Chapter: Medical Surgical Nursing: Management of Patients With HIV Infection and AIDS
HIV Infection and AIDS: Transmission to Health Care Providers
Transmission
to Health Care Providers
STANDARD PRECAUTIONS
In
1996, efforts were made by the CDC and its Hospital Infec-tion Control
Practices Advisory Committee (HICPAC) to stan dardize procedures and reduce the
risk for exposure through de-velopment of Standard Precautions. Standard
Precautions in-corporate the major features of Universal Precautions (designed
to reduce the risk of transmission of blood-borne pathogens) and Body Substance
Isolation (designed to reduce the risk of transmission of pathogens from moist
body substances); they are applied to all patients receiving care in hospitals
regardless of their diagnosis or presumed infectious status (Chart 52-3).
Standard Precautions apply to blood; all body fluids, secre-tions, and
excretions, except sweat, regardless of whether they contain visible blood;
nonintact skin; and mucous membranes (Hospital Infection Control Practices
Advisory Committee [HICPAC], 1996).
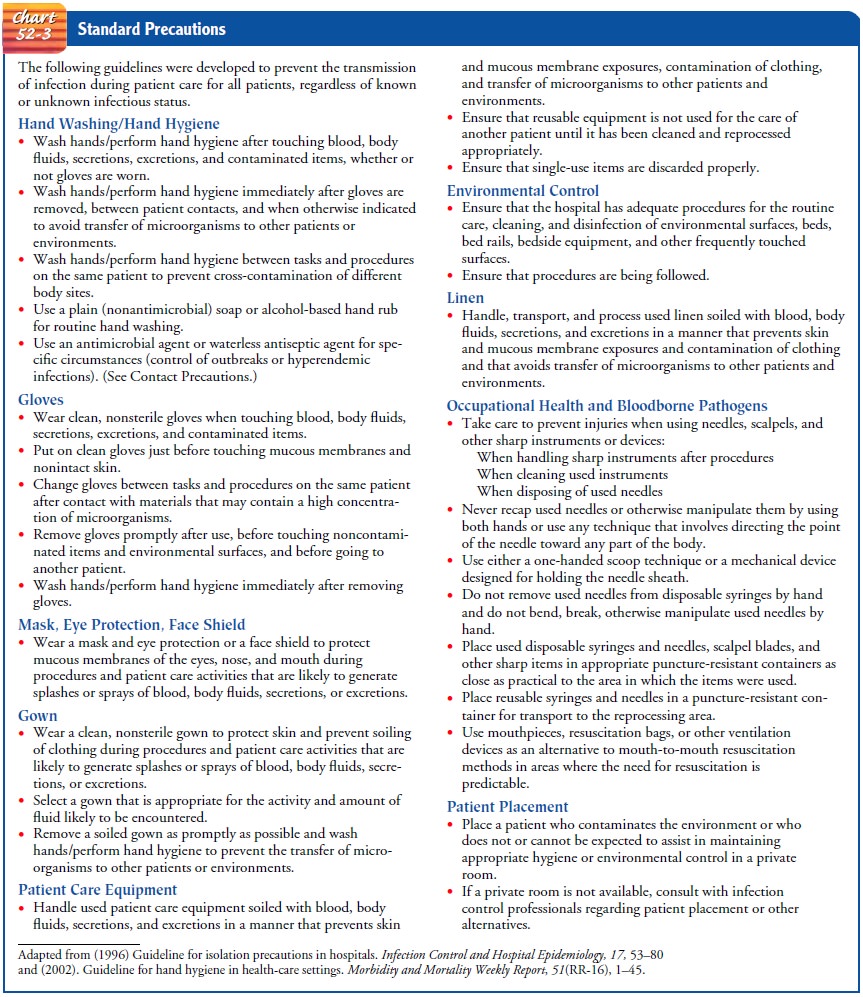
The primary goal of Standard Precautions is
to prevent the transmission of nosocomial infection. The first tier, referred
to as Standard Precautions, was developed to reduce the risk for all
rec-ognized or unrecognized sources of infections in hospitals. A sec-ond tier
for infection control precautions for specified conditions, called
Transmission-Based Precautions, was designed for use in addition to Standard
Precautions for patients with documented or suspected infections involving
highly transmissible pathogens. The three types of Transmission-Based
Precautions are referred to as Airborne Precautions, Droplet Precautions, and Contact
Precautions. They can be used singularly or in combination, but they are always
to be used in addition to Standard Precautions (HICPAC, 1997).
Large-scale studies of exposed health care
workers continue to be conducted by the CDC and other groups. In November 2000,
the Needlestick Safety and Prevention Act became law, mandat-ing health care
facilities to use devices to protect against sharps injuries (Worthington,
2001).
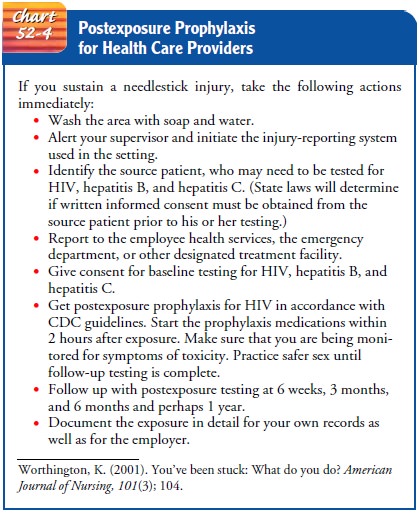
POSTEXPOSURE PROPHYLAXIS FOR HEALTH CARE PROVIDERS
Postexposure
prophylaxis in response to exposure of health care personnel to blood or other
body fluids has been proven to reduce the risk for HIV infection (Worthington,
2001). The CDC (1998) recommends that all health care providers who have
sus-tained a significant exposure to HIV be counseled and offered anti-HIV
postexposure prophylaxis, if appropriate. Some clini-cians are considering
using postexposure prophylaxis for patients exposed to HIV from high-risk
sexual behavior or possible con-tact through injection drug use. This use of
postexposure pro-phylaxis is controversial because of concern that it may be
substituted for safer sex practices and safer injection drug use. Postexposure
prophylaxis should not be considered an acceptable method of preventing HIV
infection.
The medications recommended for postexposure
prophylaxis are those used to treat established HIV infection. Ideally,
pro-phylaxis needs to start immediately after exposure; therapy started more
than 72 hours after exposure is thought to offer no benefit.
The recommended course of therapy involves taking the pre-scribed mediations for 4 weeks. Those who choose postexposure prophylaxis must be prepared for the side effects of the medica-tions and must be willing to face the unknown long-term risks, because HIV often becomes resistant to the medications used to treat it. If the person becomes infected despite prophylaxis, viral drug resistance may reduce future treatment options. The cost is also of concern; the cost of a drug regimen ranges from $500 to more than $1,000, plus the costs of testing and counseling. Health insurance generally does not cover the costs of medica-tions, laboratory tests, and counseling (Chart 52-4).
Related Topics