Chapter: Medical Surgical Nursing: Management of Patients With Oncologic or Degenerative Neurologic Disorders
Herniation of a Lumbar Disk
HERNIATION OF A LUMBAR DISK
Most lumbar disk herniations occur at the L4-5 or the
L5-S1 interspaces (Humphreys & Eck, 1999). A herniated lumbar disk produces
low back pain accompanied by varying degrees of sen-sory and motor impairment.
Clinical Manifestations
The patient complains of
low back pain with muscle spasms, followed by radiation of the pain into one
hip and down into the leg (sciatica). Pain is aggravated by actions that
increase intra-spinal fluid pressure (bending, lifting, straining, as in
sneezing and coughing) and usually is relieved by bed rest. Usually there is
some type of postural deformity, because pain causes an alteration of the
normal spinal mechanics. If the patient lies on the back and attempts to raise
a leg in a straight position, pain radiates into the leg because this maneuver,
called the straight leg-raising test, stretches the sciatic nerve. Additional
signs include muscle weak-ness, alterations in tendon reflexes, and sensory
loss.
Assessment and Diagnostic Findings
The diagnosis of lumbar disk disease is based on the
history and physical findings and the use of imaging techniques such as MRI,
CT, and myelography.
Medical Management
The objectives of
treatment are to relieve pain, slow disease pro-gression, and increase the
patient’s functional ability. Bed rest for 1 to 2 days on a firm mattress (to
limit spinal flexion) is encour-aged to reduce the weight load and
gravitational forces, thereby freeing the disk from stress (Humphrey & Eck,
1999). The pa-tient is allowed to assume a comfortable position; usually, a
semi-Fowler’s position with moderate hip and knee flexion relaxes the back
muscles. When the patient is in a side-lying position, a pil-low is placed
between the legs. To get out of bed, the patient lies on one side while pushing
up to a sitting position.
Because muscle spasm is
prominent during the acute phase, muscle relaxants are used. NSAIDs and
systemic corticosteroids may be administered to counter the inflammation that
usually occurs in the supporting tissues and the affected nerve roots. Moist
heat and massage help to relax spastic muscles and have a sedative effect.
Antidepressant agents appear to help in low back pain that is neuropathic in
origin (Fishbain, 2000).
SURGICAL MANAGEMENT
In the lumbar region,
surgical treatment includes lumbar disk ex-cision through a posterolateral
laminotomy and the newer tech-niques of microdiscectomy and percutaneous
discectomy. In microdiscectomy, an operating microscope is used to visualize
the offending disk and compressed nerve roots; it permits a small in-cision
(2.5 cm [1 inch]) and minimal blood loss and takes about 30 minutes of
operating time. Generally, it involves a short hos-pital stay, and the patient
makes a rapid recovery. Percutaneous discectomy is an alternative treatment for
herniated intervertebral disks of the lumbar spine at the L4-5 level. One
approach in cur-rent use is through a 2.5-cm (1-inch) incision just above the
iliac crest. A tube, trocar, or cannula is inserted under x-ray guidance
through the retroperitoneal space to the involved disk space. Spe-cial
instruments are used to remove the disk. The operating time is about 15
minutes. Blood loss and postoperative pain are min-imal, and the patient is
generally discharged within 2 days after surgery. The disadvantage of this
procedure is the possibility of damage to structures in the surgical pathway.
Complications
of Disk Surgery.A patient undergoing a
disk pro-cedure at one level of the vertebral column may have a degenera-tive
process at other levels. A herniation relapse may occur at the same level or
elsewhere, so that the patient may become a candi-date for another disk
procedure. Arachnoiditis (inflammation of the arachnoid membrane) may occur
after surgery (and after myelography); it involves an insidious onset of
diffuse, frequently burning pain in the lower back, radiating into the
buttocks. Disk excision can leave adhesions and scarring around the spinal
nerves and dura, which then produce inflammatory changes that create chronic
neuritis and neurofibrosis. Disk surgery may relieve pres-sure on the spinal
nerves, but it does not reverse the effects of neural injury and scarring and
the pain that results. Failed disk syndrome (recurrence of sciatica after lumbar
discectomy) re-mains a common cause of disability.
