Chapter: Medical Surgical Nursing: Management of Patients With Oncologic or Degenerative Neurologic Disorders
Primary Brain Tumors
Oncologic
Disorders of the Brain and Spinal Cord
Oncologic disorders in
the brain and spinal cord include several types of neoplasms, each with its own
biology, prognosis, and treatment options. Because of the unique anatomy and
physiol-ogy of the central nervous system (CNS), this collection of neo-plasms
is challenging to diagnose and treat. The pathophysiology, clinical manifestations,
assessment findings, and medical and nursing management of brain tumors and
spinal cord tumors are discussed in the following sections.
PRIMARY BRAIN TUMORS
A brain tumor is a
localized intracranial lesion that occupies space within the skull. Tumors
usually grow as a spherical mass, but they can grow diffusely and infiltrate
tissue. The effects of neo-plasms occur from the compression and infiltration
of tissue. A variety of physiologic changes result, causing any or all of the
fol-lowing pathophysiologic events:
·
Increased intracranial
pressure (ICP) and cerebral edema
·
Seizure activity and focal
neurologic signs
·
Hydrocephalus
·
Altered pituitary function
Primary brain tumors originate from cells and structures
within the brain. Secondary, or metastatic, brain tumors develop from
structures outside the brain and occur in 20% to 40% of all patients with
cancer. Brain tumors rarely metastasize outside the CNS, but metastatic lesions
to the brain occur commonly from the lung, breast, lower gastrointestinal
tract, pancreas, kidney, and skin (melanomas).
The cause of primary
brain tumors is unknown. The only known risk factor is exposure to ionizing
radiation. Both glial and meningeal neoplasms have been linked to irradiation
of the cranium, with a latency period of 10 to 20 years after
exposure(DeAngelis, 2001). Additional possible causes have been investi-gated,
but results of studies are conflicting and unconvincing; suggested causes have
included use of cellular telephones, expo-sure to high-tension wires, use of
hair dyes, head trauma, dietary exposure to such factors as nitrates (found in
some processed and barbecued foods), and other sources (DeAngelis, 2001).
The incidence of brain tumors appears to have increased
in the past few decades. Epidemiologic data, however, suggest that this is due
more to aggressive and accurate diagnosis rather than to an actual rise in
incidence. It is estimated that there are about 17,000 new cases of primary
brain tumors per year, 9,600 in men and 7,400 in women (American Cancer
Society, 2002). Secondary tumors or metastases to the brain from a systemic
primary cancer are more common (DeAngelis, 2001). The highest incidence of
brain tumors in adults occurs in the fifth, sixth, and seventh decades, with a
slightly higher incidence in men. In adults, most brain tumors originate from
glial cells (glial cells make up the structure and support system of the brain
and spinal cord) and are supratentorial (located above the covering of the
cerebellum). Neoplastic lesions in the brain ultimately cause death by
impair-ing vital functions, such as respiration, or by increasing intracra-nial
pressure (ICP).
Pathophysiology
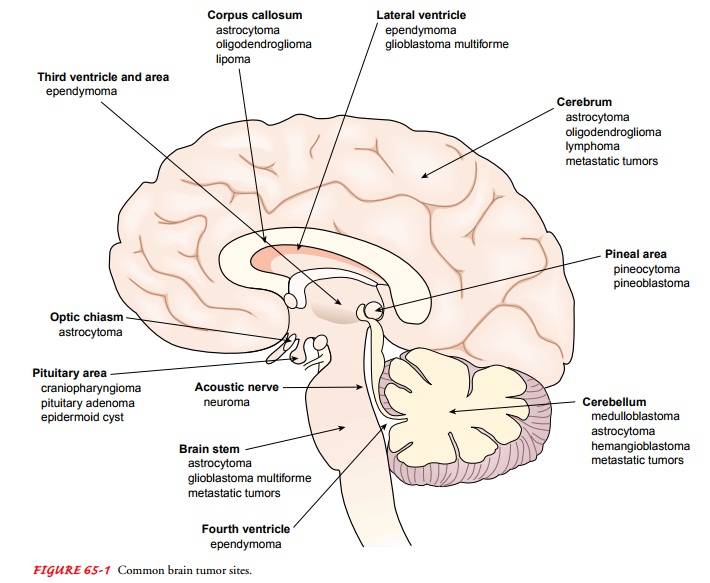
Brain tumors may be classified into several groups: those
arising from the coverings of the brain (eg, dural meningioma), those
de-veloping in or on the cranial nerves (eg, acoustic neuroma), those
originating within brain tissue (eg, gliomas), and metastatic le-sions
originating elsewhere in the body. Tumors of the pituitary and pineal glands
and of cerebral blood vessels are also types of brain tumors. Relevant clinical
considerations include the loca-tion and the histologic character of the tumor.
