Chapter: Medical Surgical Nursing: Shock and Multisystem Failure
Cardiogenic Shock
Cardiogenic Shock
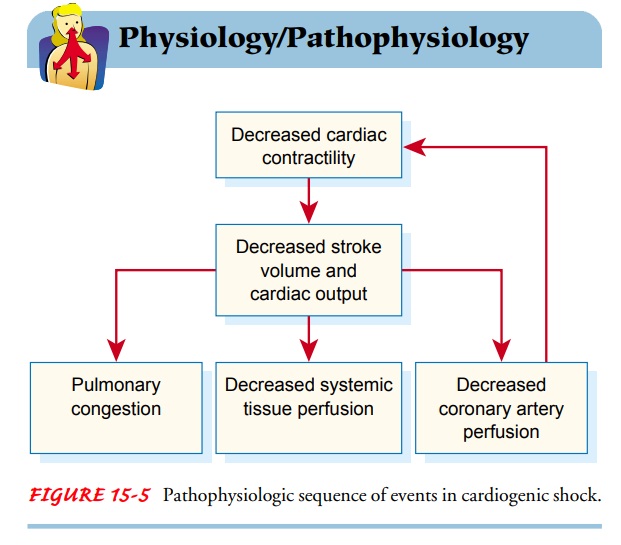
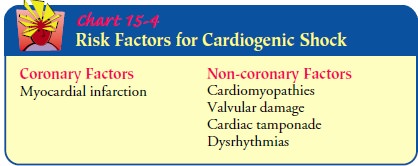
Cardiogenic shock occurs when the heart’s ability to contract and to pump blood is impaired and the supply of oxygen is inade-quate for the heart and tissues. The causes of cardiogenic shock are known as either coronary or noncoronary. Coronary cardio-genic shock is more common than noncoronary cardiogenic shock and is seen most often in patients with myocardial in-farction. Coronary cardiogenic shock occurs when a significant amount of the left ventricular myocardium has been destroyed (Price et al., 1999). Patients experiencing an anterior wall my-ocardial infarction are at the greatest risk for developing cardio-genic shock because of the potentially extensive damage to the left ventricle caused by occlusion of the left anterior descending coro-nary artery (Chart 15-4). Non-coronary causes can be related to severe metabolic problems (severe hypoxemia, acidosis, hypo-glycemia, and hypocalcemia) and tension pneumothorax.
Pathophysiology
In cardiogenic shock, cardiac output, which is a function of both stroke
volume and heart rate, is compromised. When stroke vol-ume and heart rate
decrease or become erratic, blood pressure drops and tissue perfusion is
compromised. Along with other tis-sues and organs being deprived of adequate
blood supply, the heart muscle itself receives inadequate blood. The result is
im-paired tissue perfusion. Because impaired tissue perfusion weak-ens the
heart and impairs its ability to pump blood forward, the ventricle does not
fully eject its volume of blood at systole. As a result, fluid accumulates in
the lungs. This sequence of events can occur rapidly or over a period of days
(Fig. 15-5).
Clinical Manifestations
Patients in cardiogenic shock may experience angina pain and develop
dysrhythmias and hemodynamic instability.
Medical Management
The goals of medical management are to (1) limit further myo-cardial
damage and preserve the healthy myocardium and (2) im-prove the cardiac function
by increasing cardiac contractility, decreasing ventricular afterload, or both
(Price et al., 1999). In general, these goals are achieved by increasing oxygen
supply to the heart muscle while reducing oxygen demands.
CORRECTION OF UNDERLYING CAUSES
As with all forms of shock, the underlying cause of cardiogenic shock must be corrected. It is necessary first to treat the oxygena-tion needs of the heart muscle to ensure its continued ability to pump blood to other organs. In the case of coronary cardiogenic shock, the patient may require thrombolytic therapy, angioplasty, or coronary artery bypass graft surgery. In the case of noncoro-nary cardiogenic shock, the patient may require a cardiac valve replacement or correction of a dysrhythmia.
INITIATION OF FIRST-LINE TREATMENT
First-line treatment of
cardiogenic shock involves the following actions:
· Supplying supplemental
oxygen
· Controlling chest pain
· Providing selected fluid
support
· Administering vasoactive
medications
· Controlling heart rate
with medication or by implementa-tion of a transthoracic or intravenous
pacemaker
· Implementing mechanical
cardiac support (intra-aortic bal-loon counterpulsation therapy, ventricular
assist systems, or extracorporeal cardiopulmonary bypass)
Oxygenation.
