Chapter: Medical Surgical Nursing: Shock and Multisystem Failure
Stages of Shock
Stages of Shock
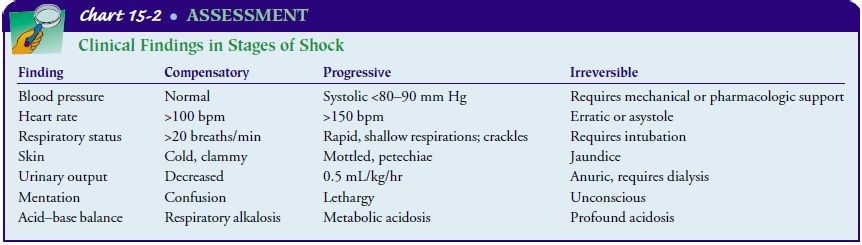
Some think of the shock syndrome as a continuum along which the patient struggles to survive. A convenient way to understand the physiologic responses and subsequent clinical signs and symp-toms is to divide the continuum into separate stages: compen-satory, progressive, and irreversible. (Although some authorities identify an initial stage of shock, changes attributed to this stage occur at the cellular level and are generally not detectable clini-cally.) The earlier that medical management and nursing inter-ventions can be initiated along this continuum, the greater the patient’s chance of survival.
COMPENSATORY STAGE
In the compensatory stage of shock, the patient’s blood pressure remains
within normal limits. Vasoconstriction, increased heart rate, and increased
contractility of the heart contribute to main-taining adequate cardiac output.
This results from stimulation of the sympathetic nervous system and subsequent
release of cate-cholamines (epinephrine and norepinephrine). The patient
dis-plays the often-described “fight or flight” response. The body shunts blood
from organs such as the skin, kidneys, and gas-trointestinal tract to the brain
and heart to ensure adequate blood supply to these vital organs. As a result,
the patient’s skin is cold and clammy, bowel sounds are hypoactive, and urine
output de-creases in response to the release of aldosterone and ADH.
Clinical Manifestations
Despite a normal blood pressure, the patient shows numerous clinical
signs indicating inadequate organ perfusion (Chart 15-2). The result of
inadequate perfusion is anaerobic metabolism and a buildup of lactic acid,
producing metabolic acidosis. The respira-tory rate increases in response to
metabolic acidosis. This rapid res-piratory rate facilitates removal of excess
carbon dioxide but raises the blood pH and often causes a compensatory
respiratory alkalo-sis. The alkalotic state causes mental status changes, such
as con-fusion or combativeness, as well as arteriolar dilation. If treatment
begins in this stage of shock, the prognosis for the patient is good.
Medical Management
Medical treatment is directed toward identifying the cause of the shock,
correcting the underlying disorder so that shock does not progress, and
supporting those physiologic processes that thus far have responded
successfully to the threat. Because compensation cannot be effectively
maintained indefinitely, measures such as fluid replacement and medication
therapy must be initiated to maintain an adequate blood pressure and reestablish
and main-tain adequate tissue perfusion.
Nursing Management
Early intervention along the continuum of shock is the key to im-proving
the patient’s prognosis. Therefore, the nurse needs to as-sess systematically
those patients at risk for shock to recognize the subtle clinical signs of the
compensatory stage before the patient’s blood pressure drops.
MONITORING TISSUE PERFUSION
In assessing tissue perfusion, the nurse observes for changes in level
of consciousness, vital signs (including pulse pressure), urinary output, skin,
and laboratory values. In the compensatory stage of shock, serum sodium and
blood glucose levels are elevated in re-sponse to the release of aldosterone
and catecholamines.
The role of the nurse at the compensatory stage of shock is to monitor
the patient’s hemodynamic status and promptly report deviations to the
physician, assist in identifying and treating the underlying disorder by
continuous in-depth assessment of the pa-tient, administer prescribed fluids
and medications, and promote patient safety. Vital signs are key indicators of
the patient’s he-modynamic status; however, blood pressure is an indirect
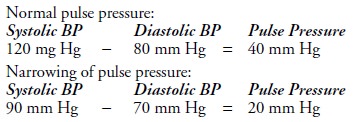
method of monitoring tissue hypoxia. Pulse pressure correlates well to stroke
volume, the amount of blood ejected from the heart with systole. Pulse pressure
is calculated by subtracting the diastolic measurement from the systolic
measurement; the difference is the pulse pressure. Normally, the pulse pressure
is 30 to 40 mm Hg (Mikhail, 1999). Narrowing or decreased pulse pressure is an
earlier indicator of shock than a drop in systolic blood pressure. Decreased or
narrowing pulse pressure, an early indication of de-creased stroke volume, is
illustrated in the following example:
Systolic blood pressure − diastolic blood pressure = pulse pressure
Elevation in the diastolic blood pressure with release of
cate-cholamines and attempts to increase venous return through
vaso-constriction is an early compensatory mechanism in response to decreased
stroke volume, blood pressure, and overall cardiac output.
