Chapter: Medical Surgical Nursing: Shock and Multisystem Failure
Septic Shock - Circulatory Shock
SEPTIC
SHOCK
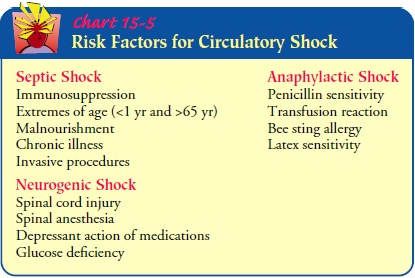
Septic shock is the most common type of circulatory shock and is caused
by widespread infection (Chart 15-5). Despite the in-creased sophistication of
antibiotic therapy, the incidence of sep-tic shock has continued to rise during
the past 60 years. It is the most common cause of death in noncoronary
intensive care units in the United States and the 13th leading cause of death
in the U.S. population (Balk, 2000a). Elderly patients are at particular risk
for sepsis because of decreased physiologic reserves and an aging immune system
(Balk, 2000a; Vincent & Ferreira, 2000).
Nosocomial infections (infections occurring in the hospital) in critically ill patients most frequently originate in the blood-stream, lungs, and urinary tract (in decreasing order of frequency) (Richards, Edwards, Culver et al., 1999). The source of infection is an important determinant of the clinical outcome. The great-est risk of sepsis occurs in patients with bacteremia (bloodstream) and pneumonia (Simon & Trenholme, 2000). Other infections that may progress to septic shock include intra-abdominal infec-tions, wound infections, bacteremia associated with intravascular catheters (Eggimann & Pittet, 2001), and indwelling urinary catheters.
Additional risk factors that contribute to the growing incidence of septic shock are the increased awareness and identification of septic shock; the increased number of immunocom-promised
patients (due to malnutrition, alcoholism, malignancy, and diabetes mellitus);
the increased incidence of invasive proce-dures and indwelling medical devices;
the increased number of resistant microorganisms; and the increasingly older
population (Balk, 2000a). The incidence of septic shock can be reduced by
débriding wounds to remove necrotic tissue and carrying out in-fection control
practices, including the use of meticulous aseptic technique, properly cleaning
and maintaining equipment, and using thorough hand-hygiene techniques.
The most common causative microorganisms of septic shock are the gram-negative bacteria; however, there is also an increased incidence of gram-positive bacterial infections. Currently, gram-positive bacteria are responsible for 50% of bacteremic events (Simon & Trenholme, 2000). Other infectious agents such as viruses and funguses also can cause septic shock.
When a microorganism
invades body tissues, the patient ex-hibits an immune response. This immune response
provokes the activation of biochemical mediators associated with an
inflam-matory response and produces a variety of effects leading to shock.
Increased capillary permeability, which leads to fluid seep-ing from the
capillaries, and vasodilation are two such effects that interrupt the ability
of the body to provide adequate perfusion, oxygen, and nutrients to the tissues
and cells.
Septic shock typically
occurs in two phases. The first phase, referred to as the hyperdynamic,
progressive phase, is character-ized by a high cardiac output with systemic
vasodilation. The blood pressure may remain within normal limits. The heart
rate increases, progressing to tachycardia. The patient becomes hyper-thermic
and febrile, with warm, flushed skin and bounding pulses. The respiratory rate
is elevated. Urinary output may remain at normal levels or decrease.
Gastrointestinal status may be compro-mised as evidenced by nausea, vomiting,
diarrhea, or decreased bowel sounds. The patient may exhibit subtle changes in mental
status, such as confusion or agitation.
The later phase, referred to as the hypodynamic, irreversible phase, is
characterized by low cardiac output with vasoconstriction, reflecting the
body’s effort to compensate for the hypovolemia caused by the loss of
intravascular volume through the capillaries. In this phase, the blood pressure
drops and the skin is cool and pale. Temperature may be normal or below normal.
Heart and res-piratory rates remain rapid. The patient no longer produces
urine, and multiple organ dysfunction progressing to failure develops.
Systemic inflammatory
response syndrome (SIRS) presents clinically like sepsis. The only difference
between SIRS and sep-sis is that there is no identifiable source of infection.
SIRS stim-ulates an overwhelming inflammatory immunologic and hormonal
response, similar to that seen in septic patients. Despite an absence of
infection, antibiotic agents may still be adminis-tered because of the
possibility of unrecognized infection. Addi-tional therapies directed to the
support of the patient with SIRS are similar to those for sepsis. If the
inflammatory process pro-gresses, septic shock may develop.
Medical Management
Current treatment of septic shock involves identifying and elim-inating
the cause of infection. Specimens of blood, sputum, urine, wound drainage, and
invasive catheter tips are collected for culture using aseptic technique.
Any potential routes of infection must be eliminated. Intra-venous lines
are removed and reinserted at other body sites. Antibiotic-coated intravenous
central lines may be placed to de-crease the risk of invasive line-related
bacteremia in high-risk pa-tients, such as the elderly (Eggimann & Pittet,
2001). If possible, urinary catheters are removed. Any abscesses are drained
and necrotic areas débrided.