In
the early stages of shock, supplemental oxygen isadministered by nasal cannula
at a rate of 2 to 6 L/min to achieve an oxygen saturation exceeding 90%.
Monitoring arterial blood gas values and pulse oximetry values helps to indicate
whether the patient requires a more aggressive method of oxygen delivery.
Pain Control.
If
the patient experiences chest pain, morphine sul-fate is administered
intravenously for pain relief. In addition to relieving pain, morphine dilates
the blood vessels. This reduces the workload of the heart by both decreasing
the cardiac filling pressure (preload) and reducing the pressure against which
the heart muscle has to eject blood (afterload). Morphine also relieves the
patient’s anxiety. Cardiac enzyme (CPK-MB and cTn-I) lev-els are measured, and
serial 12-lead electrocardiograms are ob-tained to assess the degree of
myocardial damage.
Hemodynamic Monitoring.
Hemodynamic
monitoring is initi-ated to assess the patient’s response to treatment. In many
insti-tutions, this is performed in the intensive care unit, where an arterial
line can be inserted. The arterial line enables accurate and continuous
monitoring of blood pressure and provides a port from which to obtain frequent
arterial blood samples without having to perform repeated arterial punctures. A
multilumen pul-monary artery catheter is inserted to allow measurement of the
pulmonary artery pressures, myocardial filling pressures, cardiac output, and
pulmonary and systemic resistance.
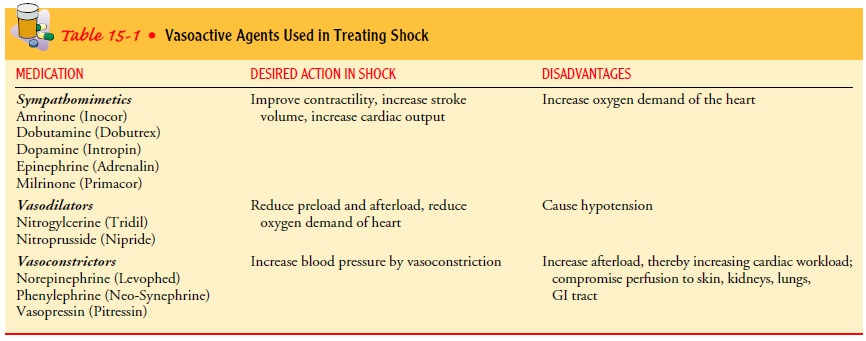
PHARMACOLOGIC THERAPY
Vasoactive medication
therapy consists of multiple pharmaco-logic strategies to restore and maintain
adequate cardiac output. In coronary cardiogenic shock, the aims of vasoactive
medication therapy are improved cardiac contractility, decreased preload and
afterload, or stable heart rate.
Because improving contractility and decreasing cardiac work-load are
opposing pharmacologic actions, two classifications of medications may be
administered in combination: sympath-omimetic agents and vasodilators. Sympathomimetic
medications increase cardiac output by mimicking the action of the sympa-thetic
nervous system through vasoconstriction, resulting in in-creased preload, and
by increasing myocardial contractility (inotropic action) or increasing the
heart rate (chronotropic ac-tion). Vasodilators are used to decrease preload
and afterload, thus reducing the workload of the heart and the oxygen demand.
Med-ications commonly combined to treat cardiogenic shock include dobutamine,
dopamine, and nitroglycerin (see Table 15-1).
Dobutamine.
Dobutamine
(Dobutrex) produces inotropic effectsby stimulating myocardial beta receptors,
increasing the strengthof myocardial activity and improving cardiac output.
Myocar-dial alpha-adrenergic receptors are also stimulated, resulting in
decreased pulmonary and systemic vascular resistance (decreased afterload).
Dobutamine enhances the strength of cardiac con-traction, improving stroke
volume ejection and overall cardiac output (Jindal et al., 2000; Price et al.,
1999).
Nitroglycerin.
Intravenous
nitroglycerin (Tridil) in low dosesacts as a venous vasodilator and therefore
reduces preload. At higher doses, nitroglycerin causes arterial vasodilation
and there-fore reduces afterload as well. These actions, in combination with
medium-dose dopamine, increase cardiac output while minimiz-ing cardiac
workload. Additionally, vasodilation enhances blood flow to the myocardium,
improving oxygen delivery to the weak-ened heart muscle (Price et al., 1999).
