Chapter: Medical Surgical Nursing: Management of Patients With HIV Infection and AIDS
HIV Infection and AIDS: Epidemiology and HIV Transmission
HIV Infection and AIDS
Since acquired immunodeficiency syndrome
(AIDS) was first rec-ognized more than 20 years ago, remarkable progress has
been made in improving the quality and duration of life of persons with HIV infection. During the first decade, this progress was asso-ciated with recognition of opportunistic
disease processes, more ef-fective therapy for complications, and introduction
of prophylaxis against common opportunistic infections (OIs). The second decade
has witnessed progress in developing highly active anti-retroviral therapies
(HAART) as well as continuing progress in treating OIs (Masur, Kaplan &
Holmes, 1999). Since the HIV serologic test (enzyme immunoassay [EIA], formerly
enzyme-linked immunosorbent assay [ELISHA]), became available in 1984, allow-ing
early diagnosis of the infection before onset of symptoms, HIV infection has
been best managed as a chronic disease and most ap-propriately managed in an
outpatient care setting (Gallant, 2001).
Epidemiology
In fall 1982, the Centers for Disease Control
and Prevention (CDC) issued a case definition of AIDS after the first 100 cases
were reported. Since then, the CDC has revised the case defini-tion a number of
times (1985, 1987, and 1993). All 50 states, the District of Columbia, U.S.
dependencies and possessions, and in-dependent nations in free association with
the United States re-port AIDS cases to the CDC using a uniform surveillance
case definition and case report form (CDC, 2000). Starting in the late 1990s,
more states started to implement HIV case reporting in response to the changing
epidemic and the need for information on persons with HIV infection who have
not developed AIDS.
As of
December 2001, there were 816,149 reported cases of HIV/AIDS and 506,154
adults, adolescents, and children in the United States (including U. S.
dependencies, possessions, and as-sociated nations) living with AIDS.
Unprotected sex and sharing of injection drug use equipment are the major means
of trans-mission of HIV. A total of 43,158 AIDS cases were diagnosed in 2001. For
men diagnosed with AIDS during 2001, 59% were in the exposure category of men
who have sex with men; 24% in injection drug use; and 7% in heterosexual
contact. In women diagnosed with AIDS during that same period, 44% reported
in-jection drug use and 52% reported heterosexual contact. Com-paring race/
ethnicity among the three largest groups diagnosed in 2001, 20,752 were black,
not Hispanic; 11,675 were Caucasian; and 8,221 were Hispanic (CDC, 2002).
The
number of people living with AIDS is not evenly distrib-uted throughout the
United States. States with the largest num-ber of reported AIDS cases during
2001 were New York (7,476), Florida (5,138), California (4,315), Texas (2,892),
and Maryland (1,860) (CDC, 2002).
AIDS has reached epidemic proportions in some
other parts of the world. According to the Joint United Nations Programme on
HIV/AIDS, more than 18.8 million people worldwide have died of AIDS and 34.3
million people are infected with HIV, with 5.4 million people newly infected
with HIV in 1999 alone (Letvin, Bloom & Hoffman, 2001). UNAIDS (2001)
reports that since the epidemic began, more than 60 million people have been
infected with the virus, making it the most devastating disease ever.
The earliest confirmed case of HIV infection
was found in blood drawn from an African man in 1959 (Stephenson, 1998).
Although factors associated with the spread of HIV in Africa re-main unknown,
possibilities include the reuse of unsterilized nee-dles in large-scale
vaccination campaigns that began in Africa in the 1960s; however, social
changes such as easier access to trans-portation, increasing population
density, and more frequent sex-ual contacts may have been more important
(Stephenson, 1998).
HIV Transmission
HIV-1 is transmitted in body fluids containing HIV and/or in-fected CD4+ (or CD4) T lymphocytes.
These fluids include blood, seminal fluid, vaginal secretions, amniotic fluid,
and breast milk. Mother-to-child transmission of HIV-1 may occur in utero, at
the time of delivery, or through breastfeeding, but transmission frequency
during each period has been difficult to determine (Nduati et al., 2000). Any
behavior that results in breaks in the skin or mucosa results in the increased
probability of exposure to HIV (Chart 52-1). Since HIV is harbored within
lymphocytes, a type of white blood cell, any exposure to infected blood results
in a significant risk of infection. The amount of virus and infected cells in
the body fluid is associated with the risk of new infections.
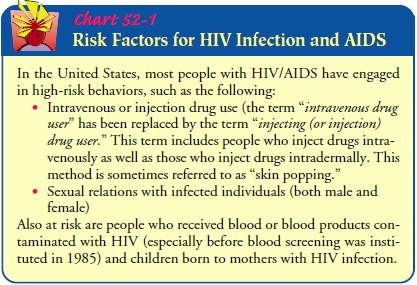
Blood and blood products can transmit HIV to recipients. However, the risk associated with transfusions has been virtually eliminated as a result of voluntary self-deferral, serologic testing, heat treatment of clotting factor concentrates, and more effective virus inactivation methods. Blood donor screening tests detect antibodies to HIV-1 and HIV-2, and p24 antigen testing has been added as an interim measure (American Red Cross, 2001). However, blood donated during the window period will be in-fectious but will test negative for HIV antibodies. The window pe-riod is the period of time between initial infection of HIV and development of a positive antibody test for HIV. Although anti-bodies will usually be detected within 3 to 6 months, the window period can last up to a year.
Related Topics