Chapter: Medical Surgical Nursing: Management of Patients With HIV Infection and AIDS
Nursing Process: The Patient With AIDS
NURSING
PROCESS:THE PATIENT WITH AIDS
The
nursing care of patients with AIDS is challenging because of the potential for
any organ system to be the target of infections or cancer. In addition, this
disease is complicated by many emo-tional, social, and ethical issues. The plan
of care for the patient with AIDS is individualized to meet the needs of the
patient (see Plan of Nursing Care). Care includes many of the interventions and
concerns cited in the supportive care section.
Assessment
Nursing
assessment includes identification of potential risk fac-tors, including a
history of risky sexual practices and injection drug use. The patient’s
physical status and psychological status are assessed. All factors affecting
immune system functioning are thoroughly explored.
NUTRITIONAL STATUS
Nutritional status is assessed by obtaining a
dietary history and identifying factors that may interfere with oral intake,
such as anorexia, nausea, vomiting, oral pain, or difficulty swallowing. In
addition, the patient’s ability to purchase and prepare food is as-sessed.
Weight, anthropometric measurements, and blood urea nitrogen (BUN), serum
protein, albumin, and transferrin levels provide objective measurements of
nutritional status.
SKIN INTEGRITY
The
skin and mucous membranes are inspected daily for evi-dence of breakdown,
ulceration, or infection. The oral cavity is monitored for redness,
ulcerations, and the presence of creamy-white patches indicative of
candidiasis. Assessment of the peri-anal area for excoriation and infection in
patients with profuse diarrhea is important. Wounds are cultured to identify
infectious organisms.
RESPIRATORY STATUS
Respiratory
status is assessed by monitoring the patient for cough, sputum production,
shortness of breath, orthopnea, tachypnea, and chest pain. The presence and
quality of breath sounds are in-vestigated. Other measures of pulmonary
function include chest x-ray results, arterial blood gas values, pulse
oximetry, and pul-monary function test results.
NEUROLOGIC STATUS
Neurologic
status is determined by assessing level of conscious-ness; orientation to
person, place, and time; and memory lapses. Mental status is assessed as early
as possible to provide a baseline (Chart 52-6). The patient is also assessed
for sensory deficits (visual changes, headache, or numbness and tingling in the
ex-tremities) and motor involvement (altered gait, paresis, or paral-ysis) and
seizure activity.
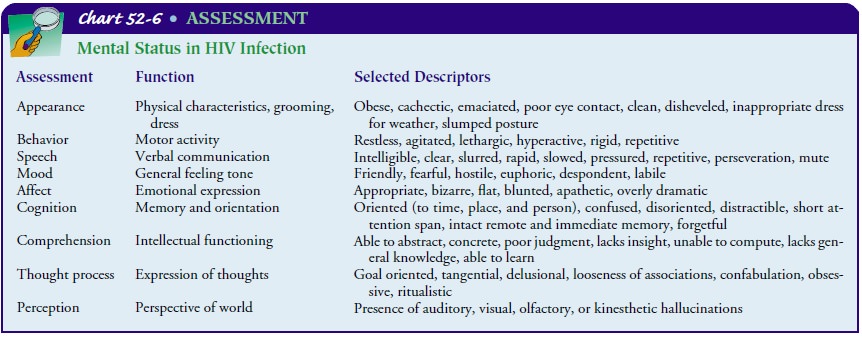
FLUID AND ELECTROLYTE BALANCE
Fluid and electrolyte status is assessed by
examining the skin and mucous membranes for turgor and dryness. Increased
thirst, de-creased urine output, low blood pressure or a decrease in systolic
blood pressure between 10 and 15 mm Hg with a concurrent rise in pulse rate
when the patient sits up or stands, weak and rapid pulse, and urine specific
gravity of 1.025 or more may indicate dehydration. Electrolyte imbalances, such
as decreased serum sodium, potassium, calcium, magnesium, and chloride,
typically result from profuse diarrhea. The patient is assessed for signs and
symptoms of electrolyte deficits, including decreased mental sta-tus (see Chart
52-6), muscle twitching, muscle cramps, irregular pulse, nausea and vomiting,
and shallow respirations.
