Chapter: Medical Surgical Nursing: Management of Patients With Oncologic or Degenerative Neurologic Disorders
Spinal Cord Tumors
SPINAL CORD TUMORS
Tumors within the spine
are classified according to their anatomic relation to the spinal cord. They
include intramedullary lesions (within the spinal cord),
extramedullary-intradural lesions (within or under the spinal dura), and
extramedullary-extradural lesions (outside the dural membrane). Tumors
occurring within the spinal cord or exerting pressure on it cause symptoms
ranging from localized or shooting pains and weakness and loss of reflexes
above the tumor level to progressive loss of motor function and paralysis.
Usually, sharp pain occurs in the area innervated by the spinal roots that
arise from the cord in the region of the tumor. In addition, increasing sensory
deficits develop below the level of the lesion.
Assessment and Diagnostic Findings
Neurologic examination
and diagnostic studies are used to make the diagnosis. Neurologic examination
includes assessment of pain, loss of reflexes, loss of sensation or motor
function, and the presence of weakness and paralysis. Helpful diagnostic
studies in-clude x-rays, radionuclide bone scans, and MRI. MRI is the most
sensitive diagnostic tool and is particularly helpful in detecting epidural
spinal cord compression and vertebral bone metastases ( Jacobs& Perrin,
2001; Nevidjon & Sowers, 2000).
Medical Management
Treatment of specific
intraspinal tumors depends on the type and location of the tumor and the
presenting symptoms and physical status of the patient. Surgical intervention
is the primary treat-ment for most spinal cord tumors. Other treatment
modalities include partial removal of the tumor, decompression of the spinal
cord, chemotherapy, and radiation therapy, particularly for in-tramedullary
tumors and metastatic lesions ( Jacobs& Perrin, 2001).
Epidural spinal cord
compression occurs in approximately 5% of patients who die of cancer and is
considered a neurologic emer-gency (Nevidjon & Sowers, 2000). In the
patient with epidural spinal cord compression resulting from metastatic cancer
(most commonly from breast, prostate, or lung), high-dose dexametha-sone combined
with radiation therapy is effective in relieving pain (Nevidjon & Sowers,
2000).
SURGICAL MANAGEMENT
Tumor removal is desirable but not always possible. The
goal is to remove as much tumor as possible while sparing uninvolved portions
of the spinal cord. Microsurgical techniques have im-proved the prognosis for
patients with intramedullary tumors. Prognosis is related to the degree of
neurologic impairment at the time of surgery, the speed with which symptoms
occurred, and the tumor origin. Patients with extensive neurologic deficits
be-fore surgery usually do not make significant functional recovery even after
successful tumor removal.
Nursing Management
PROVIDING PREOPERATIVE CARE
The objectives of
preoperative care include recognition of neuro-logic changes through ongoing
assessments, pain control, and management of altered activities of daily living
due to sensory and motor deficits and bowel and bladder dysfunction. The nurse
as-sesses for weakness, muscle wasting, spasticity, sensory changes, bowel and
bladder dysfunction, and potential respiratory prob-lems, especially if a
cervical tumor is present. The patient is also evaluated for coagulation
deficiencies. A history of aspirin intake is obtained and reported because the
use of aspirin may impede hemostasis postoperatively. Breathing exercises are
taught and demonstrated preoperatively. Postoperative pain management
strategies are discussed with the patient before surgery.
ASSESSING THE PATIENT AFTER SURGERY
The patient is monitored
for deterioration in neurologic status. A sudden onset of neurologic deficit is
an ominous sign and maybe due to vertebral collapse associated with spinal cord
infarction. Frequent neurologic checks are carried out, with emphasis on
movement, strength, and sensation of the upper and lower ex-tremities.
Assessment of sensory function involves pinching the skin of the arms, legs,
and trunk to determine if there is loss of feeling and, if so, determining at
what level. Vital signs are mon-itored at regular intervals.
MANAGING PAIN
The prescribed pain
medication should be administered in ade-quate amounts and at appropriate
intervals to relieve pain and prevent its recurrence. Pain is the hallmark of
spinal metastasis. Patients with sensory root involvement or vertebral collapse
may suffer excruciating pain, which requires effective pain management.
The bed is usually kept
flat initially. The nurse turns the pa-tient as a unit, keeping shoulders and
hips aligned and the back straight. The side-lying position is usually the most
comfortable because this position imposes the least pressure on the surgical
site. Placement of a pillow between the knees of the patient in a side-lying
position helps to prevent extreme knee flexion.
MONITORING AND MANAGINGPOTENTIAL COMPLICATIONS
If the tumor was in the
cervical area, the possibility of postoper-ative respiratory compromise arises.
The nurse monitors the pa-tient for asymmetric chest movement, abdominal
breathing, and abnormal breath sounds. For a high cervical lesion, the endotra-cheal
tube remains in place until adequate respiratory function is ensured. The
patient is encouraged to perform deep-breathing and coughing exercises.
The area over the
bladder is palpated or a bladder scan is per-formed to assess for urinary retention.
The nurse also monitors for incontinence because urinary dysfunction usually
implies sig-nificant decompensation of spinal cord function. An intake and
output record is maintained. Additionally, the abdomen is aus-cultated for
bowel sounds.
Staining of the dressing
may indicate leakage of CSF from the surgical site, which may lead to serious
infection or to an inflam-matory reaction in the surrounding tissues that can
cause severe pain in the postoperative period.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care.
In preparation for
discharge, pa-tients are assessed for their ability to function independently
in the home and for the availability of resources such as family members to
assist in caregiving. Patients with residual sensory involvement are cautioned
about the dangers of extremes in temperature. They should be alert to the
dangers of heating devices (eg, hot water bottles, heating pads, and space
heaters). The patient is taught to check skin integrity daily. Patients with impaired
motor function related to motor weakness or paralysis may require training in
activities of daily living and safe use of assistive devices, such as a cane,
walker, or wheelchair.
The patient and family
member are instructed about pain management strategies, bowel and bladder
management, and assessment for signs and symptoms that should be reported
promptly.
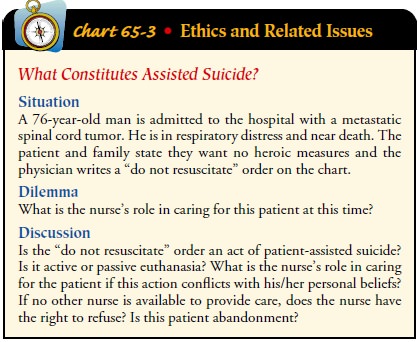
Continuing Care.
Referral for inpatient
or outpatient rehabilita-tion may be warranted to improve self-care abilities.
A home care referral may be indicated and provides the home care nurse with the
opportunity to assess the patient’s physical and psychological status and the
patient’s and family’s ability to adhere to recom-mended management strategies.
During the home visit, the nurse determines whether changes in neurologic
function have oc-curred. The patient’s respiratory and nutritional status is
assessed. The adequacy of pain management is assessed, and modifications are
made to ensure adequate pain relief. The need for hospice ser-vices or
placement in an extended-care facility is discussed with the patient and family
if warranted, and the patient is asked about preferences for end-of-life care
(Chart 65-3). Additionally, social workers may be consulted to assist the
patient and family mem-bers in identifying support groups and agencies that can
provide help in coping with the disease process.
Related Topics