Tumors may be benign or malignant. A benign tumor can occur in a vital area and
can grow large enough to have effects as serious as those of a malignant tumor.
GLIOMAS
Glial tumors, the most common type of brain neoplasm, are
di-vided into many categories (DeAngelis, 2001). See Chart 65-1 for the
classification of brain tumors. Astrocytomas are the most common type of glioma
and are graded from I to IV, indicating the degree of malignancy. The grade is
based on cellular density, cell mitosis, and appearance. Usually, these tumors
spread by in-filtrating into the surrounding neural connective tissue and
there-fore cannot be totally removed without causing considerable damage to
vital structures.
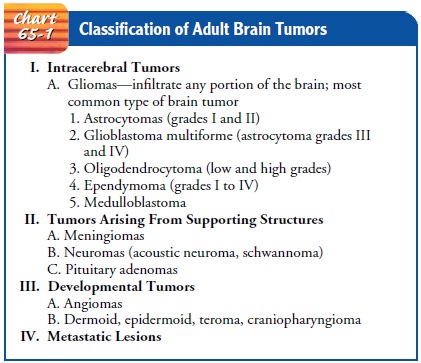
Oligodendroglial tumors are another type of glial tumor,
rep-resenting 20% of gliomas (DeAngelis, 2001). The histologic distinction
between astrocytomas and oligodendrogliomas is difficult to make but important,
as recent research shows that oligodendrogliomas are more sensitive to
chemotherapy than astrocytomas. These tumors are categorized as low-grade and
high-grade (anaplastic).
MENINGIOMAS
Meningiomas, which
represent 20% of all primary brain tumors, are common benign encapsulated
tumors of arachnoid cells on the meninges (DeAngelis, 2001). They are
slow-growing and occur most often in middle-aged adults (more often in women).
Meningiomas most often occur in areas proximal to the venous sinuses.
Manifestations depend on the area involved and are the result of compression
rather than invasion of brain tissue. Standard treatment is surgery with
complete removal or partial dissection.
ACOUSTIC NEUROMAS
An acoustic neuroma is a
tumor of the eighth cranial nerve, the cranial nerve most responsible for
hearing and balance. It usually arises just within the internal auditory
meatus, where it frequently expands before filling the cerebellopontine recess.
An acoustic neuroma may grow slowly and attain
considerable size before it is correctly diagnosed. The patient usually
experi-ences loss of hearing, tinnitus, and episodes of vertigo and stag-gering
gait. As the tumor becomes larger, painful sensations of the face may occur on
the same side as a result of the tumor’s com-pression of the fifth cranial
nerve.
With improved imaging
techniques and the use of the oper-ating microscope and microsurgical
instrumentation, even large tumors can be removed through a relatively small
craniotomy. Some of these tumors may be suitable for stereotactic radiother-apy
rather than surgery.
PITUITARY ADENOMAS
Pituitary tumors
represent about 8% to 12% of all brain tumors and cause symptoms as a result of
pressure on adjacent structures or hormonal changes (hyperfunction or
hypofunction of the pi-tuitary). The pituitary gland, also called the
hypophysis, is a rel-atively small gland located in the sella turcica. It is
attached to thehypothalamus by a short stalk (hypophyseal stalk) and is divided
into two lobes: the anterior (adenohypophysis) and the posterior
(neurohypophysis).
Pressure Effects of Pituitary Adenomas.
Pressure from a
pitu-itary adenoma may be exerted on the optic nerves, optic chiasm, or optic
tracts or on the hypothalamus or the third ventricle when the tumor invades the
cavernous sinuses or expands into the sphe-noid bone. These pressure effects
produce headache, visual dys-function, hypothalamic disorders (eg, disorders of
sleep, appetite, temperature and emotions), increased ICP, and enlargement and
erosion of the sella turcica.