Although treatments are prescribed and initiated by the physi-cian, the nurse usually implements them, operates and trou-bleshoots equipment used in treatment, monitors the patient’s status during treatment, and assesses the immediate effects of treatment. Additionally, the nurse assesses the response of the pa-tient and the family to the crisis and to treatment.
REDUCING ANXIETY
While experiencing a
major threat to health and well-being and being the focus of attention of many
health care providers, the patient often becomes anxious and apprehensive.
Providing brief explanations about the diagnostic and treatment procedures,
sup-porting the patient during those procedures, and providing in-formation
about their outcomes are usually effective in reducing stress and anxiety and
thus promoting the patient’s physical and mental well-being.
PROMOTING SAFETY
Another nursing intervention is monitoring potential threats to the
patient’s safety, because a high anxiety level and altered men-tal status
typically impair a person’s judgment. In this stage, pa-tients who were
previously cooperative and followed instructions may now disrupt intravenous
lines and catheters and complicate their condition. Therefore, close monitoring
is essential.
PROGRESSIVE STAGE
In the progressive stage of shock, the mechanisms that regulate blood
pressure can no longer compensate and the MAP falls below normal limits, with
an average systolic blood pressure of less than 90 mm Hg (Abraham et al.,
2000).
Pathophysiology
Although all organ systems suffer from hypoperfusion at this stage, two
events perpetuate the shock syndrome. First, the over-worked heart becomes
dysfunctional; the body’s inability to meet increased oxygen requirements
produces ischemia; and biochem-ical mediators cause myocardial depression
(Kumar, Haery & Parrillo, 2000; Price, Anning, Mitchell et al., 1999). This
leads to failure of the cardiac pump, even if the underlying cause of the shock
is not of cardiac origin. Second, the autoregulatory func-tion of the
microcirculation fails in response to numerous bio-chemical mediators released
by the cells, resulting in increased capillary permeability, with areas of
arteriolar and venous con-striction further compromising cellular perfusion. At
this stage, the patient’s prognosis worsens. The relaxation of precapillary
sphincters causes fluid to leak from the capillaries, creating inter-stitial
edema and return of less fluid to the heart. Even if the underlying cause of
the shock is reversed, the breakdown of the circulatory system itself
perpetuates the shock state, and a vicious circle ensues.
Assessment and Diagnostic Findings
Chances of survival depend on the patient’s general health before the
shock state as well as the amount of time it takes to restore tis-sue
perfusion. As shock progresses, organ systems decompensate.
RESPIRATORY EFFECTS
The lungs, which become compromised early in shock, are af-fected at
this stage. Subsequent decompensation of the lungs in-creases the likelihood
that mechanical ventilation will be needed if shock progresses. Respirations
are rapid and shallow. Crackles are heard over the lung fields. Decreased
pulmonary blood flow causes arterial oxygen levels to decrease and carbon
dioxide levels to increase. Hypoxemia and biochemical mediators cause an
in-tense inflammatory response and pulmonary vasoconstriction, perpetuating the
pulmonary capillary hypoperfusion and hypox-emia. The hypoperfused alveoli stop
producing surfactant andsubsequently collapse. Pulmonary capillaries begin
to leak their contents, causing pulmonary edema, diffusion abnormalities
(shunting), and additional alveolar collapse. Interstitial inflam-mation and
fibrosis are common as the pulmonary damage pro-gresses (Fein &
Calalang-Colucci, 2000). This condition is sometimes referred to as acute
respiratory distress syndrome (ARDS), acute lung injury (ALI), shock lung, or
noncardiogenic pulmonary edema.
CARDIOVASCULAR EFFECTS
A lack of adequate blood supply leads to dysrhythmias and is-chemia. The
patient has a rapid heart rate, sometimes exceeding 150 bpm. The patient may
complain of chest pain and even suf-fer a myocardial infarction. Cardiac enzyme
levels (eg, lactate de-hydrogenase, CPK-MB, and cTn-I) rise. In addition,
myocardial depression and ventricular dilation may further impair the heart’s
ability to pump enough blood to the tissues to meet oxygen requirements.