KNOWLEDGE LEVEL
The patient’s level of knowledge about the disease and the modes of disease transmission is evaluated. In addition, the level of knowledge of family and friends is assessed. The patient’s psy-chological reaction to the diagnosis of HIV infection or AIDS is important to explore. Reactions vary among patients and may in-clude denial, anger, fear, shame, withdrawal from social interac-tions, and depression. It is often helpful to gain an understanding of how the patient has dealt with illness and major life stress in the past. The patient’s resources for support are also identified.
Diagnosis
NURSING DIAGNOSES
The
list of potential nursing diagnoses is extensive because of the complex nature
of this disease. Based on assessment data, how-ever, major nursing diagnoses
for the patient may include the following:
· Impaired skin integrity
related to cutaneous manifestations of HIV infection, excoriation, and diarrhea
· Diarrhea related to
enteric pathogens or HIV infection
· Risk for infection
related to immunodeficiency
· Activity intolerance
related to weakness, fatigue, malnutri-tion, impaired fluid and electrolyte
balance, and hypoxia as-sociated with pulmonary infections
· Disturbed thought
processes related to shortened attention span, impaired memory, confusion, and
disorientation as-sociated with HIV encephalopathy
· Ineffective airway
clearance related to PCP, increased bron-chial secretions, and decreased
ability to cough related to weakness and fatigue
· Pain related to impaired
perianal skin integrity secondary to diarrhea, KS, and peripheral neuropathy
· Imbalanced nutrition,
less than body requirements, related to decreased oral intake
· Social isolation related
to stigma of the disease, withdrawal of support systems, isolation procedures,
and fear of infect-ing others
· Anticipatory grieving
related to changes in lifestyle and roles and unfavorable prognosis
· Deficient knowledge
related to HIV infection, means of preventing HIV transmission, and self-care
COLLABORATIVE PROBLEMS/POTENTIAL COMPLICATIONS
Based
on the assessment data, possible complications may include the following:
· Opportunistic infections
· Impaired breathing or
respiratory failure
· Wasting syndrome and
fluid and electrolyte imbalance
Adverse reaction to medications
Planning and Goals
Goals for the patient may include achievement
and maintenance of skin integrity, resumption of usual bowel habits, absence of
in-fection, improved activity tolerance, improved thought processes, improved
airway clearance, increased comfort, improved nutri-tional status, increased
socialization, expression of grief, increased knowledge regarding disease
prevention and self-care, and ab-sence of complications.
Nursing Interventions
PROMOTING SKIN INTEGRITY
The skin and oral mucosa are assessed
routinely for changes in ap-pearance, location and size of lesions, and
evidence of infection and breakdown. The patient is encouraged to maintain a
balance between rest and mobility whenever possible. Patients who are immobile
are assisted to change position every 2 hours. Devices such as
alternating-pressure mattresses and low-air-loss beds are used to prevent skin
breakdown. Patients are encouraged to avoid scratching, to use nonabrasive,
nondrying soaps, and to apply nonperfumed skin moisturizers to dry skin
surfaces. Regular oral care is also encouraged.
Medicated lotions, ointments, and dressings
are applied to af-fected skin surfaces as prescribed. Adhesive tape is avoided.
Skin surfaces are protected from friction and rubbing by keeping bed linens
free of wrinkles and avoiding tight or restrictive clothing. Patients with foot
lesions are advised to wear cotton socks and shoes that do not cause the feet
to perspire. Antipruritic, anti-biotic, and analgesic agents are administered
as prescribed.
The perianal region is assessed frequently
for impairment of skin integrity and infection. The patient is instructed to
keep the area as clean as possible. The perianal area is cleaned after each
bowel movement with nonabrasive soap and water to prevent further excoriation
and breakdown of the skin and infection. If the area is very painful, soft
cloths or cotton sponges may prove to be less irritating than washcloths. In
addition, sitz baths or gentle irrigation may facilitate cleaning and promote
comfort. The area is dried thoroughly after cleaning. Topical lotions or
ointments may be prescribed to promote healing. Wounds are cultured if
in-fection is suspected so that the appropriate antimicrobial treat-ment can be
initiated. Debilitated patients may require assistance in maintaining hygienic
practices.