Hormonal Effects of Pituitary Adenomas.
Functioning
pituitarytumors can produce one or more hormones normally produced by the
anterior pituitary. These hormones may cause prolactin-secreting pituitary
adenomas (prolactinomas), growth hormone-secreting pituitary adenomas that
produce acromegaly in adults, and adrenocorticotropic hormone (ACTH)-producing
pituitary adenomas that result in Cushing’s disease. Adenomas that secrete
thyroid-stimulating hormone or follicle-stimulating hormone and luteinizing
hormone occur infrequently, whereas adenomas that produce both growth hormone
and prolactin are relatively common.
The female patient whose
pituitary gland is secreting excessive quantities of prolactin presents with
amenorrhea or galactorrhea (excessive or spontaneous flow of milk). Male
patients with pro-lactinomas may present with impotence and hypogonadism.
Acromegaly, caused by excess growth hormone, produces en-largement of the hands
and feet, distortion of the facial features, and pressure on peripheral nerves
(entrapment syndromes). The clinical features of Cushing’s disease, a condition
associated with prolonged overproduction of cortisol, occur with excessive
pro-duction of ACTH. Manifestations include a form of obesity with
redistribution of fat to the facial, supraclavicular, and abdominal areas;
hypertension; purple striae and ecchymoses; osteoporosis; elevated blood
glucose levels; and emotional disorders.
ANGIOMAS
Brain angiomas (masses
composed largely of abnormal blood ves-sels) are found either in or on the
surface of the brain. They occur in the cerebellum in 83% of cases. Some
persist throughout life without causing symptoms; others cause symptoms of a
brain tumor. Occasionally, the diagnosis is suggested by the presence of
another angioma somewhere in the head or by a bruit (an ab-normal sound)
audible over the skull. Because the walls of the blood vessels in angiomas are
thin, these patients are at risk for a cerebral vascular accident (stroke). In
fact, cerebral hemorrhage in people younger than 40 years of age should suggest
the possi-bility of an angioma.
Clinical Manifestations
Brain tumors can produce
either focal or generalized neurologic signs and symptoms. Generalized symptoms
reflect increased ICP, and the most common focal or specific signs and symptoms
result from tumors interfering with functions in specific brain re-gions.
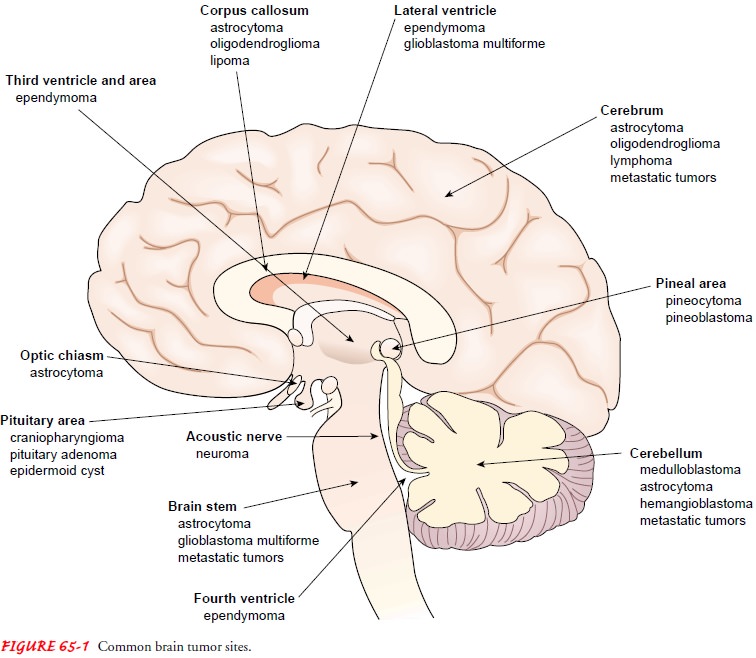
Figure 65-1 indicates common tumor sites in the brain.
INCREASING ICP
As discussed, the skull is a rigid compartment con-taining essential noncompressible contents: brain matter, intra-vascular blood, and cerebrospinal fluid (CSF). According to the modified Monro-Kellie hypothesis, if any one of these skull components increases in volume, ICP increases unless one of the other components decreases in volume.
