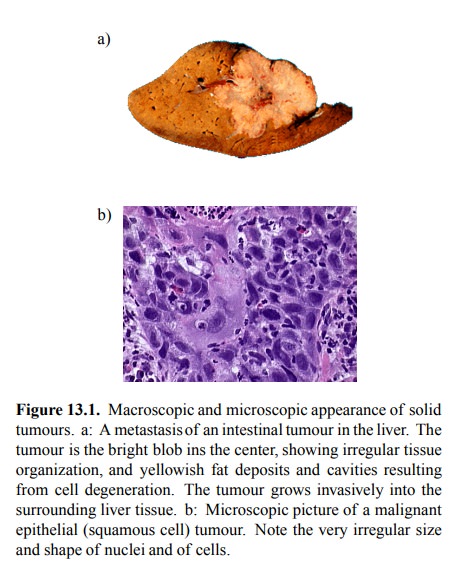
Chapter: Biochemical Pharmacology : Some principles of cancer pharmacotherapy
Some principles of cancer pharmacotherapy
Some principles of cancer
pharmacotherapy
Cancer therapy consists of
surgery, irradiation, and chemotherapy. Cancer chemotherapy is particular and
par-ticularly challenging in several aspects:
• While in most cases the aim of pharmacotherapy
is to modulate cell function, in cancer therapy it is to kill the diseased
cells – no prisoners. Selective killing is quite feasible with bacteria, since
they are prokaryotic, and their biochemical apparatus contains a substantial
num-ber of targets that do not occur in human cells1. It is more
challenging yet possible with fungi and parasites. The latter share with our
own cells the eukaryotic nature, and so inhibitors of ribosomal protein
synthesis, which are very important in antibacterial chemotherapy, are most-ly
useless. However, fungi have ergosterol in their cell membranes instead of cholesterol,
and both ergosterol and its synthesis are targeted by drugs that thus can be
reasonably selective2. In contrast, since tumour cells are derived
from normal body cells, they do not normally possess any particular drug target
that sets them apart from the healthy cells.
• Cancers are diverse – they may be derived from
near-ly any organ, and there are several types of cancers for each organ. This
diversity brings with it an inherent variability in the susceptibility to
chemotherapy. Some cancers are susceptible to many cytotoxic agents and can be
cured quite efficiently; an example is lymphatic leukemia, especially in
childhood that nowadays has a cure rate of approximately 90%. Others – e.g.,
squamous lung cancer – are virtually intractable if not by surgery. In many
cases, the susceptibility cannot be predicted ac-curately beforehand. However,
with an increasing num-ber of tumours (particularly leukemias), genetic
analysis is being used for exact typing, which helps in the selec-tion of
appropriate treatment regimens.
· Cancers, even if typically derived from one
individual transformed cell, are heterogeneous – due to their in-herent genetic
instability. Normal body cells are `good citizens' and obey the commandments
enshrined in the genome; the same set of enzymes and receptors (i.e., drug
targets), with the same regulation and expression levels, can be expected to
occur in any cell of a given type. In contrast, tumours at advanced stages
usually de-velop multiple clones with varying chromosomal dele-tions,
duplications and translocations that can profound-ly change the prevalence of
drug targets and the function of regulatory mechanisms. E.g., breast tumours
that ini-tially are susceptible to hormone withdrawal (or compet-itive hormone
antagonists) frequently give rise to clones that grow without the hormones;
tumours that initially are inhibited by anti-metabolites may develop resistance
by changing expression levels of the enzymes involved.
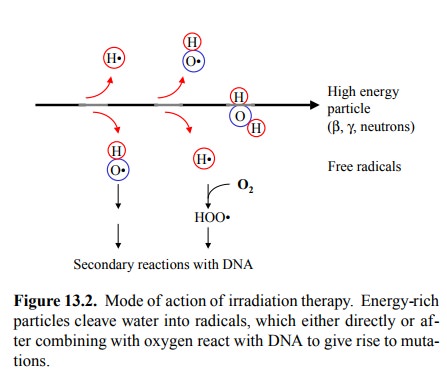
Although we are concerned here with
chemotherapy only, it is worth noting that irradiation therapy also has a
chem-ical mode of action (Figure 13.2): Energy-rich particles (photons in X-
and γ-irradiation, electrons or neutrons in particle irradiation)
dispose of their energy in multiple suc-cessive events, giving rise to multiple
radicals (mostly de-rived from water) along their path. These, in turn, may di
rectly react with macromolecules, or they may react with oxygen to form
superoxide radicals, which have a longer lifetime and thus are more likely to
find biologically signifi-cant targets (mostly DNA) by diffusion. Oxygen
therefore sensitizes cells to radiation, while radical-capturing and re-ducing
compounds (e.g, free thiols) will reduce sensitivity. Radio-sensitizing and
-protecting drugs for use in conjunc-tion with radiation have been investigated
but not found widespread clinical application.
Related Topics