Chapter: Medical Surgical Nursing: Management of Patients With Oncologic or Degenerative Neurologic Disorders
Nursing Process: The Patient With ParkinsonŌĆÖs Disease
NURSING PROCESS: THE PATIENT WITH
PARKINSONŌĆÖS DISEASE
Assessment
Assessment focuses on
how the disease has affected the patientŌĆÖs activities of daily living and
functional abilities. Patients are ob-served for degree of disability and the
functional changes that occur throughout the day, such as responses to
medication. Nearly every patient with a movement disorder has some functional
alteration and may have some type of behavioral dysfunction. The following
questions may be useful to assess alterations:
┬Ę
Do you have leg or arm
stiffness?
┬Ę
Have you experienced any
irregular jerking of your arms or legs?
┬Ę
Have you ever been ŌĆ£frozenŌĆØ or
rooted to the spot and un-able to move?
┬Ę
Does your mouth water
excessively? Have you (or others) noticed yourself grimacing or making faces or
chewing movements?
┬Ę
What specific activities do
you have difficulty doing?
During this assessment, the nurse observes the patient for quality of speech, loss of facial expression, swallowing deficits (drooling, poor head control, coughing), tremors,
slowness of movement, weakness, forward posture, rigidity, evidence of men-tal
slowness, and confusion. Parkinsonian symptoms, as well as side effects of
medications, put these patients at high risk of falls; therefore, a fall risk
assessment should be included (Gray & Hildebrand, 2000).
Diagnosis
NURSING DIAGNOSES
Based on the assessment data, the patientŌĆÖs major nursing
diag-noses may include the following:
┬Ę
Impaired physical mobility
related to muscle rigidity and motor weakness
┬Ę
Self-care deficits (feeding,
dressing, hygiene, and toileting) related to tremor and motor disturbance
┬Ę
Constipation related to
medication and reduced activity
┬Ę
Imbalanced nutrition, less
than body requirements, related to tremor, slowness in eating, difficulty in
chewing and swallowing
┬Ę
Impaired verbal communication
related to decreased speech volume, slowness of speech, inability to move
facial muscles
┬Ę
Ineffective coping related to
depression and dysfunction due to disease progression
Other nursing diagnoses may include sleep pattern
distur-bances, deficient knowledge, risk for injury, risk for activity
in-tolerance, disturbed thought processes, and compromised family coping.
Planning and Goals
The goals for the
patient may include improving functional mo-bility, maintaining independence in
activities of daily living, achieving adequate bowel elimination, attaining and
maintaining acceptable nutritional status, achieving effective communication,
and developing positive coping mechanisms.
Nursing Interventions
IMPROVING MOBILITY
A progressive program of
daily exercise will increase muscle strength, improve coordination and
dexterity, reduce muscular rigidity, and prevent contractures that occur when
muscles are not used. Walking, riding a stationary bicycle, swimming, and
gardening are all exercises that help maintain joint mobility. Stretching
(stretchŌĆōholdŌĆōrelax) and range-of-motion exercises promote joint flexibility.
Postural exercises are important to counter the tendency of the head and neck
to be drawn forward and down. A physical therapist may be helpful in developing
an individualized exercise program and can provide instruction to the patient
and caregiver on exercising safely. Faithful adherence to an exercise and
walking program helps to delay the progress of the disease. Warm baths and
massage in addition to passive and active exercises help relax muscles and
relieve painful muscle spasms that accompany rigidity.
Balance may be adversely
affected because of the rigidity of the arms (arm swinging is necessary in
normal walking). Special walking techniques must be learned to offset the
shuffling gait and the tendency to lean forward. The patient is taught to
con-centrate on walking erect, to watch the horizon, and to use a wide-based
gait (ie, walking with the feet separated). A conscious effort must be made to
swing the arms, raise the feet while walking,and to use a heel-toe placement of
the feet with long strides. The patient is advised to practice walking to
marching music or to the sound of a ticking metronome because this provides
sensory re-inforcement. Doing breathing exercises while walking helps to move
the rib cage and to aerate parts of the lungs. Frequent rest periods aid in
preventing frustration and fatigue.
ENHANCING SELF-CARE ACTIVITIES
Encouraging, teaching,
and supporting the patient during activ-ities of daily living promote
self-care.