Dopamine.
Dopamine (Intropin) is a
sympathomimetic agentthat has varying vasoactive effects depending on the
dosage. It may be used with dobutamine and nitroglycerine to improve tissue
per-fusion. Low-dose dopamine (0.5 to 3.0 μg/kg/min)
increases renal and mesenteric blood flow, thereby preventing ischemia of these
organs because shock causes blood to be shunted away from the kidneys and the
mesentery. This dosage, however, does not im-prove cardiac output. Medium-dose
dopamine (4 to 8 μg/kg/min) has sympathomimetic properties and
improves contractility (ino-tropic action) and slightly increases the heart
rate (chronotropic action). At this dosage, dopamine increases cardiac output
and therefore is desirable. High-dose dopamine (8 to 10 μg/kg/min) predominantly causes vasoconstriction, which increases
afterload and thus increases cardiac workload. Because this effect is
unde-sirable in patients with cardiogenic shock, dopamine dosages must be
carefully titrated. Once the patient’s blood pressure stabilizes, low-dose
dopamine may be continued for its effect of promoting renal perfusion in
particular. In severe metabolic acidosis, which occurs in the later stages of
shock, dopamine’s effectiveness is di-minished. To maximize the effectiveness
of any vasoactive agent, metabolic acidosis must first be corrected. The
physician may pre-scribe intravenous sodium bicarbonate to treat the acidosis
(Jindal et al., 2000).
Other Vasoactive Medications.
Additional vasoactive agents thatmay be used in managing cardiogenic
shock include norepineph-rine (Levophed), epinephrine (Adrenalin), milrinone
(Primacor), amrinone (Inocor), vasopressin (Pitressin), and phenylephrine
(Neo-Synephrine). Each of these medications stimulates differ-ent receptors of
the sympathetic nervous system. A combination of these medications may be
prescribed, depending on the pa-tient’s response to treatment. All vasoactive
medications have ad-verse effects, making specific medications more useful than
others at different stages of shock. Diuretics such as furosemide (Lasix) may
be administered to reduce the workload of the heart by re-ducing fluid
accumulation (see Table 15-1).
Antiarrhythmic Medications.
Antiarrhythmic
medication is alsopart of the medication regimen in cardiogenic shock. Multiple
factors, such as hypoxemia, electrolyte imbalances, and acid–base imbalances,
contribute to serious cardiac dysrhythmias in all pa-tients with shock.
Additionally, as a compensatory response to de-creased cardiac output and blood
pressure, the heart rate increases beyond normal limits. This impedes cardiac
output further by shortening diastole and thereby decreasing the time for
ventricu-lar filling. Consequently, antiarrhythmic medications are re-quired to
stabilize the heart rate. For a full discussion of cardiac dysrhythmias as well
as commonly prescribed medications.
Fluid Therapy.
In
addition to medications, appropriate fluid isnecessary in treating cardiogenic
shock. Administration of fluids must be monitored closely to detect signs of
fluid overload. In-cremental intravenous fluid boluses are cautiously
administered to determine optimal filling pressures for improving cardiac
out-put. A fluid bolus should never be given quickly because rapid fluid
administration in patients with cardiac failure may result in acute pulmonary
edema.
MECHANICAL ASSISTIVE DEVICES
If cardiac output does not improve despite supplemental oxygen,
vasoactive medications, and fluid boluses, mechanical assistive de-vices are
used temporarily to improve the heart’s ability to pump. Intra-aortic balloon
counterpulsation is one means of providing temporary circulatory assistance. A
polyurethane balloon catheter is inserted percutaneously through the common
femoral artery and advanced into the descending thoracic aorta. The balloon
catheter is connected to a console containing a gas-filled pump. The timing of
the balloon inflation is synchronized electrocardiographically with the
beginning of diastole, and the balloon deflation occurs just before systole. The
goals of intra-aortic balloon counterpulsation include the following:
·
Increased stroke volume
·
Improved coronary artery perfusion
·
Decreased preload
·
Decreased cardiac workload
·
Decreased myocardial oxygen demand (Kumar et al.,
2000)
Other means of mechanical
assistance include left and right ventricular assist devices and total
artificial hearts. These devices are electrical pumps or pumps driven by air.