PROMOTING USUAL BOWEL HABITS
Bowel patterns are assessed for diarrhea. The
nurse monitors the frequency and consistency of stools and reports of abdominal
pain or cramping associated with bowel movements. Factors that ex-acerbate
frequent diarrhea are also assessed. The quantity and vol-ume of liquid stools
are measured to document fluid volume losses. Stool cultures are obtained to
identify pathogenic organisms.
The patient is counseled about ways to
decrease diarrhea. The physician may recommend restriction of oral intake to
rest the bowel during periods of acute inflammation associated with se-vere
enteric infections. As the patient’s dietary intake is increased, foods that
act as bowel irritants, such as raw fruits and vegetables, popcorn, carbonated
beverages, spicy foods, and foods of extreme temperatures, should be avoided.
Small, frequent meals help to prevent abdominal distention. The physician may
prescribe med-ications such as anticholinergic antispasmodics or opioids, which
decrease diarrhea by decreasing intestinal spasms and motility. Administering
antidiarrheal agents on a regular schedule may be more beneficial than
administering them on an as-needed basis. Antibiotics and antifungal agents may
also be prescribed to com-bat pathogens identified by stool cultures. The nurse
should also assess the self-care strategies being used by the patient to
control diarrhea (Henry et al., 1999).
PREVENTING INFECTION
The patient and caregivers are instructed to
monitor for signs and symptoms of infection: fever; chills; night sweats; cough
with or without sputum production; shortness of breath; difficulty breath-ing;
oral pain or difficulty swallowing; creamy-white patches in the oral cavity;
unexplained weight loss; swollen lymph nodes; nausea; vomiting; persistent
diarrhea; frequency, urgency, or pain on urination; headache; visual changes or
memory lapses; redness, swelling, or drainage from skin wounds; and vesicular
lesions on the face, lips, or perianal area. The nurse also monitors laboratory
values that indicate infection, such as the white blood cell count and
differential. The physician may decide to culture specimens of wound drainage,
skin lesions, urine, stool, sputum, mouth, and blood to identify pathogenic
organisms and the most appropriate antimicrobial therapy. The patient is
instructed to avoid others with active infections such as upper respiratory
infections.
IMPROVING ACTIVITY TOLERANCE
Activity
tolerance is assessed by monitoring the patient’s ability to ambulate and
perform activities of daily living. Patients may be unable to maintain their
usual levels of activity because of weakness, fatigue, shortness of breath,
dizziness, and neurologic involvement. Assistance in planning daily routines
that maintain a balance between activity and rest may be necessary. In
addition, patients benefit from instructions about energy conservation
techniques, such as sitting while washing or while preparing meals. Personal
items that are frequently used should be kept within the patient’s reach.
Measures such as relaxation and guided imagery may be beneficial because they
decrease anxiety, which contributes to weakness and fatigue.
Collaboration
with other members of the health care team may uncover other factors associated
with increasing fatigue and strategies to address them. For example, if fatigue
is related to anemia, administering epoetin alfa (Epogen) as prescribed may
relieve fatigue and increase activity tolerance.