NEUROLOGIC EFFECTS
As blood flow to the brain becomes impaired, the patient’s men-tal
status deteriorates. Changes in mental status occur as a re-sult of decreased
cerebral perfusion and hypoxia; the patient may initially exhibit confusion or
a subtle change in behavior. Subsequently, lethargy increases and the patient
begins to lose consciousness. The pupils dilate and are only sluggishly
reactive to light.
RENAL EFFECTS
When the MAP falls below
80 mm Hg (Guyton & Hall, 2000), the glomerular filtration rate of the
kidneys cannot be main-tained, and drastic changes in renal function occur.
Acute renal failure (ARF) can develop. ARF is characterized by an increase in
blood urea nitrogen (BUN) and serum creatinine levels, fluid and electrolyte
shifts, acid–base imbalances, and a loss of the renal-hormonal regulation of
blood pressure. Urinary output usually decreases to below 0.5/mL/kg per hour
(or below 30 mL per hour) but can be variable depending on the phase of ARF.
HEPATIC EFFECTS
Decreased blood flow to the liver impairs the liver cells’ ability to
perform metabolic and phagocytic functions. Consequently, the patient is less
able to metabolize medications and metabolic waste products, such as ammonia
and lactic acid. The patient becomes more susceptible to infection as the liver
fails to filter bacteria from the blood. Liver enzymes (aspartate
aminotransferase [AST], formerly serum glutamic-oxaloacetic transaminase
[SGOT]; alanine aminotransferase [ALT], formerly serum gluta-mate pyruvate
transaminase [SGPT]; lactate dehydrogenase) and bilirubin levels are elevated,
and the patient appears jaundiced.
GASTROINTESTINAL EFFECTS
Gastrointestinal ischemia can cause stress ulcers in the stomach,
placing the patient at risk for gastrointestinal bleeding. In the small
intestine, the mucosa can become necrotic and slough off, causing bloody
diarrhea. Beyond the local effects of impaired per-fusion, gastrointestinal
ischemia leads to bacterial toxin translo-cation, in which bacterial toxins
enter the bloodstream through the lymph system. In addition to causing
infection, bacterial tox-ins can cause cardiac depression, vasodilation,
increased capillary permeability, and an intense inflammatory response with
activation of additional biochemical mediators. The net result is inter-ference
with healthy cells and their ability to metabolize nutrients (Balk, 2000b;
Jindal et al., 2000).
HEMATOLOGIC EFFECTS
The combination of hypotension, sluggish blood flow, metabolic acidosis,
and generalized hypoxemia can interfere with normal hemostatic mechanisms.
Disseminated intravascular coagulation (DIC) can occur either as a cause or as
a complication of shock. In this condition, widespread clotting and bleeding
occur simul-taneously. Bruises (ecchymoses) and bleeding (petechiae) may
ap-pear in the skin. Coagulation times (prothrombin time, partial thromboplastin
time) are prolonged. Clotting factors and platelets are consumed and require
replacement therapy to achieve hemostasis.
Medical Management
Specific medical management in the progressive stage of shock depends on
the type of shock and its underlying cause. It is also based on the degree of
decompensation in the organ systems. Medical management specific to each type
of shock is discussed in later sections. Although there are several
differ-ences in medical management by type of shock, some medical
in-terventions are common to all types. These include use of appropriate
intravenous fluids and medications to restore tissue perfusion by (1)
optimizing intravascular volume, (2) supporting the pumping action of the
heart, and (3) improving the compe-tence of the vascular system. Other aspects
of management may include early enteral nutritional support and use of
antacids, histamine-2 blockers, or antipeptic agents to reduce the risk of
gastrointestinal ulceration and bleeding.
Nursing Management
Nursing care of the
patient in the progressive stage of shock re-quires expertise in assessing and
understanding shock and the sig-nificance of changes in assessment data. The
patient in the progressive stage of shock is often cared for in the intensive
care setting to facilitate close monitoring (hemodynamic monitoring,
electrocardiographic monitoring, arterial blood gases, serum elec-trolyte
levels, physical and mental status changes), rapid and fre-quent administration
of various prescribed medications and fluids, and possibly intervention with
supportive technologies, such as mechanical ventilation, dialysis, and
intra-aortic balloon pump.
Working closely with other members of the health care team, the nurse
carefully documents treatments, medications, and flu-ids that are administered
by members of the team, recording the time, dosage or volume, and the patient’s
response. Additionally, the nurse coordinates both the scheduling of diagnostic
proce-dures that may be carried out at the bedside and the flow of health care
personnel involved in the patient’s care.