Environmental modifications are necessary to compensate
for functional disabilities. Patients may have severe mobility prob-lems that
make normal activities impossible. Adaptive or assistive devices may be useful.
A hospital bed at home with bedside rails, an overbed frame with a trapeze, or
a rope tied to the foot of the bed can provide assistance in pulling up without
help. An occu-pational therapist can evaluate the patientŌĆÖs needs in the home
and make recommendations regarding adaptive devices and teach the patient and
caregiver how to improvise.
IMPROVING BOWEL ELIMINATION
The patient may have
severe problems with constipation. Among the factors causing constipation are
weakness of the muscles used in defecation, lack of exercise, inadequate fluid
intake, and de-creased autonomic nervous system activity. The medications used
for the treatment of the disease also inhibit normal intestinal se-cretions. A
regular bowel routine may be established by encour-aging the patient to follow
a regular time pattern, consciously increase fluid intake, and eat foods with a
moderate fiber content. Laxatives should be avoided. Psyllium, for example,
decreases con-stipation but carries the risk for bowel obstruction (Herndon et
al., 2000). A raised toilet seat is useful because the patient has diffi-culty
in moving from a standing to a sitting position.
IMPROVING NUTRITION
Patients may have
difficulty maintaining their weight. Eating be-comes a very slow process,
requiring concentration due to a dry mouth from medications and difficulty
chewing and swallowing. They are at risk for aspiration because of impaired
swallowing and the accumulation of saliva. They may be unaware that they are
aspirating, and subsequently bronchopneumonia may develop.
Monitoring weight on a
weekly basis indicates whether caloric intake is adequate. Supplemental
feedings increase caloric intake. As the disease progresses, a nasogastric tube
or percutaneous en-doscopic gastroscopy may be necessary to maintain adequate nu-trition.
A dietitian can be consulted regarding nutritional needs.
ENHANCING SWALLOWING
Swallowing disorders can be due to poor head control, tongue tremor, hesitancy in initiating swallowing, difficulty in shaping food into a bolus, and disturbances in pharyngeal motility. To offset these problems, the patient should sit in an upright posi-tion during mealtime. A semisolid diet with thick liquids is easier to swallow than solids; thin liquids should be avoided. It is help-ful for patients to think through the swallowing sequence. The patient is taught to place the food on the tongue, close the lips and teeth, lift the tongue up and then back, and swallow. The pa-tient is encouraged to chew first on one side of the mouth and then on the other. To control the buildup of saliva, the patient is reminded to hold the head upright and make a conscious effort to swallow. Massaging the facial and neck muscles before meals may be beneficial.
ENCOURAGING THE USE OF ASSISTIVE DEVICES
An electric warming tray keeps food hot and permits the
patient to rest during the prolonged time that it takes to eat. Special
uten-sils also assist at mealtime. A plate that is stabilized, a nonspill cup,
and eating utensils with built-up handles are useful self-help devices. The
occupational therapist can assist in identifying appropriate adaptive devices.
IMPROVING COMMUNICATION
Speech disorders are
present in most patients with ParkinsonŌĆÖs disease. Their low-pitched,
monotonous, soft speech requires that they make a conscious effort to speak
slowly, with deliberate at-tention to what they are saying. Patients are
reminded to face the listener, exaggerate the pronunciation of words, speak in
short sentences, and take a few deep breaths before speaking.
A speech therapist may be helpful in designing speech
im-provement exercises and assisting the family and health care per-sonnel to
develop and use a method of communication to meet the patientŌĆÖs needs. A small
electronic amplifier is helpful if the patient has difficulty being heard.
SUPPORTING COPING ABILITIES
Support can be given by
encouraging the patient and pointing out that activities are being maintained
through active participa-tion. A combination of physiotherapy, psychotherapy,
medica-tion therapy, and support group participation may help reduce the
depression that often occurs.
Patients often feel embarrassed, apathetic, inadequate,
bored, and lonely. These feelings may be due, in part, to physical slow-ness
and the great effort that even small tasks require. Patients are assisted and
encouraged to set achievable goals (eg, improvement of mobility).
Because parkinsonism tends to lead to withdrawal and
de-pression, patients must be active participants in their therapeutic program,
including social and recreational events. There should be a planned program of
activity throughout the day to prevent too much daytime sleeping as well as
disinterest and apathy.
