Chapter: Medical Physiology: Renal Regulation of Potassium, Calcium, Phosphate, and Magnesium; Integration of Renal Mechanisms for Control of Blood Volume and Extracellular Fluid Volume
Summary of Factors That Regulate Potassium Secretion
Summary of Factors That Regulate Potassium Secretion: Plasma Potassium Concentration, Aldosterone, Tubular Flow Rate, and Hydrogen Ion Concentration
Because normal regulation of potassium excretion occurs mainly as a result of changes in potassium secretion by the principal cells of the late distal and collecting tubules, we will discuss the primary factors that influence secretion by these cells. The most impor-tant factors that stimulate potassium secretion by the principal cells include (1) increased extracellular fluid potassium concentration, (2) increased aldosterone, and (3) increased tubular flow rate.
One factor that decreases potassium secretion is increased hydrogen ion concentration (acidosis).
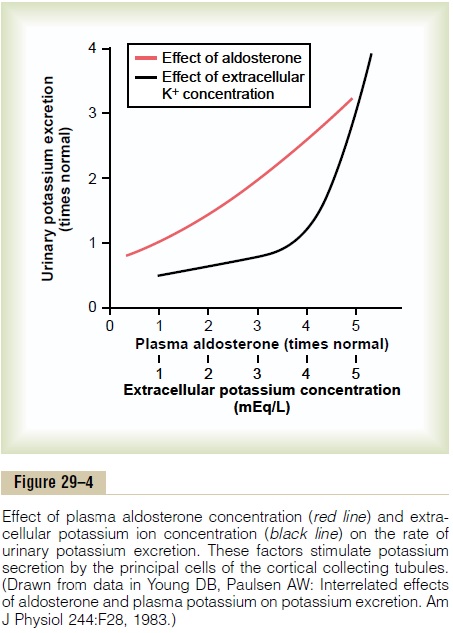
Increased Extracellular Fluid Potassium Concentration Stimu-lates Potassium Secretion. The rate of potassium secre-tion in the late distal and cortical collecting tubules is directly stimulated by increased extracellular fluid potassium concentration, leading to increases in potas-sium excretion, as shown in Figure 29–4. This effect is especially pronounced when extracellular fluid potassium concentration rises above about 4.1 mEq/L, slightly less than the normal concentration. Increased plasma potassium concentration, therefore, serves as one of the most important mechanisms for increasing potassium secretion and regulating extracellular fluid potassium ion concentration.
There are three mechanisms by which increased extracellular fluid potassium concentration raises potassium secretion: (1) Increased extracellular fluid potassium concentration stimulates the sodium-potassium ATPase pump, thereby increasing potas-sium uptake across the basolateral membrane. This in turn increases intracellular potassium ion concentra-tion, causing potassium to diffuse across the luminal membrane into the tubule. (2) Increased extracellular potassium concentration increases the potassium gra-dient from the renal interstitial fluid to the interior of the epithelial cell; this reduces backleakage of potas-sium ions from inside the cells through the basolateral membrane. (3) Increased potassium concentration stimulates aldosterone secretion by the adrenal cortex, which further stimulates potassium secretion, as dis-cussed next.
Aldosterone Stimulates Potassium Secretion. We discuss the fact that aldosterone stimulates active reabsorption of sodium ions by the principal cells of the late distal tubules and collecting ducts. This effect is mediated through a sodium-potassium ATPase pump that transports sodium outward through the basolateral membrane of the cell and into the blood at the same time that it pumps potassium into the cell. Thus, aldosterone also has a powerful effect to control the rate at which the principal cells secrete potassium.
A second effect of aldosterone is to increase the per-meability of the luminal membrane for potassium, further adding to the effectiveness of aldosterone in stimulating potassium secretion. Therefore, aldos-terone has a powerful effect to increase potassium excretion, as shown in Figure 29–4.