PREVENTING COMPLICATIONS
If supportive technologies are used, the nurse helps reduce the risk of
related complications and monitors the patient for early signs of
complications. Monitoring includes evaluating blood lev-els of medications,
observing invasive vascular lines for signs of infection, and checking
neurovascular status if arterial lines are inserted, especially in the lower
extremities. Simultaneously, the nurse promotes the patient’s safety and
comfort by ensuring thatall procedures, including invasive procedures and
arterial and ve-nous punctures, are carried out using correct aseptic
techniques and that venous and arterial puncture and infusion sites are
main-tained with the goal of preventing infection. Positioning and
repositioning the patient to promote comfort, prevent pul-monary complications,
and maintain skin integrity are integral to caring for the patient in shock.
PROMOTING REST AND COMFORT
Efforts are made to minimize the cardiac workload by reducing the
patient’s physical activity and fear or anxiety. Promoting rest and comfort is
a priority in the patient’s care. To ensure that the patient gets as much
uninterrupted rest as possible, the nurse per-forms only essential nursing activities.
To conserve the patient’s energy, the nurse protects the patient from
temperature extremes (excessive warmth or shivering cold), which can increase
the metabolic rate and subsequently the cardiac workload. The pa-tient should
not be warmed too quickly, and warming blankets should not be applied because
they can cause vasodilation and a subsequent drop in blood pressure.
SUPPORTING FAMILY MEMBERS
Because the patient in shock is the object of intense attention by the
health care team, the family members may feel neglected; how-ever, they may be
reluctant to ask questions or seek information for fear that they will be in
the way or will interfere with the at-tention given to the patient. The nurse
should make sure that the family is comfortably situated and kept informed
about the pa-tient’s status. Often, family members need advice from the health
care team to get some rest; they are more likely to take this advice if they
feel that the patient is being well cared for and that they will be notified of
any significant changes in the patient’s status. A visit from the hospital
chaplain may be comforting to the family and provides some attention to the
family while the nurse concentrates on the patient.
IRREVERSIBLE STAGE
The irreversible (or refractory) stage of shock represents the point
along the shock continuum at which organ damage is so severe that the patient
does not respond to treatment and cannot sur-vive. Despite treatment, blood
pressure remains low. Complete renal and liver failure, compounded by the
release of necrotic tissue toxins, creates an overwhelming metabolic acidosis.
Anaer-obic metabolism contributes to a worsening lactic acidosis. Re-serves of
ATP are almost totally depleted, and mechanisms for storing new supplies of
energy have been destroyed. Multiple organ dysfunction progressing to complete
organ failure has oc-curred, and death is imminent. Multiple organ dysfunction
can occur as a progression along the shock continuum or as a syn-drome unto
itself.
Medical Management
Medical management during the irreversible stage of shock is usually the
same as for the progressive stage. Although the pa-tient’s condition may have
progressed from the progressive to the irreversible stage, the judgment that
the shock is irreversible can be made only retrospectively on the basis of the
patient’s failure to respond to treatment. Strategies that may be experimental
(ie, investigational medications, such as antibiotic agents and
immunomodulation therapy) may be tried to reduce or reverse the severity of
shock.
Nursing Management
As in the progressive
stage of shock, the nurse focuses on carry-ing out prescribed treatments,
monitoring the patient, preventing complications, protecting the patient from
injury, and providing comfort. Offering brief explanations to the patient about
what is happening is essential even if there is no certainty that the patient
hears or understands what is being said.
As it becomes obvious
that the patient is unlikely to survive, the family needs to be informed about
the prognosis and likely outcomes. Opportunities should be provided, throughout
the pa-tient’s care, for the family to see, touch, and talk to the patient. A
close family friend or spiritual advisor may be of comfort to the family in
dealing with the inevitable death of the patient. When-ever possible and
appropriate, the family should be approached regarding any living will, advance
directive, or other written or verbal wishes the patient may have shared in the
event that he or she cannot participate in end-of-life decisions. In some
cases, ethics committees may assist the family and health care team in making
difficult decisions.
During this stage of
shock, families may misinterpret the ac-tions of the health care team. They
have been told that nothing has been effective in reversing the shock and that
the patient’s sur-vival is very unlikely, yet the health care team continues to
work feverishly on the patient. A distraught, grieving family may inter-pret
this as a chance for recovery when none exists. As a result, family members may
become angry when the patient dies. Con-ferences with all members of the health
care team and the family will promote better understanding by the family of the
patient’s prognosis and the purpose for the measures being taken. During these
conferences, it is essential to explain that the equipment and treatments being
provided are for the patient’s comfort and do not suggest that the patient will
recover. Families should be encour-aged to express their wishes concerning the
use of life-support measures.
Related Topics