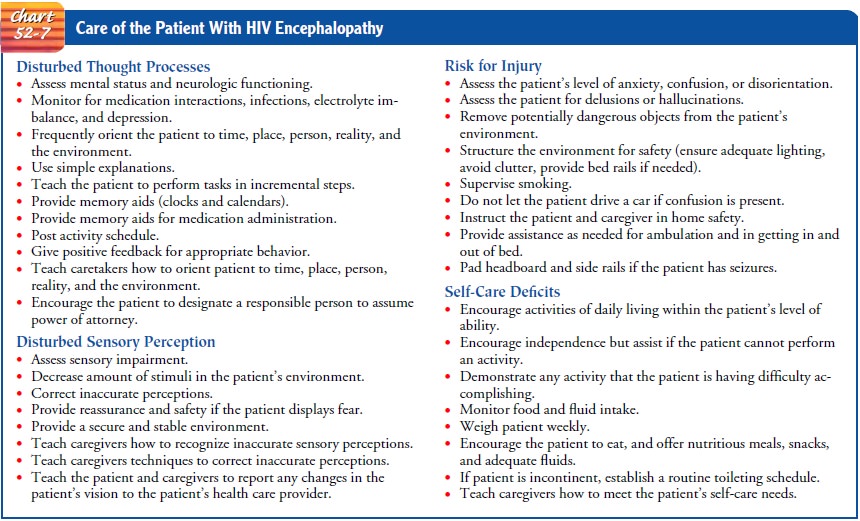
MAINTAINING THOUGHT PROCESSES
The
patient is assessed for alterations in mental status that may be related to
neurologic involvement, metabolic abnormalities, infection, side effects of
treatment, and coping mechanisms. Manifestations of neurologic impairment may
be difficult to dis-tinguish from psychological reactions to HIV infection,
such as anger and depression.
Family members are instructed to speak to the
patient in sim-ple, clear language and give the patient sufficient time to
respond to questions. Family members are instructed to orient the patient to
the daily routine by talking about what is taking place during daily activities.
They are encouraged to provide the patient with a regular daily schedule for
medication administration, grooming, meal times, bedtimes, and awakening times.
Posting the schedule in a prominent area (eg, on the refrigerator), providing
nightlights for the bedroom and bathroom, and planning safe leisure activi-ties
allow the patient to maintain a regular routine in a safe man-ner. Activities
that the patient previously enjoyed are encouraged. These should be easy to
accomplish and fairly short in duration. The nurse encourages the family to
remain calm and not to argue with the patient while protecting the patient from
injury. Around-the-clock supervision may be necessary, and strategies can be
im-plemented to prevent the patient from engaging in potentially dangerous
activities, such as driving, using the stove, or mowing the lawn. Strategies
for improving or maintaining functional abil-ities and for providing a safe
environment are used for patients with HIV encephalopathy (Chart 52-7).
IMPROVING AIRWAY CLEARANCE
Respiratory status, including rate, rhythm, use of accessory mus-cles, and breath sounds; mental status; and skin color must be assessed at least daily. Any cough and the quantity and charac-teristics of sputum are documented. Sputum specimens are ana-lyzed for infectious organisms. Pulmonary therapy (coughing, deep breathing, postural drainage, percussion, and vibration) is provided as often as every 2 hours to prevent stasis of secretions and to promote airway clearance. Because of weakness and fa-tigue, many patients require assistance in attaining a position (such as a high Fowler’s or semi-Fowler’s position) that facilitates breathing and airway clearance. Adequate rest is essential to max-imize energy expenditure and prevent excessive fatigue. The fluid volume status is evaluated so that adequate hydration can be maintained. Unless contraindicated by renal or cardiac disease, an intake of 3 L of fluid daily is encouraged. Humidified oxygen may be prescribed, and nasopharyngeal or tracheal suctioning, in-tubation, and mechanical ventilation may be necessary to main-tain adequate ventilation.
RELIEVING PAIN AND DISCOMFORT
The patient is assessed for the quality and
severity of pain associ-ated with impaired perianal skin integrity, the lesions
of KS, and peripheral neuropathy. In addition, the effects of pain on
elimi-nation, nutrition, sleep, affect, and communication are explored, along
with exacerbating and relieving factors. Cleaning the peri-anal area as previously
described can promote comfort. Topical anesthetics or ointments may be
prescribed. Use of soft cushions or foam pads may increase comfort while
sitting. The patient is instructed to avoid foods that act as bowel irritants.
Antispas-modics and antidiarrheal medications may be prescribed to re-duce the
discomfort and frequency of bowel movements. If necessary, systemic analgesic
agents may also be prescribed.
Pain from KS is frequently described as a
sharp, throbbing pres-sure and heaviness if lymphedema is present. Pain
management may include using nonsteroidal anti-inflammatory drugs (NSAIDs) and
opioids plus nonpharmacologic approaches such as relax-ation techniques. When
NSAIDs are used in patients receiving zidovudine, hepatic and hematologic
status must be monitored.
