Chapter: Medical Surgical Nursing: Management of Patients With Oncologic or Degenerative Neurologic Disorders
HuntingtonŌĆÖs Disease
HUNTINGTONŌĆÖS DISEASE
HuntingtonŌĆÖs disease is
a chronic, progressive, hereditary disease of the nervous system that results
in progressive involuntary cho-reiform movement and dementia. It affects men
and women of all races. Because it is transmitted as an autosomal dominant
ge-netic disorder, each child of a parent with HuntingtonŌĆÖs disease has a 50%
risk of inheriting the illness (Bradley et al., 2000).
Pathophysiology
The basic pathology involves premature death of cells in the stria-tum (caudate and putamen) of the basal ganglia, the region deep within the brain involved in the control of movement. There is also loss of cells in the cortex, the region of the brain associated with thinking, memory, perception, and judgment, and in the cerebellum, the area that coordinates voluntary muscle activity.
Researchers now believe that a
building block for protein called glutamine abnormally collects in the cell
nucleus, causing cell death. The reason that the protein destroys only certain
brain cells is unknown. The cellsŌĆÖ destruction results in a lack of the
neurotransmitters gamma-aminobutyric acid (GABA) and acetyl-choline, which
inhibit nerve action (Bradley et al., 2000). Onset usually occurs between the
ages of 35 and 45 years, although about 10% of patients are children. The
disease progresses slowly. Despite a ravenous appetite, patients usually become
emaciated and exhausted. Patients succumb in 10 to 20 years to heart failure,
pneumonia, or infection, or as a result of a fall or choking.
Clinical Manifestations
The most prominent
clinical features of the disease are abnormal involuntary movements (chorea), intellectual decline, and,
often, emotional disturbance. As the disease progresses, a constant writhing,
twisting, uncontrollable movement may involve the entire body. These motions
are devoid of purpose or rhythm, although patients may try to turn them into
purposeful move-ment. All of the body musculature is involved. Facial movements
produce tics and grimaces. Speech is affected, becoming
slurred, hesitant, often explosive, and eventually unintelligible. Chewing and
swallowing are difficult, and there is a constant danger of choking and
aspiration. Choreiform movements persist but di-minish during sleep.
As with speech, the gait becomes disorganized to the
point that ambulation eventually is impossible. Although independent ambulation
should be encouraged for as long as possible, a wheel-chair usually becomes
necessary. Eventually, the patient is con-fined to bed when the chorea
interferes with walking, sitting, and all other activities. Bladder and bowel
control is lost.
Cognitive function is
usually affected, with dementia usually occurring. Initially, the patient generally
is aware that the disease is responsible for the myriad dysfunctions that are
occurring. The mental and emotional changes that occur may be more devastat-ing
to the patient and family than the abnormal movements. Per-sonality changes may
result in nervous, irritable, or impatient behaviors. In the early stages,
patients are particularly subject to uncontrollable fits of anger, profound,
often suicidal depression, apathy, anxiety, psychosis, or euphoria (Hofmann,
1999). Judg-ment and memory are impaired, and dementia eventually ensues.
Hallucinations, delusions, and paranoid thinking may precede the appearance of
disjointed movements. Emotional symptoms often become less acute as the disease
progresses.
Assessment and Diagnostic Findings
The diagnosis is made
based on the clinical presentation of char-acteristic symptoms, a positive
family history, and exclusion of other causes. Imaging studies, such as CT and
MRI, may show atrophy of the caudate nuclei once the disease is well
established (Bradley et al., 2000).
A genetic marker for
HuntingtonŌĆÖs has been identified through the use of recombinant DNA technology.
As a result, re-searchers can now identify presymptomatic individuals who will
develop this disease. Although this presymptomatic test can re-move the
uncertainty, it offers no hope of cure or even specific prediction of the
timing of its onset. Researchers continue to study the genetic causes that lead
to the death of brain cells (Bradley et al., 2000).
Management
Although no treatment halts or reverses the underlying
process, several methods of management have fairly good palliative results
(Bradley et al., 2000; Sawle, 1999). Thiothixene hydrochloride (Navane) and
haloperidol decanoate (Haldol), which predomi-nantly block dopamine receptors, improve
the chorea in many patients (Bradley et al., 2000). Chorea also is lessened by
reser-pine (depletes presynaptic dopamine) and tetrabenazine (reduces
dopaminergic transmission). Motor signs must be assessed and evaluated on an
ongoing basis so that optimal therapeutic drug levels can be reached. Akathisia (motor restlessness) in the
over-medicated patient is dangerous because it may be mistaken for the restless
fidgeting of the illness and consequently can be over-looked.
In certain types of the
disease, hypokinetic motor impairment resembles parkinsonism. In patients who
present with rigidity, some temporary benefit may be obtained from
antiparkinson medication, such as levodopa.