Nursing Management
PROVIDING PREOPERATIVE CARE
Most patients fear
surgery on any part of the spine and therefore need explanations about the
surgery and reassurance that surgery will not weaken the back. When data are
being collected for the health history, any reports of pain, paresthesia, and
muscle spasm are recorded to provide a baseline for comparison after surgery.
Preoperative assessment also includes an evaluation of movement of the extremities
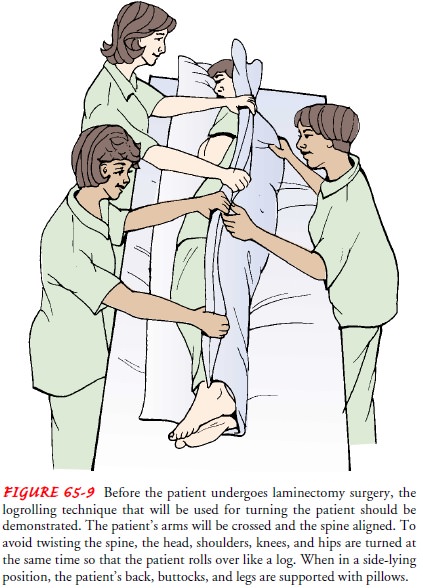
as well as bladder and bowel function. To facil-itate the postoperative turning
procedure, the patient is taught to turn as a unit (called logrolling) as part
of the preoperative prepa-ration (Fig. 65-9). Before surgery, the patient is
also encouraged to take deep breaths, cough, and perform muscle-setting
exercises to maintain muscle tone.
ASSESSING THE PATIENT AFTER SURGERY
After lumbar disk
excision, vital signs are checked frequently and the wound is inspected for
hemorrhage because vascular injury is a complication of disk surgery. Because
postoperative neurologic deficits may occur from nerve root injury, the
sensation and motor strength of the lower extremities are evaluated at
specified inter-vals, along with the color and temperature of the legs and
sensa-tion of the toes. It is important to assess for urinary retention,
another sign of neurologic deterioration.
In discectomy with fusion, the patient has an additional
sur-gical incision if bone fragments were taken from the iliac crest or fibula
to serve as wedges in the spine. The recovery period is longer than for those
patients who underwent discectomy with-out spinal fusion because bony union
must take place.
POSITIONING THE PATIENT
To position the patient, a pillow is placed under the head
and the knee rest is elevated slightly to relax the back muscles. When the
patient is lying on one side, however, extreme knee flexion must be avoided.
The patient is encouraged to move from side to side to relieve pressure and is
reassured that no injury will result from moving. When the patient is ready to
turn, the bed is placed in a flat position and a pillow is placed between the
legs. The patient turns as a unit (logrolls), without twisting the back.
To get out of bed, the patient lies on one side while pushing up to a sitting position. At the same time, the nurse or family member eases the patient’s legs over the side of the bed. Coming to a sitting or standing posture is accomplished in one long, smooth motion. Most patients walk to the bathroom the same day as surgery. Sitting is discouraged except for defecation.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care.
The patient is advised to graduallyincrease
activity as tolerated because it takes up to 6 weeks for the ligaments to heal.
Excessive activity may result in spasm of the paraspinal muscles.
Activities that produce
flexion strain on the spine (eg, driving a car) should be avoided until healing
has taken place. Heat may be applied to the back to relax muscle spasms.
Scheduled rest pe-riods are important, and the patient is advised to avoid
heavy work for 2 to 3 months after surgery. Exercises are prescribed to
strengthen the abdominal and erector spinal muscles. A back brace or corset may
be necessary if back pain persists.
Related Topics