Every effort should be
made to encourage patients to carry out the tasks involved in meeting their own
daily needs and to remain independent. Doing things for the patient merely to
save time is contrary to the basic goal of improving coping abilities and
pro-moting a positive self-concept.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
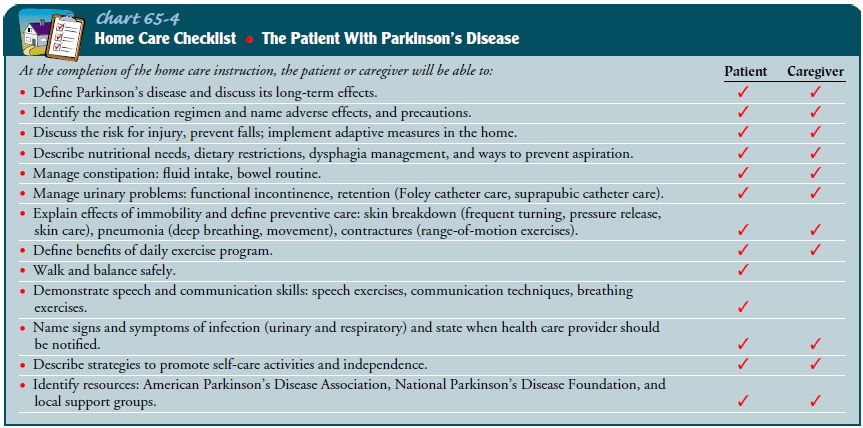
Patient and family
education is important in the management of ParkinsonŌĆÖs disease. Teaching needs
depend on the severity of symptoms and the stage of the disease. Care must be
taken not to overwhelm the patient and family with too much information early
in the disease process. The patientŌĆÖs and familyŌĆÖs need for information is
ongoing as adaptations become necessary. The education plan should include a
clear explanation of the disease, assisting the patient to remain functionally
independent as long as possible. Every effort is made to explain the nature of
the dis-ease and its management to offset disabling anxieties and fears. The
patient and family must be taught about the effects and side effects of
medications and about the importance of reporting side effects to the physician
(Chart 65-4).
Continuing Care
In the early stages
patients can be managed well at home. Family members often serve as caregivers,
with home care or community services available to assist in meeting health care
needs as the dis-ease progresses. The family caregiver may be under
considerable stress from living with and caring for a person with a significant
disability. Providing information about treatment and care pre-vents many
unnecessary problems. The caregiver is included in the plan and may be advised
to learn stress reduction techniques, to include others in the caregiving
process, to obtain periodic re-lief from responsibilities, and to have a yearly
health assessment. Allowing family members to express feelings of frustration,
anger, and guilt is often helpful to them.
The patient should be
evaluated in the home for adaptation and safety needs and compliance with the
plan of care. In the ad-vanced stages, patients usually enter long-term care
facilities when family support is absent. Periodically, admission to an acute
care facility may be necessary for changes in medical management or treatment
of complications. Nurses provide support, education, and monitoring of patients
over the course of illness.
The nurse involved in
home and continuing care needs to remind patients and family members of the
need to address health promotion needs such as screening for hypertension and
stroke risk assessments in this predominantly elderly popula-tion. Patients who
have not been involved in these practices in the past are educated about their
importance and are referred to appropriate health care providers. Informational
booklets and a newsletter for patient education are published by the National
ParkinsonŌĆÖs Foundation, Inc. and the American ParkinsonŌĆÖs Disease Association.
Evaluation
EXPECTED PATIENT OUTCOMES
Expected patient outcomes may include:
1) Strives
toward improved mobility
a) Participates
in exercise program daily
b) Walks
with wide base of support; exaggerates arm swing-ing when walking
c) Takes
medications as prescribed
2) Progresses
toward self-care
a) Allows
time for self-care activities
b) Uses
self-help devices
3) Maintains
bowel function
a) Consumes
adequate fluid
b) Increases
dietary intake of fiber
c) Reports
regular pattern of bowel function
4) Attains
improved nutritional status
a) Swallows
without aspiration
b) Takes
time while eating
5) Achieves
a method of communication
a) Communicates
needs
b) Practices
speech exercises
6) Copes
with effects of ParkinsonŌĆÖs disease
a) Sets
realistic goals
b) Demonstrates
persistence in meaningful activities
c) Verbalizes
feelings to appropriate person
Related Topics