Chapter: Medical Surgical Nursing: Management of Patients With HIV Infection and AIDS
Stages of HIV Disease
Stages
of HIV Disease
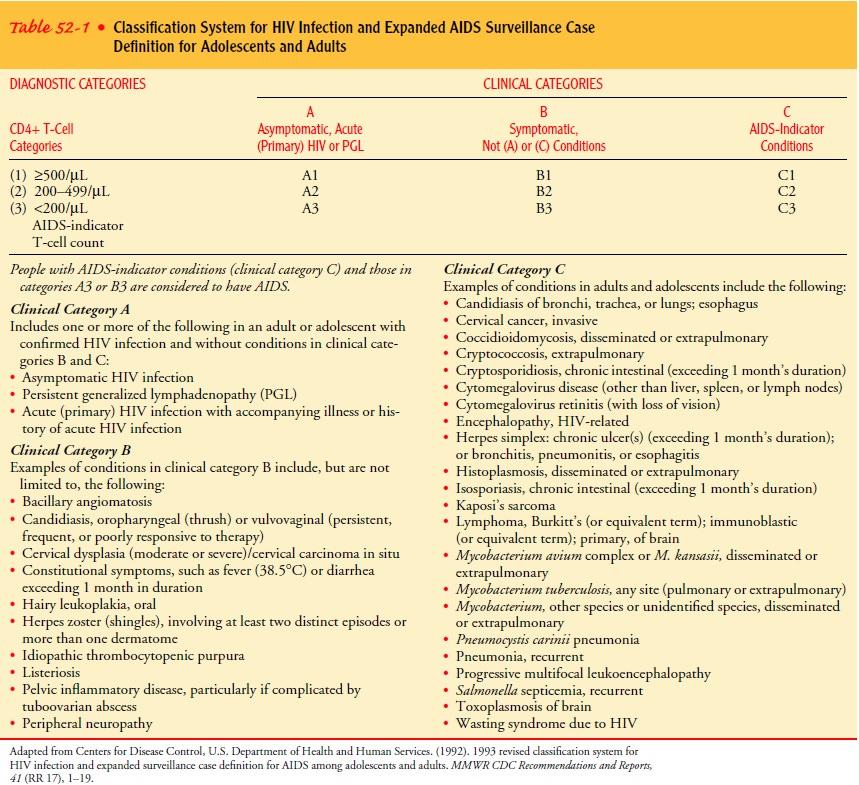
The stage of HIV disease is based on clinical
history, physical ex-amination, laboratory evidence of immune dysfunction,
signs and symptoms, and infections and malignancies. The CDC stan-dard case
definition of AIDS categorizes HIV infection and AIDS in adults and adolescents
on the basis of clinical conditions asso-ciated with HIV infection and CD4+ T-cell counts. The
classifi-cation system (Table 52-1) groups clinical conditions into one of
three categories denoted as A, B, or C.
PRIMARY INFECTION (ALSO KNOWN AS ACUTE HIV INFECTION OR ACUTE HIV SYNDROME)
The period from infection with HIV to the
development of anti-bodies to HIV is known as primary infection. During this pe-riod, there is intense viral
replication and widespread dissemination of HIV throughout the body. Symptoms
associated with theviremia range from none to severe flu-like symptoms. During
the primary infection period, the window period occurs because a person is
infected with HIV but tests negative on the HIV anti-body blood test. Although
antibodies to the HIV envelope glyco-proteins typically can be detected in the
sera of HIV-infected individuals by 2 to 3 weeks after infection, most of these
anti-bodies lack the ability to inhibit virus infection. By the time
neu-tralizing antibodies are detected, HIV-1 is firmly established in the host
(Wyatt & Sodroski, 1998). During this period, there are high levels of
viral replication and the killing of CD4 T cells, re-sulting in high levels of
HIV in the blood and a dramatic drop in CD4 T cell counts from the normal level
of at least 800 cells/mm3 of blood. About 3 weeks into this acute phase, individuals may display
symptoms reminiscent of mononucleosis, such as fever, enlarged lymph nodes, rash,
muscle aches, and headaches. These symptoms resolve within another 1 to 3 weeks
as the immune sys-tem begins to gain some control over the virus. That is, the
CD4 T-cell population responds in ways that spur other immune cells, such as
CD8 lymphocytes, to increase their killing of infected, virus-producing cells.