Consequently, any change in volume
occupied by the brain (as occurs with disorders such as brain tumor or cerebral
edema) produces signs and symptoms of increased ICP.
Symptoms of increased
ICP result from a gradual compression of the brain by the enlarging tumor. The
effect is a disruption of the equilibrium that exists between the brain, the
CSF, and the cerebral blood, all located within the skull. As the tumor grows,
compensatory adjustments may occur through compression of intracranial veins,
reduction of CSF volume (by increased ab-sorption or decreased production), a
modest decrease of cerebral blood flow, and reduction of intracellular and
extracellular brain tissue mass. When these compensatory mechanisms fail, the
pa-tient develops signs and symptoms of increased ICP. The three most common
signs of increased ICP are headache, nausea and vomiting, and a sixth-nerve
palsy (DeAngelis, 2001). Personality changes and a variety of focal deficits,
including motor, sensory, and cranial nerve dysfunction, are also common.
Headache.
Headache, although not always present, is most
com-mon in the early morning and is made worse by coughing, strain-ing, or
sudden movement. It is thought to be caused by the tumor invading, compressing,
or distorting the pain-sensitive structures or by edema that accompanies the
tumor. Headaches are usuallydescribed as deep or expanding
or as dull but unrelenting. Frontal tumors usually produce a bilateral frontal
headache; pituitary gland tumors produce pain radiating between the two temples
(bitemporal); in cerebellar tumors, the headache may be located in the
suboccipital region at the back of the head.
Vomiting.
Vomiting, seldom related to food intake, is
usuallydue to irritation of the vagal centers in the medulla. If the vom-iting
is of the forceful type, it is described as projectile vomiting.
Visual Disturbances.
Papilledema(edema
of the optic nerve) ispresent in 70% to 75% of patients and is associated with
visual disturbances such as decreased visual acuity, diplopia (double vision),
and visual field deficits.
LOCALIZED SYMPTOMS
The most common focal or
localized symptoms are hemiparesis, seizures, and mental status changes
(DeAngelis, 2001). When specific regions of the brain are affected, additional
local signs and symptoms occur, such as sensory and motor abnormalities, visual
alterations, alterations in cognition, and language disturbances such as
aphasia. The progression of the signs and symptoms is important because it
indicates tumor growth and expansion. For example, a rapidly developing
hemiparesis is more typical of a highly malignant glioma than a low-grade tumor
(DeAngelis, 2001).
Although some tumors are
not easily localized because they lie in so-called silent areas of the brain
(ie, areas in which functions are not definitely determined), many tumors can
be localized by correlating the signs and symptoms to known areas of the brain,
as follows:
·
A motor cortex tumor produces
seizure-like movements lo-calized on one side of the body, called Jacksonian
seizures.
·
An occipital lobe tumor
produces visual manifestations: contralateral homonymous hemianopsia (visual
loss in half of the visual field on the opposite side of the tumor) and visual
hallucinations.
·
A cerebellar tumor causes
dizziness, an ataxic or staggering gait with a tendency to fall toward the side
of the lesion, marked muscle incoordination, and nystagmus (involun-tary
rhythmic eye movements), usually in the horizontal direction.
·
A frontal lobe tumor
frequently produces personality dis-orders, changes in emotional state and
behavior, and an un-interested mental attitude. The patient often becomes
extremely untidy and careless and may use obscene language.
·
A
cerebellopontine angle tumor usually originates in the sheath of the acoustic
nerve and gives rise to a characteris-tic sequence of symptoms. Tinnitus and
vertigo appear first, soon followed by progressive nerve deafness (eighth
cranial nerve dysfunction). Numbness and tingling of the face and the tongue
occur (due to involvement of the fifth cranial nerve). Later, weakness or
paralysis of the face develops (seventh cranial nerve involvement). Finally,
because the enlarging tumor presses on the cerebellum, abnormalities in motor
function may be present.
