Chapter: Medical Surgical Nursing: Shock and Multisystem Failure
Hypovolemic Shock
Hypovolemic Shock
In addition to caring for the patient through different stages of shock,
the nurse needs to tailor interventions to the type of shock, whether it is
hypovolemic, cardiogenic, or circulatory shock.
Hypovolemic shock, the
most common type of shock, is char-acterized by a decreased intravascular volume.
Body fluid is con-tained in the intracellular and extracellular compartments.
Intracellular fluid accounts for about two thirds of the total body water. The
extracellular body fluid is found in one of two com-partments: intravascular
(inside blood vessels) or interstitial (sur-rounding tissues). The volume of
interstitial fluid is about three to four times that of intravascular fluid.
Hypovolemic shock oc-curs when there is a reduction in intravascular volume of
15% to 25%. This would represent a loss of 750 to 1,300 mL of blood in a 70-kg
(154-lb) person.
Pathophysiology
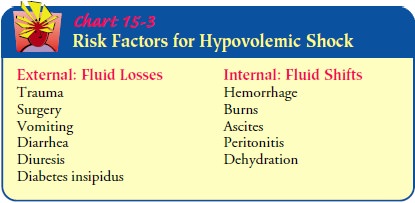
Hypovolemic shock can be caused by external fluid losses, such as
traumatic blood loss, or by internal fluid shifts, as in severe de-hydration,
severe edema, or ascites (Chart 15-3). Intravascular volume can be reduced both
by fluid loss and fluid shifting be-tween the intravascular and interstitial
compartments.
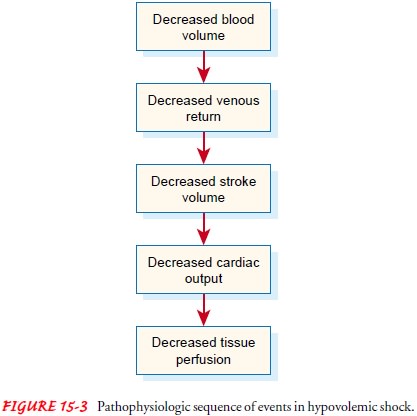
The sequence of events in hypovolemic shock begins with a decrease in
the intravascular volume. This results in decreased ve-nous return of blood to
the heart and subsequent decreased ven-tricular filling. Decreased ventricular
filling results in decreased stroke volume (amount of blood ejected from the
heart) and de-creased cardiac output. When cardiac output drops, blood pres-sure
drops and tissues cannot be adequately perfused (Fig. 15-3).
Medical Management
Major goals in treating hypovolemic shock are to (1) restore
in-travascular volume to reverse the sequence of events leading to inadequate
tissue perfusion, (2) redistribute fluid volume, andcorrect the underlying
cause of the fluid loss as quickly as pos-sible. Depending on the severity of
shock and the patient’s con-dition, it is likely that efforts will be made to address
all three goals simultaneously.
TREATMENT OF THE UNDERLYING CAUSE
If the patient is hemorrhaging, efforts are made to stop the bleed-ing.
This may involve applying pressure to the bleeding site or surgery to stop
internal bleeding. If the cause of the hypovolemia is diarrhea or vomiting,
medications to treat diarrhea and vomit-ing are administered as efforts are
made simultaneously to iden-tify and treat the cause. In the elderly patient,
dehydration may be the cause of hypovolemic shock.
FLUID AND BLOOD REPLACEMENT
Beyond reversing the primary cause of the decreased intravascular
volume, fluid replacement (also referred to as fluid resuscitation) is of
primary concern. At least two large-gauge intravenous lines are inserted to
establish access for fluid administration. Two intra-venous lines allow
simultaneous administration of fluid, medica-tions, and blood component therapy
if required. Because the goal of the fluid replacement is to restore
intravascular volume, it is nec-essary to administer fluids that will remain in
the intravascular com-partment and thus avoid creating fluid shifts from the
intravascular compartment into the intracellular compartment. Table 15-2
summarizes the fluids commonly used in treating shock.
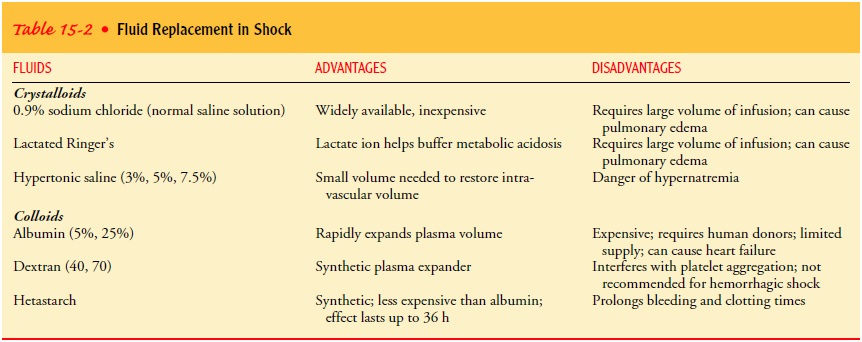
Lactated Ringer’s and 0.9% sodium chloride solutions are iso-tonic
crystalloid fluids commonly used in treating hypovolemic shock ( Jindal et al.,
2000). Large amounts of fluid must be ad-ministered to restore intravascular
volume because isotonic crys-talloid solutions move freely between the fluid
compartments of the body and do not remain in the vascular system.