They assist or replace the ventricular pumping action of the heart. Human heart
trans-plantation may be the only option remaining for a patient who has
cardiogenic shock and who cannot be weaned from mechan-ical assistive devices.
Another short-term means
of providing cardiac or pulmonary support to the patient in cardiogenic shock
is through an extra-corporeal device similar to the cardiopulmonary bypass
(CPB) used in open-heart surgery. The CPB system requires systemic
anticoagulation, arterial and venous cannulation of the femoral artery and
vein, and connection to a centrifugal, oxygenated pump. The catheter tip is
advanced into the right atrium. This system lowers left and right ventricular
pressures, reducing the workload and oxygen needs of the heart. Complications
of CPB include coagulopathies, myocardial ischemia, infection, and
thromboembolism. CPB is used only in emergency situations until definitive
treatment, such as heart transplantation, can be initiated.
Nursing Management
PREVENTING CARDIOGENIC SHOCK
In some circumstances, identifying patients at risk early and pro-moting
adequate oxygenation of the heart muscle and decreasing cardiac workload can
prevent cardiogenic shock. This can be ac-complished by conserving the
patient’s energy, promptly reliev-ing angina, and administering supplemental
oxygen. Often, however, cardiogenic shock cannot be prevented. In such instances, nursing
management includes working with other mem-bers of the health care team to
prevent shock from progressing and to restore adequate cardiac function and
tissue perfusion.
MONITORING HEMODYNAMIC STATUS
A major role of the nurse is monitoring the patient’s hemo-dynamic and
cardiac status. Arterial lines and electrocardiographic monitoring equipment
must be maintained and functioning properly. The nurse anticipates the
medications, intravenous flu-ids, and equipment that might be used and is ready
to assist in implementing these measures. Changes in hemodynamic, cardiac, and
pulmonary status are documented and reported promptly. Additionally,
adventitious breath sounds, changes in cardiac rhythm, and other abnormal physical
assessment findings are re-ported immediately.
ADMINISTERING MEDICATIONS AND INTRAVENOUS FLUIDS
The nurse has a critical role in safe and accurate administration of
intravenous fluids and medications. Fluid overload and pul-monary edema are
risks because of ineffective cardiac function and accumulation of blood and
fluid in the pulmonary tissues. The nurse documents and records medications and
treatments that are administered as well as the patient’s response to
treatment.
The nurse needs to be knowledgeable about the desired effects as well as
the side effects of medications. For example, it is im-portant to monitor the
patient for decreased blood pressure after administering morphine or
nitroglycerin. The patient receiving thrombolytic therapy must be monitored for
bleeding. Arterial and venous puncture sites must be observed for bleeding and
pressure must be applied at the sites if bleeding occurs. Neuro-logic
assessment is essential after the administration of throm-bolytic therapy to
assess for the potential complication of cerebral hemorrhage associated with
the therapy. Intravenous infusions must be observed closely because tissue
necrosis and sloughing may occur if vasopressor medications infiltrate the
tissues. Urine output, BUN, and serum creatinine levels are monitored to
de-tect decreased renal function secondary to the effects of cardio-genic shock
or its treatment.
MAINTAINING INTRA-AORTIC BALLOON COUNTERPULSATION
The nurse plays a critical role in caring for the patient receiving
intra-aortic balloon counterpulsation. The nurse makes ongoing timing
adjustments of the balloon pump to max-imize its effectiveness by synchronizing
it with the cardiac cycle. The patient is at great risk for circulatory
compromise to the leg on the side where the catheter for the balloon has been
placed; therefore, the nurse must frequently check the neurovascular sta-tus of
the lower extremities.
ENHANCING SAFETY AND COMFORT
Throughout care, the nurse must take an active role in safe-guarding the
patient, enhancing comfort, and reducing anxiety. This includes administering
medication to relieve chest pain, pre-venting infection at the multiple
arterial and venous line insertion sites, protecting the skin, and monitoring
respiratory function. Proper positioning of the patient promotes effective
breathing without decreasing blood pressure and may also increase the
pa-tient’s comfort while reducing anxiety.
Brief explanations about
procedures that are being performed and the use of comforting touch often
provide reassurance to the patient and family. Families are usually anxious and
benefit from opportunities to see and talk to the patient. Explanations of
treat-ments and the patient’s response to them are often comforting to family
members.
Related Topics