Assessment and Diagnostic Findings
The history of the
illness and the manner and time frame in which the symptoms evolved are key
components in the diagno-sis of brain tumors. A neurologic examination indicates
the areas of the CNS involved. To assist in the precise localization of the
lesion, a battery of tests is performed. Computed tomography (CT) scans,
enhanced by a contrast agent, can give specific infor-mation concerning the
number, size, and density of the lesions and the extent of secondary cerebral
edema. CT scans can pro-vide information about the ventricular system. Magnetic
reso-nance imaging (MRI) is the most helpful diagnostic tool for detecting
brain tumors, particularly smaller lesions, and tumors in the brain stem and
pituitary regions, where bone interferes with CT (Fig. 65-2). In a few
instances, the appearance of a brain tumor on an MRI is so characteristic that
a biopsy is unnecessary, especially when the tumor is located in a part of the brain
that is difficult to biopsy (American Cancer Society, 2001).
In centers where
positron emission tomography (PET) is avail-able, it is used to supplement MRI.
On PET scans, low-grade tu-mors are associated with hypometabolism and
high-grade tumors show hypermetabolism. This information can be useful in
treat-ment decisions (DeAngelis, 2001). Computer-assisted stereotactic
(three-dimensional) biopsy is being used to diagnose deep-seated brain tumors
and to provide a basis for treatment and prognosis. Cerebral angiography
provides visualization of cerebral blood vessels and can localize most cerebral
tumors.
An electroencephalogram
(EEG) can detect an abnormal brain wave in regions occupied by a tumor and is
used to evalu-ate temporal lobe seizures and assist in ruling out other
disorders.
Cytologic studies of the CSF may be performed to detect ma-lignant cells because CNS tumors can shed cells into the CSF.
Gerontologic Considerations
Intracranial tumors can
produce personality changes, confusion, speech dysfunction, or disturbances of
gait. In elderly patients early signs and symptoms of intracranial tumors can
be easily overlooked and incorrectly attributed to cognitive and neurologic
changes associated with normal aging. The most frequent tumor types in the
elderly are anaplastic astrocytoma, glioblastoma multi-forme, and cerebral
metastases from other sites. The incidence of primary brain tumors and the
likelihood of malignancy increase with age. Signs and symptoms in the elderly
must be carefully evaluated because 10% of brain metastases occur in patients
with a history of prior cancer (Rude, 2000).
Medical Management
A variety of medical
treatment modalities, including chemother-apy and external-beam radiation
therapy, are used alone or in combination with surgical resection. Radiation
therapy, the corner-stone of treatment of many brain tumors, decreases the
incidence of recurrence of incompletely resected tumors. Brachytherapy (the
surgical implantation of radiation sources to deliver high doses at a short
distance) has had promising results for primary malignancies. It is generally
used as an adjunct to conventional radiation therapy or as a rescue measure for
recurrent disease.
Intravenous (IV)
autologous bone marrow transplantation is used in some patients who will
receive chemotherapy or radiation therapy because it has the potential to
“rescue” the patient from the bone marrow toxicity associated with high doses
of chemother-apy and radiation. A fraction of the patient’s bone marrow is
as-pirated, usually from the iliac crest, and stored. The patient receives
large doses of chemotherapy or radiation therapy to destroy large numbers of
malignant cells. The marrow is then reinfused intra-venously after treatment is
completed.
Corticosteroids may be used before and after treatment to
reduce cerebral edema and promote a smoother, more rapid re-covery.
Gene-transfer therapy uses retroviral vectors to carry genes to the tumor,
reprogramming the tumor tissue for susceptibil-ity to treatment. This approach
is being tested.
A new technique being investigated is photodynamic
therapy. This is a treatment of primary malignant brain tumors that de-livers a
targeted therapy while conserving healthy brain tissue (Goodell & Muller, 2001).
SURGICAL MANAGEMENT
The objective of
surgical management is to remove or destroy the entire tumor without increasing
the neurologic deficit (paralysis, blindness) or to relieve symptoms by partial
removal (decom-pression). A variety of treatment modalities may be used; the
spe-cific approach depends on the type of tumor, its location, and
accessibility. In many patients, combinations of these modalities may be used.
Most pituitary adenomas are treated by transsphe-noidal microsurgical removal,
whereas the re-mainder of tumors that cannot be removed completely are treated
by radiation. An untreated brain tumor ultimately leads to death, either from
increasing ICP or from the damage to brain tissue it causes.