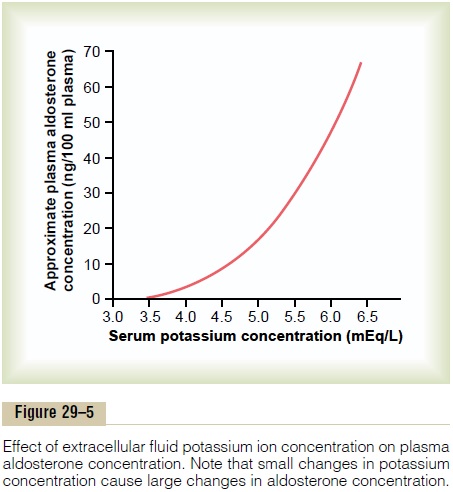
Increased Extracellular Potassium Ion Concentration Stimu-lates Aldosterone Secretion. In negative feedback controlsystems, the factor that is controlled usually has a feedback effect on the controller. In the case of the aldosterone-potassium control system, the rate of aldosterone secretion by the adrenal gland is con-trolled strongly by extracellular fluid potassium ion concentration. Figure 29–5 shows that an increase in plasma potassium concentration of about 3 mEq/L can increase plasma aldosterone concentration from nearly 0 to as high as 60 ng/100 ml, a concentration almost 10 times normal.
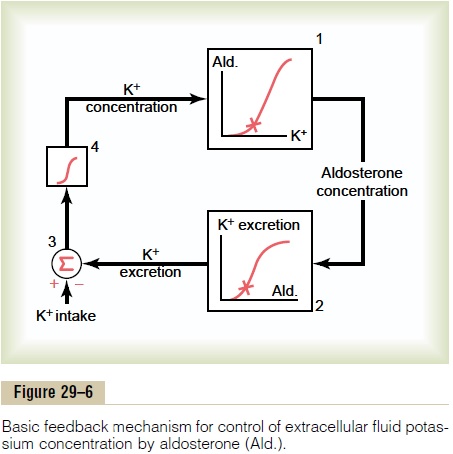
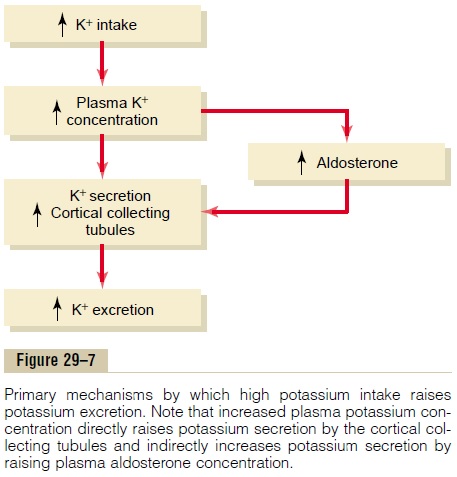
The effect of potassium ion concentration to stimu-late aldosterone secretion is part of a powerful feed-back system for regulating potassium excretion, as shown in Figure 29–6. In this feedback system, an increase in plasma potassium concentration stimulates aldosterone secretion and, therefore, increases the blood level of aldosterone (block 1). The increase in blood aldosterone then causes a marked increase in potassium excretion by the kidneys (block 2). The increased potassium excretion then reduces the extra-cellular fluid potassium concentration back toward normal (blocks 3 and 4). Thus, this feedback mecha-nism acts synergistically with the direct effect of increased extracellular potassium concentration to elevate potassium excretion when potassium intake is raised (Figure 29–7).
Blockade of Aldosterone Feedback System Greatly Impairs Control of Potassium Concentration. In the absence ofaldosterone secretion, as occurs in patients with Addison’s disease, renal secretion of potassium is impaired, thus causing extracellular fluid potassium concentration to rise to dangerously high levels. Con-versely, with excess aldosterone secretion (primary aldosteronism), potassium secretion becomes greatly increased, causing potassium loss by the kidneys and thus leading to hypokalemia.
The special quantitative importance of the aldos-terone feedback system in controlling potassium con-centration is shown in Figure 29–8. In this experiment, potassium intake was increased almost sevenfold in dogs under two conditions: (1) under normal condi-tions and (2) after the aldosterone feedback system had been blocked by removing the adrenal glands and placing the animals on a fixed rate of aldosterone infu-sion so that plasma aldosterone concentration could neither increase nor decrease.
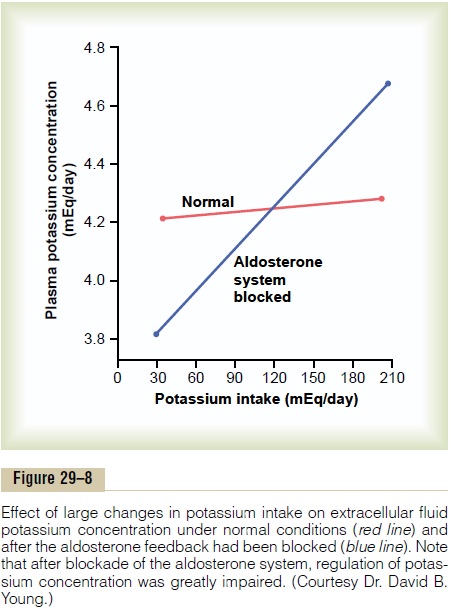
Note that in the normal animals, a sevenfold increase in potassium intake caused only a slight in-crease in potassium concentration, from 4.2 to 4.3 mEq/ L. Thus, when the aldosterone feedback system is functioning normally, potassium concentration is pre-cisely controlled, despite large changes in potassium intake.