The
patient with pain related to peripheral neuropathy fre-quently describes it as
burning, numbness, and “pins and nee-dles.” Pain management measures may
include opioids, tricyclic antidepressants, and elastic compression stockings
to equalize pressure. Tricyclic antidepressants have been found helpful in
controlling the symptoms of neuropathic pain. They also poten-tiate the actions
of opioids and can be used to relieve pain with-out increasing the dose of the
opioid.
IMPROVING NUTRITIONAL STATUS
Nutritional status is assessed by monitoring
weight; dietary in-take; anthropometric measurements; and serum albumin, BUN,
protein, and transferrin levels. The patient is also assessed for factors that
interfere with oral intake, such as anorexia, oral and esophageal candidal
infection, nausea, pain, weakness, fatigue, and lactose intolerance. Based on
the results of assessment, the nurse can implement specific measures to
facilitate oral intake. The dietitian is consulted to determine the patient’s
nutritional requirements.
Control of nausea and vomiting with
antiemetic medications administered on a regular basis may increase the
patient’s dietary intake. Inadequate food intake resulting from pain caused by
mouth sores or a sore throat may be managed by administering prescribed opioids
and viscous lidocaine (the patient is instructed to rinse the mouth and
swallow). Additionally, the patient is en-couraged to eat foods that are easy
to swallow and to avoid rough, spicy, or sticky food items and foods that are
excessively hot or cold. Oral hygiene before and after meals is encouraged.
When
fatigue and weakness interfere with intake, the nurse encourages the patient to
rest before meals. If the patient is hos-pitalized, meals should be scheduled
so that they do not occur immediately after painful or unpleasant procedures.
The patient with diarrhea and abdominal cramping is encouraged to avoid foods
that stimulate intestinal motility and abdominal distention (eg, fiber-rich
food or lactose if the patient is intolerant to lactose). The patient is
instructed about ways to enhance the nutritional value of meals. Adding eggs,
butter, margarine, and fortified milk (powdered skim milk is added to milk to
increase the caloric content) to gravies, soups, or milkshakes can provide
additional calories and protein. Commercial supplements such as puddings,
powders, milkshakes, and Advera (a nutritional product specifi-cally designed
for people with HIV infection or AIDS) may also be useful. Patients who cannot
maintain their nutritional status through oral intake may require enteral
feedings or parenteral nutrition.
DECREASING THE SENSE OF ISOLATION
Individuals with AIDS are at risk for double
stigmatization. They have what society refers to as a “dread disease,” and they
may have a lifestyle that differs from what is considered acceptable by many
people. Many people with AIDS are young adults at a develop-mental stage
usually associated with establishing intimate rela-tionships and personal and
career goals and having and raising children. Their focus changes as they are
faced with a disease that threatens their life expectancy with no cure. In
addition, they may be forced to reveal hidden lifestyles or behaviors to
family, friends, coworkers, and health care providers. As a result, people with
HIV infection may be overwhelmed with emotions such as anxiety, guilt, shame,
and fear. They also may be faced with mul-tiple losses, such as rejection by
family and friends and loss of sex-ual partners, family, and friends; financial
security; normal roles and functions; self-esteem; privacy; ability to control
bodily func-tions; ability to interact meaningfully with the environment; and
sexual functioning. Some patients may harbor feelings of guilt be-cause of
their lifestyle or because they may have infected others in current or previous
relationships. Other patients may feel anger toward sexual partners who
transmitted the virus. Infection con-trol measures used in the hospital or at
home may further con-tribute to the patient’s emotional isolation. Any or all
of these stressors may cause the patient with AIDS to withdraw both physically
and emotionally from social contact.
Nurses
are in a key position to provide an atmosphere of acceptance and understanding
of people with AIDS and their families and partners. The patient’s usual level
of social inter-action is assessed as early as possible to provide a baseline
for monitoring changes in behavior indicative of social isolation (eg,
decreased interaction with staff or family, hostility, non-compliance).
