerosis). The presence of bone cyst formation is a common finding. Later findings include bony collapse and the formation of osteophytes (bony outgrowths that are seen at the margins of the joint). Inflammatory markers and autoantibodies are negative.
Management
1 Non-pharmacological management includes weight loss, physiotherapy, walking aids and hydrotherapy to rebuild lost muscle bulk.
2 Medical treatments are used for pain relief. Simple analgesia and nonsteroidal anti-inflammatory drugs are the mainstay of treatment supplemented by intra-articular steroid injection. See also indications for Cox II antagonists under rheumatoid arthritis (page 360).
3 Surgical: The aim of surgery is to relieve pain not treated by medical management and to increase useful function.
· Osteotomy is the surgical realignment of a joint (normally hip or knee), which may produce benefit for 1–10 years post-surgery. It allows alteration of the muscle use, the contact areas and the blood dynamics within the joint. It is of most use in younger patients with a good range of movement and relative preservation of the intra-articular cartilage.
· Arthroscopic procedures include synovectomy (removal of the synovium), irrigation of joints and debridement.
· Arthroplasty (joint replacement) is the treatment of choice in older patients. Hip and knee replacements are the most successful; however, there is a risk of failure after about 10 years. In the upper limb, although the joints are not weight bearing, the normal range of movement is difficult to achieve and the prostheses are prone to failure.
· Arthrodesis (joint fusion) can be useful for pain, but can only be used if the loss of function is acceptable.
Prognosis
The disease may show a slow progression, little or no change over years, or a stepwise deterioration. There are some genetically inherited disorders with early onset osteoarthritis, which have a much worse prognosis.
Related Topics