When the aldosterone feedback system was blocked, the same increases in potassium intake caused a much larger increase in potassium concen-tration, from 3.8 to almost 4.7 mEq/L. Thus, control of potassium concentration is greatly impaired when the aldosterone feedback system is blocked. A similar impairment of potassium regulation is observed in humans with poorly functioning aldosterone feedback systems, such as occurs in patients with either primary aldosteronism (too much aldosterone) or Addison’s disease (too little aldosterone).
IncreasedDistalTubularFlowRateStimulatesPotassium Secretion. A rise in distal tubular flow rate, as occurswith volume expansion, high sodium intake, or diuretic drug treatment, stimulates potassium secretion. Con-versely, a decrease in distal tubular flow rate, as caused by sodium depletion, reduces potassium secretion.
The mechanism for the effect of high-volume flow rate is as follows: When potassium is secreted into the tubular fluid, the luminal concentration of potassium increases, thereby reducing the driving force for potas-sium diffusion across the luminal membrane. With increased tubular flow rate, the secreted potassium is continuously flushed down the tubule, so that the rise in tubular potassium concentration becomes mini-mized. Therefore, net potassium secretion is stimu-lated by increased tubular flow rate.
The effect of increased tubular flow rate is especially important in helping to preserve normal potassium excretion during changes in sodium intake. For example, with a high sodium intake, there is decreased aldosterone secretion, which by itself would tend to decrease the rate of potassium secretion and, there-fore, reduce urinary excretion of potassium. However, the high distal tubular flow rate that occurs with a high sodium intake tends to increase potassium secretion
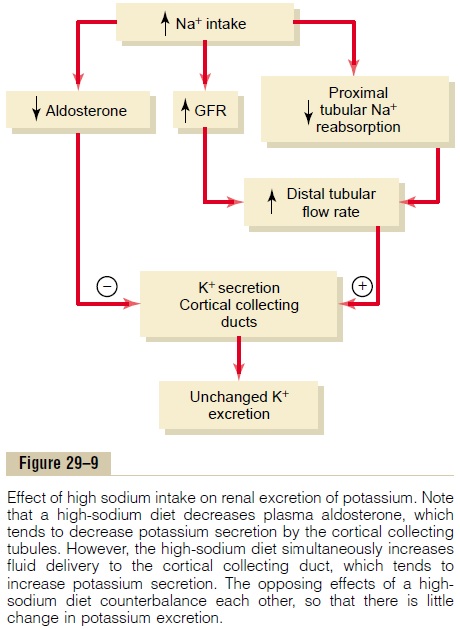
(Figure 29–9),. Therefore, the two effects of high sodium intake, decreased aldosterone secretion and the high tubular flow rate, counterbalance each other, so that there is little change in potassium excretion. Likewise, with a low sodium intake, there is little change in potassium excretion because of the counterbalancing effects of increased aldosterone secretion and decreased tubular flow rate on potassium secretion.
Acute Acidosis Decreases Potassium Secretion. Acuteincreases in hydrogen ion concentration of the extra-cellular fluid (acidosis) reduce potassium secretion, whereas decreased hydrogen ion concentration (alka-losis) increases potassium secretion. The primary mechanism by which increased hydrogen ion concen-tration inhibits potassium secretion is by reducing the activity of the sodium-potassium ATPase pump. This in turn decreases intracellular potassium concentra-tion and subsequent passive diffusion of potassium across the luminal membrane into the tubule.
With more prolonged acidosis, lasting over a period of several days, there is an increase in urinary potassium excretion. The mechanism for this effect is due in part to an effect of chronic acidosis to inhibit proximal tubular sodium chloride and water reabsorption, which increases distal volume delivery, thereby stimulating the secretion of potassium. This effect overrides the inhibitory effect of hydrogen ions on the sodium-potassium ATPase pump. Thus, chronic acidosis leads to a loss of potassium, whereas acute acidosis leads to decreased potassium excretion.
Related Topics