Chapter: Medical Surgical Nursing: Management of Patients With Oncologic or Degenerative Neurologic Disorders
Nursing Process: The Patient With Cerebral Metastases or Incurable Brain Tumor
NURSING PROCESS: THE PATIENT WITH
CEREBRAL METASTASES OR INCURABLE BRAIN TUMOR
Assessment
The nursing assessment
includes a baseline neurologic examina-tion and focuses on how the patient is
functioning, moving, and walking; adapting to weakness or paralysis and to
visual and speech loss; and dealing with seizures. Assessment addresses
symptoms that cause distress to the patient, including pain, respiratory
problems, bowel and bladder disorders, sleep disturbances, and impairment of
skin integrity, fluid balance, and temperature reg-ulation. Tumor invasion,
compression, or obstruction may cause these disorders.
Nutritional status is assessed because cachexia (weak and
ema-ciated condition) is common in patients with metastases. The nurse explores
changes associated with poor nutritional status (anorexia, pain, weight loss,
altered metabolism, muscle weakness, malabsorption, and diarrhea) and asks the
patient about altered taste sensations that may be secondary to dysphagia,
weakness, and depression and about distortions and impaired sense of smell
(anosmia).
The nurse takes a dietary history to assess food intake,
intol-erance, and preferences. Calculation of body mass index can con-firm the
loss of subcutaneous fat and lean body mass. Biochemical measurements (albumin,
transferrin, total lympho-cyte count, creatinine index, and urinary tests) are
reviewed to as-sess the degree of malnutrition, impaired cellular immunity, and
electrolyte balance. A dietitian assists in determining the caloric needs of
the patient.
The nurse works with
other members of the health care team to assess the impact of the illness on
the family in terms of home care, altered relationships, financial problems,
time pressures, and family problems. This information is important in helping
family members cope with the diagnosis and changes associated with it.
Diagnosis
NURSING DIAGNOSES
Based on the assessment data, the patient’s major nursing
diag-noses may include the following:
·
Self-care deficit (feeding,
bathing, and toileting) related to loss or impairment of motor and sensory
function and de-creased cognitive abilities
·
Imbalanced nutrition, less
than body requirements, related to cachexia due to treatment and tumor effects,
decreased nutritional intake, and malabsorption
·
Anxiety related to fear of
dying, uncertainty, change in ap-pearance, altered lifestyle
·
Interrupted family processes
related to anticipatory grief and the burdens imposed by the care of the person
with a terminal illness
Other nursing diagnoses
of the patient with cerebral metas-tases may include acute pain related to
tumor compression; im-paired gas exchange related to dyspnea; constipation
related to decreased fluid and dietary intake and medications; impaired
uri-nary elimination related to reduced fluid intake, vomiting, and reactions
to medications; sleep pattern disturbances related to dis-comfort and fear of
dying; impairment of skin integrity related to cachexia, poor tissue perfusion,
and decreased mobility; deficient fluid volume related to fever, vomiting, and
low fluid intake; and ineffective thermoregulation related to hypothalamic
involve-ment, fever, and chills.
Planning and Goals
The goals for the patient may include compensating for
self-care deficits, improving nutrition, reducing anxiety, enhancing fam-ily
coping skills, and absence of complications.
Nursing Interventions
COMPENSATING FOR SELF-CARE DEFICITS
The patient may have
difficulty participating in goal setting as the tumor metastasizes and affects
cognitive function. It is important to encourage the family to keep the patient
as independent as pos-sible for as long as possible. Increasing assistance with
self-care ac-tivities is required. Because the patient with cerebral metastasis
and the family live with uncertainty, they are encouraged to plan for each day
and to make the most of each day. The tasks and challenges are to assist the
patient to find useful coping mecha-nisms, adaptations, and compensations in
solving problems that arise. This helps patients maintain some sense of
control. An in-dividualized exercise program helps maintain strength,
endurance, and range of motion. Eventually, referral for home or hospice care
may be necessary.
IMPROVING NUTRITION
Patients with nausea, vomiting, diarrhea, breathlessness,
and pain are rarely interested in eating (Wilkes, 2000). These symptoms are
managed or controlled through assessment, planning, and care. The nurse teaches
the family how to position the patient for comfort during meals. Meals are
planned for the times the pa-tient is rested and in less distress from pain or
the effects of treatment.
The patient needs to be
clean, comfortable, and free of pain for meals, in an environment that is as
attractive as possible. Oral hygiene before meals helps to improve intake.
Offensive sights, sounds, and odors are eliminated. Creative strategies may be
re-quired to make food more palatable, provide enough fluids, and increase
opportunities for socialization during meals. The family may be asked to keep a
daily weight chart and to record the quan-tity of food eaten to determine the
daily calorie count. Dietary supplements, if acceptable to the patient, can be
provided to meet increased caloric needs. If the patient is not interested in
most usual foods, those foods preferred by the patient should be of-fered. When
the patient shows marked deterioration as a result of tumor growth and effects,
some other form of nutritional support (eg, tube feeding, parenteral nutrition)
may be indicated if con-sistent with the patient’s end-of-life preferences.
Nursing inter-ventions include assessing the patency of the central and IV line
or feeding tube, monitoring the insertion site for infection, check-ing the
infusion rate, monitoring intake and output, and chang-ing the IV tubing and
dressing. Family members are instructed in these techniques if they will be
providing care at home. Par-enteral nutrition can also be provided at home if
indicated.