Fluid replacement must be instituted to correct the hypo-volemia that
results from the incompetent vasculature and in-flammatory response.
Crystalloids, colloids, and blood products may be administered to increase the
intravascular volume.
PHARMACOLOGIC THERAPY
If the infecting organism is unknown, broad-spectrum antibiotic agents
are started until culture and sensitivity reports are received (Simon &
Trenholme, 2000). A third-generation cephalosporinplus an aminoglycoside may be
prescribed initially. This combi-nation works against most gram-negative and
some gram-positive organisms. When culture and sensitivity reports are
available, the antibiotic agent may be changed to one that is more specific to
the infecting organism and less toxic to the patient.
Research efforts show promise for improving the outcomes of septic
shock. Although past treatments focused on destroying the infectious organism,
emphasis is now on altering the patient’s im-mune response to the organism. The
cell walls of gram-negative bacteria contain a lipopolysaccharide, an endotoxin
released dur-ing phagocytosis (Abraham et al., 2001). Endotoxin and/or
gram-positive cell wall products interact with inflammatory bio-chemical
mediators, initiating an intense inflammatory response and systemic effects
that lead to shock. Current research focuses on the development of medications
that will inhibit or modulate the effects of biochemical mediators, such as
endotoxin and pro-calcitonin (Bernard, Vincent, Laterre, et al., 2001). The
focus on immunotherapy in treating septic shock is expected to shed light on
how the cellular response to infection leads to shock.
Recombinant human activated protein C (APC), or drotreco-gin alfa
(Xigris), has recently been demonstrated to reduce mor-tality in patients with
severe sepsis (Bernard, Artigas, Dellinger et al., 2001). It has been approved
by the U.S. Food and Drug Administration for treatment of adults with severe
sepsis and re-sulting acute organ dysfunction who are at high risk of death. It
acts as an antithrombotic, anti-inflammatory, and profibrinolytic agent. Its
most common serious side effect is bleeding. Therefore, it is contraindicated
in patients with active internal bleeding, re-cent hemorrhagic stroke, intracranial
surgery, or head injury.
NUTRITIONAL THERAPY
Aggressive nutritional supplementation is critical in the manage-ment of
septic shock because malnutrition further impairs the pa-tient’s resistance to
infection. Nutritional supplementation should be initiated within the first 24
hours of the onset of shock (Mizock, 2000). Enteral feedings are preferred to
the parenteral route be-cause of the increased risk of iatrogenic infection
associated with intravenous catheters; however, enteral feedings may not be possi-ble
if decreased perfusion to the gastrointestinal tract reduces peri-stalsis and
impairs absorption.
Nursing Management
The nurse caring for any patient in any setting must keep in mind the
risks of sepsis and the high mortality rate associated with sep-tic shock. All
invasive procedures must be carried out with aseptic technique after careful
hand hygiene. Additionally, intravenous lines, arterial and venous puncture
sites, surgical incisions, trau-matic wounds, urinary catheters, and pressure
ulcers are moni-tored for signs of infection in all patients. The nurse
identifies patients at particular risk for sepsis and septic shock (ie, elderly
and immunosuppressed patients or patients with extensive trauma or burns or
diabetes), keeping in mind that these high-risk patients may not develop
typical or classic signs of infection and sepsis. Confusion, for example, may
be the first sign of infection and sep-sis in elderly patients.
When caring for the
patient with septic shock, the nurse col-laborates with other members of the
health care team to identify the site and source of sepsis and the specific
organisms involved. Appropriate specimens for culture and sensitivity are often
ob-tained by the nurse.
Elevated body temperature (hyperthermia) is common with sepsis and
raises the patient’s metabolic rate and oxygen con-sumption. Fever is one of
the body’s natural mechanisms for fighting infections. Thus, an elevated
temperature may not be treated unless it reaches dangerous levels (more than
40C [104F]) or unless the patient is uncomfortable. Efforts may be made to
reduce the temperature by administering acetaminophen or applying hypothermia
blankets. During these therapies, the nurse monitors the patient closely for
shivering, which increases oxygen consumption. Efforts to increase comfort are
important if the patient experiences fever, chills, or shivering.
The nurse administers prescribed intravenous fluids and med-ications,
including antibiotic agents and vasoactive medications to restore vascular
volume. Because of decreased perfusion to the kidneys and liver, serum
concentrations of antibiotic agents that are normally cleared by these organs
may increase and produce toxic effects. Therefore, the nurse monitors blood
levels (anti-biotic agent, BUN, creatinine, white blood count) and reports
in-creased levels to the physician.
As with other types of
shock, the nurse monitors the patient’s hemodynamic status, fluid intake and
output, and nutritional sta-tus. Daily weights and close monitoring of serum
albumin levels help determine the patient’s protein requirements.
Related Topics