Patients are encouraged to express feelings of isola-tion and loneliness, with
the assurance that these feelings are not unique or abnormal.
Providing
information about how to protect themselves and others may help patients avoid
social isolation. Patients, family, and friends must be assured that AIDS is
not spread through ca-sual contact. Educating ancillary personnel, nurses, and
physi-cians will help to reduce factors that might contribute to patients’
feelings of isolation. Patient care conferences that address the psy-chosocial
issues associated with AIDS may help sensitize the health care team to
patients’ needs.
COPING WITH GRIEF
The
nurse can help patients verbalize feelings and explore and identify resources
for support and mechanisms for coping, espe-cially when the patient is grieving
about anticipated losses. Pa-tients are encouraged to maintain contact with
family, friends, and coworkers and to use local or national AIDS support groups
and hotlines. If possible, losses are identified and addressed. The patient is
encouraged to continue usual activities whenever pos-sible. Consultations with
mental health counselors are useful for many patients.
MONITORING AND MANAGING POTENTIAL COMPLICATIONS
Opportunistic Infections
Patients
who are immunosuppressed are at risk for OIs. There-fore, anti-infective agents
may be prescribed and laboratory tests obtained to monitor their effect. Signs
and symptoms of OIs, in-cluding fever, malaise, difficulty breathing, nausea or
vomiting, diarrhea, difficulty swallowing, and any occurrences of swelling or
discharge, should be reported.
Respiratory Failure
Impaired breathing is a major complication
that increases the pa-tient’s discomfort and anxiety and may lead to
respiratory and cardiac failure. The respiratory rate and pattern are monitored
and the lungs are auscultated for abnormal breath sounds. The patient is
instructed to report shortness of breath and increasing difficulty in carrying
out usual activities. Pulse rate and rhythm, blood pressure, and oxygen
saturation are monitored. Suctioning and oxygen therapy may be prescribed to
ensure an adequate air-way and to prevent hypoxia. Mechanical ventilation may
be nec-essary for a patient who cannot maintain adequate ventilation as a
result of pulmonary infection, fluid and electrolyte imbalance, or respiratory
muscle weakness. Arterial blood gas values are used to guide ventilator
settings. If the patient is intubated, a method must be established to allow
communication with the nurse and others. Attention must be given to assisting
the patient on me-chanical ventilation to cope with the stress associated with
intu-bation and ventilator assistance. The possible need for mechanical
ventilation in the future should be discussed early in the course of the
disease, when the patient is able to make his or her desires about treatment
known. The use of mechanical ventilation should be consistent with the
patient’s decisions about end-of-life treatment.
Cachexia and Wasting
Wasting
syndrome and fluid and electrolyte disturbances, in-cluding dehydration, are
common complications of HIV infec-tion and AIDS. The patient’s nutritional and
electrolyte status is evaluated by monitoring weight gains or losses, skin
turgor, fer-ritin levels, hemoglobin and hematocrit values, and electrolyte
levels. Fluid and electrolyte status is monitored on an ongoing basis; fluid
intake and output and urine specific gravity may be monitored daily if the
patient is hospitalized with complications. The skin is assessed for dryness
and adequate turgor. Vital signs are monitored for decreased systolic blood
pressure or increased pulse rate upon sitting or standing. Signs and symptoms
of elec-trolyte disturbances, such as muscle cramping, weakness, irregu-lar
pulse, decreased mental status, nausea, and vomiting, are documented and
reported to the physician. Serum electrolyte val-ues are monitored and
abnormalities reported.
The nurse helps the patient select foods that
will replenish electrolytes, such as oranges and bananas (potassium) and cheese
and soups (sodium). A fluid intake of 3 L or more, unless con-traindicated, is
encouraged to replace fluid lost with diarrhea, and measures to control
diarrhea are initiated. If fluid and electrolyte imbalances persist, the nurse
may administer IV fluids and elec-trolytes as prescribed. Effects of parenteral
therapy are monitored.