Colloids (eg, albumin, hetastarch, and dextran) may also be used.
Dextran is not indicated if the cause of the hypovolemic shock is hemorrhage because
it interferes with platelet aggregation.
Blood products, also colloids, may need to be administered, particularly
when the cause of the hypovolemic shock is hemor-rhage. Because of the risk of
transmitting bloodborne viruses and the scarcity of blood products, however,
these products are used only if other alternatives are unavailable or blood
loss is extensive and rapid. Packed red blood cells are administered to
replenish the patient’s oxygen-carrying capacity in conjunction with other
fluids that will expand volume. Current recommendations are to base the need
for transfusions on the patient’s oxygenation needs, which are determined by
vital signs, blood gas values, and clini-cal appearance rather than using an
arbitrary laboratory value. Synthetic forms of blood (ie, compounds capable of
carrying oxy-gen in the same way that blood does) are potential alternatives.
REDISTRIBUTION OF FLUID
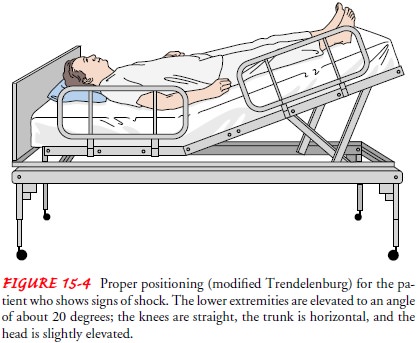
In addition to
administering fluids to restore intravascular vol-ume, positioning the patient
properly assists fluid redistribution. A modified Trendelenburg position (Fig.
15-4) is recommended in hypovolemic shock. Elevating the legs promotes the
return of venous blood. Positioning the patient in a full Trendelenburg
po-sition, however, makes breathing difficult and therefore is not recommended.
PHARMACOLOGIC THERAPY
If fluid administration
fails to reverse hypovolemic shock, then the same medications given in
cardiogenic shock are used because unreversed hypovolemic shock progresses to
cardiogenic shock (the vicious circle).
If the underlying cause of the hypovolemia is dehydration, medications
are also administered to reverse the cause of the de-hydration. For example,
insulin is administered if dehydration is secondary to hyperglycemia;
desmopressin (DDAVP) is admin-istered for diabetes insipidus, antidiarrheal
agents for diarrhea, and antiemetic medications for vomiting.
Nursing Management
Primary prevention of shock is an essential focus of nursing
inter-vention. Hypovolemic shock can be prevented in some instances by closely
monitoring patients who are at risk for fluid deficits and assisting with fluid
replacement before intravascular volume is de-pleted. In other circumstances,
hypovolemic shock cannot be pre-vented, and nursing care focuses on assisting with
treatment targeted at treating its cause and restoring intravascular volume.
General nursing measures include ensuring safe administra-tion of prescribed fluids and medications and documenting their administration and effects. Another important nursing role is monitoring for signs of complications and side effects of treat-ment and reporting these signs early in treatment.
ADMINISTERING BLOOD AND FLUIDS SAFELY
Administering blood transfusions safely is a vital nursing role. In
emergency situations, it is important to obtain blood specimens quickly to
obtain a baseline complete blood count and to type and cross-match the blood in
anticipation of blood transfusions. The patient who receives a transfusion of
blood products must be monitored closely for adverse effects.
Fluid replacement complications can occur, often when large volumes are
administered rapidly. Therefore, the nurse monitors the patient closely for
cardiovascular overload and pulmonary edema. The risk of these complications is
increased in the elderly and in patients with pre-existing cardiac disease.
Hemodynamic pressure, vital signs, arterial blood gases, hemoglobin and
hemat-ocrit levels, and fluid intake and output are among the parameters
monitored. The patient’s temperature should also be monitored closely to ensure
that rapid fluid resuscitation does not precipi-tate hypothermia. Intravenous
fluids may need to be warmed during the administration of large volumes.
Physical assessment focuses on observing the jugular veins for distention and
moni-toring jugular venous pressure. Jugular venous pressure is low in
hypovolemic shock; it increases with effective treatment and is significantly
increased with fluid overload and heart failure. The nurse needs to monitor cardiac
and respiratory status closely and report changes in blood pressure, pulse
pressure, heart rate, rhythm, and lung sounds to the physician.
IMPLEMENTING OTHER MEASURES
Oxygen is administered to increase the amount of oxygen car-ried by
available hemoglobin in the blood. A patient who is con-fused may feel
apprehensive with an oxygen mask or cannula in place, and frequent explanations
about the need for the mask may reduce some of the patient’s fear and anxiety.
Simultane-ously, the nurse must direct efforts to the safety and comfort of the
patient.
Related Topics