The patient’s quality of
life may guide the selection, initiation, and maintenance of nutritional
support. The nurse and family should not place too much emphasis on eating or
on discussions about food as the patient may not desire aggressive nutritional
in-tervention. The subsequent course of action must be congruent with the
wishes and choices of the patient and family.
RELIEVING ANXIETY
Patients with cerebral
metastases may be restless, with changing moods that may include intense
depression, euphoria, paranoia, and severe anxiety. The response of patients to
terminal illness re-flects their pattern of reaction to other crisis
situations. Serious illness imposes additional strains that often bring other
unre-solved problems to light. The patient’s own coping strategies can help
deal with anxious and depressed feelings. Caregivers need to be sensitive to
the patient’s concerns and fears.
Patients need the
opportunity to exercise some control over their situation. A sense of mastery
can be gained as they learn to understand the disease and its treatment and how
to deal with their feelings. The presence of family, friends, a spiritual
advisor, and health professionals may be supportive. Support groups such as the
Brain Tumor Support Group may provide a feeling of sup-port and strength.
Spending time with
patients allows them time to talk and to communicate their fears and concerns.
Open communication and acknowledging fears are often therapeutic. Touch is also
a form of communication. These patients need reassurance that continuing care
will be provided and that they will not be aban-doned. The situation becomes
more endurable when others share in the experience of dying. If a patient’s
emotional reactions are very intense or prolonged, additional help from a
spiritual advi-sor, social worker, or mental health professional may be
indicated.
ENHANCING FAMILY PROCESSES
The family needs to be reassured that their loved one is receiving optimal care and that attention will be paid to the patient’s changing symptoms and to their concerns. When the patient can no longer carry out self-care, the family, additional support sys-tems (social worker, home health aid, home care nurse, hospice nurse) may be needed. A nursing goal is to keep anxiety at a man-ageable level.
PROMOTING HOME AND COMMUNITY-BASED CARE
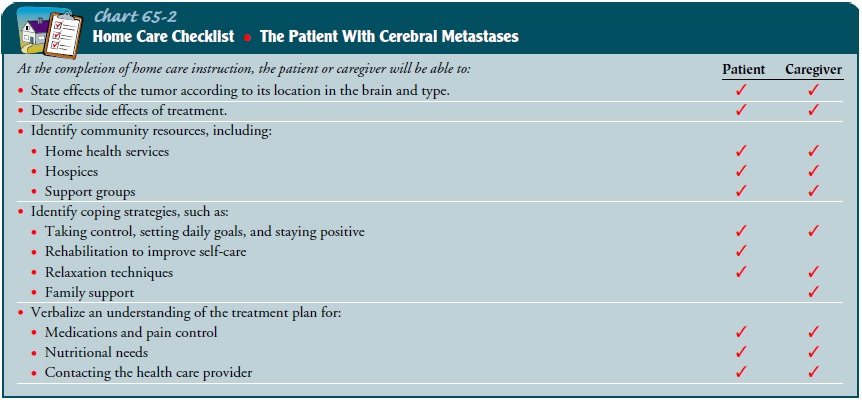
Teaching Patients Self-Care
The patient and family often have major responsibility
for care at home. Therefore, teaching includes strategies of pain manage-ment,
prevention of complications related to treatment strate-gies, and methods to
ensure adequate fluid and food intake (Chart 65-2). Teaching needs of the
patient and family regarding care priorities are likely to change as the
disease progresses. It is important to assess the changing needs of the patient
and the family and to inform them about resources and services early to assist
them to deal with changes in the patient’s condition.
Continuing Care
Home care nursing and
hospice services are valuable resources that should be made available to the
patient and the family early in the course of a terminal illness. Anticipating
needs before they occur can assist in smooth initiation of services. Home care
needs and interventions focus on four major areas: palliation of symp-toms and
pain control, assistance in self-care, control of treatment complications, and
administration of specific forms of treatment, such as parenteral nutrition.
The home care nurse assesses pain management, respiratory status, complications
of the disorder and its treatment, and the patient’s cognitive and emotional
sta-tus. Additionally, the nurse assesses the family’s ability to perform
necessary care and notifies the physician about changing needs or complications
if indicated.
The patient and family who elect to care for the patient
at home as the disease progresses benefit from the care and support provided
through hospice services. Steps to initiate hospice care, including discussion
of hospice care as an option, should not be postponed until death is imminent.
Exploration of hospice care as an option should be initiated at a time when
hospice care can provide support and care to the patient and family consistent
with their end-of-life decisions and assist in allowing death with dignity.
Evaluation
EXPECTED PATIENT OUTCOMES
Expected patient outcomes may include:
1) Engages
in self-care activities as long as possible
a) Uses
assistive devices or accepts assistance as needed
b) Schedules
periodic rest periods to permit maximal par-ticipation in self-care
2) Maintains
as optimal a nutritional status as possible
a) Eats
and accepts food within limits of condition and preferences
b) Accepts
alternative methods of providing nutrition if indicated
3) Reports
being less anxious
a) Is
less restless and is sleeping better
b) Verbalizes
concerns and fears about death
c) Participates
in activities of personal importance as long as feasible
4) Family
members seek help as needed
a) Demonstrate
ability to bathe, feed, and care for the pa-tient and participate in pain
management and preven-tion of complications
b) Express
feelings and concerns to appropriate health professionals
c) Discuss
and seek hospice care as an option
Related Topics