Side Effects of Medications
Adverse reactions are of concern in patients
who receive many medications to treat HIV infection or its complications. Many
medications can cause severe toxic effects. Information about the purpose of
the medications, correct administration, side effects, and strategies to manage
or prevent side effects is provided. Pa-tients and their caregivers need to
know which signs and symp-toms of side effects should be reported immediately
to their primary health care provider (see Table 52-3).
In addition to medications used to treat HIV
infection, other medications that may be required include opioids, tricyclics,
and NSAIDs for pain relief; medications for treatment of OIs; anti-histamines
(diphenhydramine) for relief of pruritus (itching); acetaminophen or aspirin
for management of fever; and antiemetic agents for control of nausea and
vomiting. Concurrent use of many of these medications may cause many drug
interactions, in-cluding hepatic and hematologic abnormalities. Therefore,
care-ful laboratory monitoring for these abnormalities is warranted.
During each contact with the patient, it is
important for the nurse to ask not only about side effects but also how well
the pa-tient is managing the medication regimen. The nurse may be able to
assist the patient in organizing and planning the medication schedule to
promote adherence to the medication regimen.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
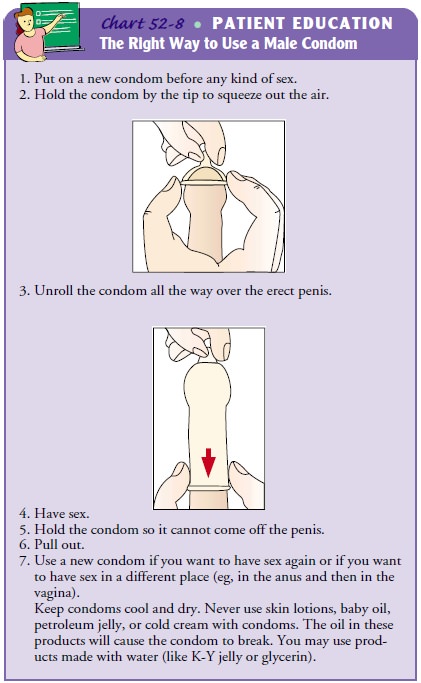
Patients,
families, and friends are instructed about the routes of transmission of HIV.
The nurse discusses precautions to prevent transmitting HIV, including using
condoms during vaginal or anal intercourse (Chart 52-8); using dental dams or
avoiding oral contact with the penis, vagina, or rectum; avoiding sexual
prac-tices that might cut or tear the lining of the rectum, vagina, or penis;
and avoiding sexual contact with multiple partners, indi-viduals known to be
HIV infected, people who use injection drugs, and sexual partners of people who
inject drugs.
Patients and their families or caregivers must receive instruc-tions about how to prevent disease transmission, including hand-washing techniques, and in methods for safely handling items soiled with body fluids. Caregivers in the home are taught how to administer medications, including IV preparations.
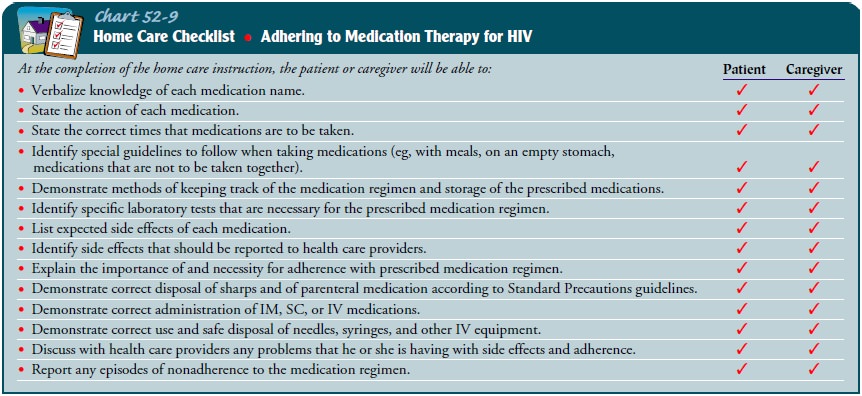
The medication regimens used for patients
with HIV infec-tion and AIDS are often complex and expensive. Patients
receiv-ing combination therapies for treatment of HIV infection and its
complications require careful teaching about the importance of taking
medications as prescribed and explanations and assistance in fitting the
medication regimen into their lives (Chart 52-9).