Patients who have emotional disturbances, particularly
de-pression, may be helped by antidepressant medications. The threat of suicide
is always present. Psychotic symptoms usuallyrespond to antipsychotic
medications. Psychotherapy aimed at allaying anxiety and reducing stress may be
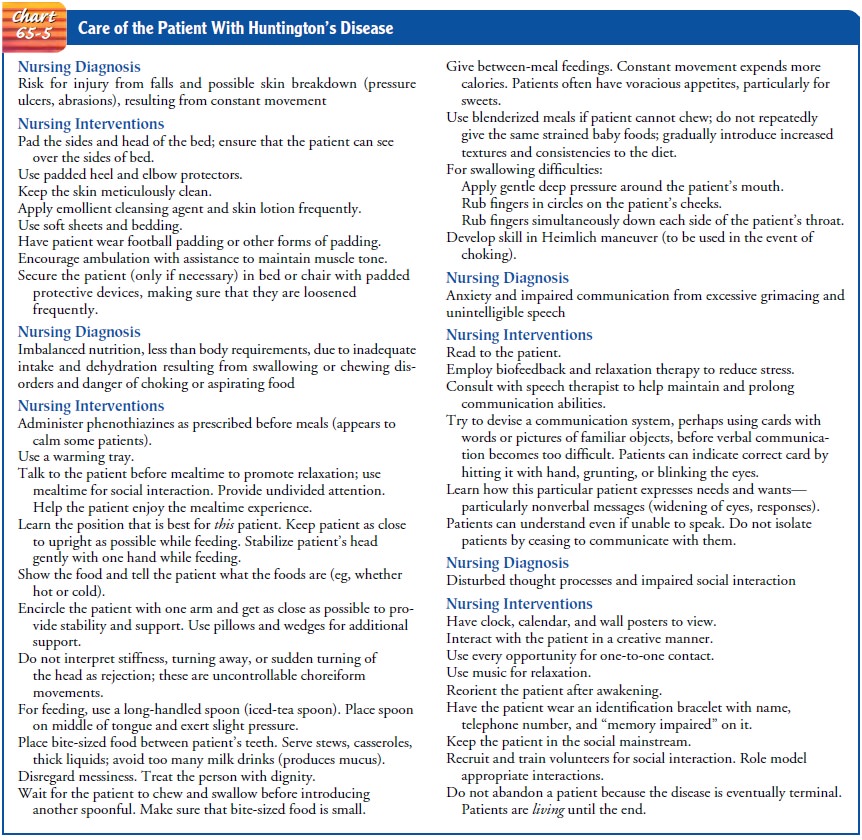
beneficial (Hofman, 1999). It is imperative that nurses look beyond the disease
to focus on the patientŌĆÖs needs and capabilities (Chart 65-5). One study showed
improved physical, mental, and social functioning in a small group of patients
with HuntingtonŌĆÖs disease using re-motivation therapy and providing a more
stimulating environ-ment (Sullivan, Bird, Alpay et al., 2001). Surgically
implanted fetal neural allografts are being tested in hopes of improving the
functional, motor, and cognitive function of patients (Bachoud-Levi, Remy,
Nguyen et al., 2000; Diederich & Goetz, 2000).
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care.
The needs of the patient and fam-ily for education
depend on the nature and severity of physical, cognitive, and psychological
changes experienced by the patient. Patients and family members are taught
about the medications prescribed and about signs indicating a need for change
in med-ication or dosage. The teaching plan addresses strategies to man-age
symptoms such as chorea, swallowing problems, limitations in ambulation, and
loss of bowel and bladder function. Con-sultation with a speech therapist may
be indicated to assist in identifying alternative communication strategies if
speech is affected.
Individuals of child-bearing age often seek information about
their risk for transmitting the disease. Even though presympto-matic testing
has been offered since 1986, approximately 75% of individuals at risk choose
not to be tested (Hayden, 2000). For most people, the benefits of testing are
unclear because of ethical and confidentiality issues. Genetic counseling is
crucial following testing, and patients and their families may require
long-term psychological counseling and emotional, financial, and legal sup-port
(Williams, Schutte, Evers et al., 2000).
Continuing Care.
A program combining medical, nursing,
psy-chological, social, occupational, speech, and physical rehabilita-tion
services is needed to help the patient and family cope with this severely
disabling illness. HuntingtonŌĆÖs exacts enormous emotional, physical, social,
and financial tolls on every member of the patientŌĆÖs family. The family often
live under a heavy burden of uncertainty, anxiety, and guilt. Regular follow-up
helps to allay the fear of abandonment.
Home care assistance,
day care centers, respite care, and even-tually skilled long-term care can
assist the patient and family in coping with the constant strain of the
illness. Although the re-lentless progression of the disease cannot be halted,
families can benefit from supportive care.
Voluntary organizations
can be major aids to families and have been largely responsible for bringing
the illness to national atten-tion. The HuntingtonŌĆÖs Disease Foundation of
America helps pa-tients and families by providing information, referrals,
family and public education, and support for research.
Related Topics