Conventional surgical approaches require an incision into the skull (craniotomy). This approach is used in patients with meningiomas, acoustic neuromas, cystic astrocytomas of the cerebellum, colloid cysts of the third ventricle, congenital tumors such as dermoid cyst, and some of the granulomas. For patients with malignant glioma, complete removal of the tumor and cure are not possible, but the rationale for resection includes relieving ICP, removing any necrotic tissue, and reducing the bulk of the tumor, which theoretically leaves behind fewer cells to become resistant to radiation or chemotherapy.
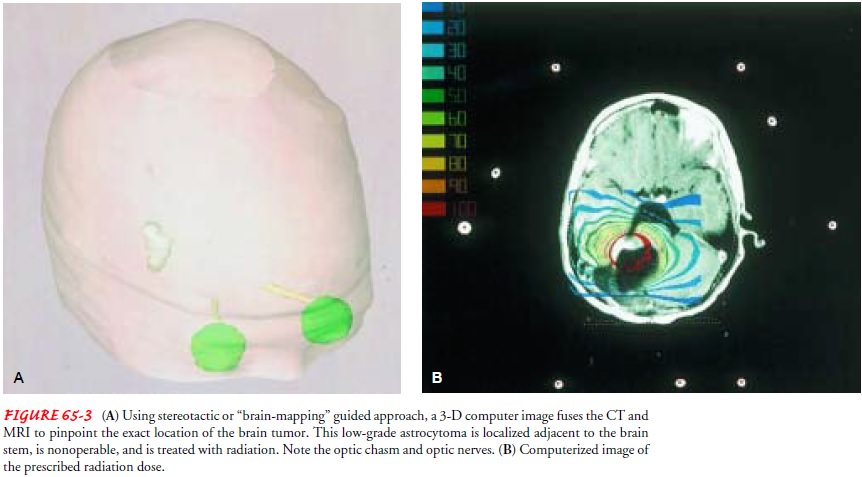
Stereotactic approaches
involve use of a three-dimensional frame that allows very precise localization
of the tumor; a stereo-tactic frame and multiple imaging studies (x-rays, CT scans)
are used to localize the tumor and verify its position (Fig. 65-3). New
brain-mapping technology helps determine how close diseased areas of the brain
are to structures essential for normal brain function. Lasers or radiation can
be delivered with stereotactic ap-proaches. Radioisotopes such as iodine 131 (131I)
can also be im-planted directly into the tumor to deliver high doses of
radiation to the tumor (brachytherapy) while minimizing effects on sur-rounding
brain tissue.
The use of the gamma knife
to perform radiosurgery allows deep, inaccessible tumors to be treated, often
in a single session. Precise localization of the tumor is accomplished using
the stereo-tactic approach and by minute measurements and precise posi-tioning
of the patient. Multiple narrow beams then deliver a very high dose of
radiation. An advantage of this method is that no surgical incision is needed;
a disadvantage is the lag time between treatment and the desired result
(Rafferty-Mitchell, Scanlon & Laskowski-Jones, 1999).
Nursing Management
The patient with a brain tumor may be at an increased
risk for as-piration due to cranial nerve dysfunction. Preoperatively, the gag
reflex and ability to swallow are evaluated. In patients with di-minished gag
response, care includes teaching the patient to direct food and fluids toward
the unaffected side, having the patient sit upright to eat, offering a semisoft
diet, and having suction readily available. Function should be reassessed
postoperatively because changes can occur.
The nurse performs
neurologic checks, monitors vital signs, maintains a neurologic flow chart,
spaces nursing interventions to prevent rapid increase in ICP, and re-orients
the patient when necessary to person, time, and place. Pa-tients with changes
in cognition caused by the lesion require frequent reorientation and the use of
orienting devices (personal possessions, photographs, lists, clock),
supervision of and assis-tance with self-care, and ongoing monitoring and
intervention for prevention of injury. Patients with seizures are carefully
mon-itored and protected from injury.
Motor function is checked at intervals because specific
motor deficits may occur, depending on the tumor’s location. Sensory
disturbances are assessed. Speech is evaluated. Eye movement and pupillary size
and reaction may be affected by cranial nerve in-volvement. In one study that
examined the experience of brain tumor patients 3 to 5 days postoperatively,
the basic needs of patients were met, but changes suggested included minimizing
the atmosphere of urgency and hurry, appointing a primary nurse for each
patient, and giving more postoperative information (Lepola et al., 2001).
Related Topics