Guidelines about infection and infection
control, follow-up care, diet, rest, and activity are also necessary. Patient
teaching also includes strategies to avoid infection. The importance of
per-sonal hygiene is emphasized. Kitchen and bathroom surfaces should be
cleaned regularly with disinfectants to prevent fungal and bacterial growth.
Patients with pets are instructed to have an-other person clean areas soiled by
animals, such as bird cages and litter boxes. If this is not possible, the
patient should use gloves to clean up after pets. Patients are advised to avoid
exposure to others who are sick or who have been recently vaccinated. Patients
with AIDS and their sexual partners are strongly urged to avoid expo-sure to body
fluids during sexual activities and to use condoms for any form of sexual
intercourse. Injection drug use is strongly discouraged because of the risk to
the patient of other infections and transmission of HIV infection to others.
Patients infected with HIV are urged to avoid exposure to bodily fluids
(through sexual contact or injection drug use) to prevent exposure to other HIV
strains. The importance of avoiding smoking and main-taining a balance between
diet, rest, and exercise is also emphasized.
If the
patient requires enteral or parenteral nutrition, instruc-tion is provided to
patients and families about how to administer nutritional therapies at home.
Home care nurses provide ongoing teaching and support for the patient and
family.
Patients
who are HIV positive or who inject drugs are in-structed not to donate blood.
Injection drug users who are un-willing to stop using drugs are advised to
avoid sharing drug equipment with others.
Continuing Care
Many
people with AIDS remain in their community and con-tinue their usual daily
activities, whereas others can no longer work or maintain their independence.
Families or caregivers may need assistance in providing supportive care. There
are many community-based organizations that provide a variety of services for
people living with HIV infection and AIDS; nurses can help identify these
services.
Community
health nurses, home care nurses, and hospice nurses are in an excellent
position to provide the support and guidance so often needed in the home setting.
As hospital costs continue to rise and insurance coverage continues to decline,
the complexity of home care increases. Home care nurses are key in the
administration of parenteral antibiotics, chemotherapy, and nutrition in the
home.
During
home visits, the nurse assesses the patient’s physical and emotional status and
home environment. The patient’s ad-herence to the therapeutic regimen is
assessed, and strategies are suggested to assist with adherence. The patient is
assessed for pro-gression of disease and for adverse side effects of
medications. Pre-vious teaching is reinforced, and the importance of keeping
follow-up appointments is stressed.
Complex wound care or respiratory care may be required in the home. Patients and families are often unable to meet these skilled care needs without assistance. Nurses may refer patients to community programs that offer a range of services for patients, friends, and families, including help with housekeeping, hygiene, and meals; transportation and shopping; individual and group therapy; support for caregivers; telephone networks for the home-bound; and legal and financial assistance. These services are typically provided by both professional and nonprofessional vol-unteers. A social worker may be consulted to identify sources of financial support, if needed.
Home
care and hospice nurses are increasingly called on to provide physical and
emotional support to patients and families as patients with AIDS enter the
terminal stages of disease. This support takes on special meaning when people
with AIDS lose friends and when family members fear the disease or feel anger
concerning the patient’s lifestyle. The nurse encourages the pa-tient and
family to discuss end-of-life decisions and to ensure that care is consistent
with those decisions, all comfort measures are employed, and the patient is
treated with dignity at all times.
Evaluation
EXPECTED PATIENT OUTCOMES
Expected
patient outcomes may include:
1) Maintains skin integrity
2) Resumes usual bowel
habits
3) Experiences no
infections
4) Maintains adequate level
of activity tolerance
5) Maintains usual level of
thought processes
6) Maintains effective
airway clearance
7) Experiences increased
sense of comfort, less pain
8) Maintains adequate
nutritional status
9) Experiences decreased
sense of social isolation
10) Progresses through
grieving process
11) Reports increased
understanding of AIDS and partici-pates in self-care activities as possible
12) Remains free of
complications
Related Topics