The body produces antibody molecules in an effort to contain the virus; they
bind to free HIV particles (outside cells) and assist in their removal
(Bartlett & Moore, 1998). This balance between the amount of HIV in the
body and the immune response is referred to as the viral set point and re-sults in a steady state of infection. During
this steady state, which can last for years, the amount of virus in circulation
and the num-ber of infected cells equal the rate of viral clearance (Ropka
& Williams, 1998).
Primary HIV infection, the time during which
the viral burden set point is achieved, includes the acute symptomatic and
early in-fection phases. During this initial stage, viral replication is
asso-ciated with dissemination in lymphoid tissue and a distinct immunologic
response. The final level of the viral set point is in-versely correlated with
disease prognosis; that is, the higher the viral set point, the poorer the
prognosis (Cates, Chesney & Cohen, 1997). The primary infection stage is
part of CDC category A.
HIV ASYMPTOMATIC (CDC CATEGORY A:MORE
THAN 500 CD4+ T LYMPHOCYTES/MM3)
On
reaching a viral set point, a chronic, clinically asymptomatic state begins.
Despite its best efforts, the immune system rarely if ever fully eliminates the
virus. By about 6 months, the rate of viral replication reaches a lower but
relatively steady state that is re-flected in the maintenance of viral levels
at a kind of “set point.” This set point varies greatly from patient to patient
and dictates the subsequent rate of disease progression; on average, 8 to 10
years pass before a major HIV-related complication develops. In this prolonged,
chronic stage, patients feel well and show few if any symptoms (Bartlett &
Moore, 1998). Apparent good health con-tinues because CD4 T-cell levels remain
high enough to preserve defensive responses to other pathogens.
HIV SYMPTOMATIC (CDC CATEGORY B: 200
TO 499 CD4+ T LYMPHOCYTES/MM3)
Over time, the number of CD4 T cells gradually falls. Category B consists of symptomatic conditions in HIV-infected patients that are not included in the conditions listed in category C. These conditions must also meet one of the following criteria: (1) the condition is due to HIV infection or a defect in cellular immu-nity, or (2) the condition must be considered to have a clinical course or require management that is complicated by HIV infec-tion. If an individual was once treated for a category B condition and has not developed a category C disease but is now symptom-free, that person’s illness would be considered category B
AIDS (CDC CATEGORY C: LESS THAN 200
CD4+ T LYMPHOCYTES/MM3)
When CD4 T-cell levels drop below 200
cells/mm3
of blood, pa-tients are said to have AIDS. As levels fall below 100, the immune
system is significantly impaired (Bartlett & Moore, 1998). Once a patient
has had a category C condition, he or she remains in cat-egory C. This
classification has implications for entitlements (ie, disability benefits,
housing, and food stamps) since these pro-grams are often linked to an AIDS
diagnosis. Although the re-vised classification emphasizes CD4+ T-cell counts, it
allows for CD4+ percentages (percentage of CD4+ T cells of total lympho-cytes). The CD4+ percentage is less
subject to variation on re-peated measurements than is the absolute CD4+ T-cell count. Less than
14% of the CD4+ T cells of the total lymphocytes is consistent with an AIDS diagnosis.
The percentage, as compared to the absolute number of CD4+ T cells, becomes
particularly important when the patient has a heightened immune response to
infections in addition to HIV. One complication of advanced HIV infection is anemia,
which may be caused by HIV, oppor-tunistic diseases, and medications (Collier
et al., 2001).
Related Topics