Chapter: Psychiatric Mental Health Nursing : Neurobiologic Theories and Psychopharmacology
Side Effects - Psychopharmacology
Side Effects
Extrapyramidal Side Effects. Extrapyramidal symptoms (EPS), serious neurologic symptoms, are the major side effects of antipsychotic drugs. They
include acute dysto-nia, pseudoparkinsonism, and akathisia. Although often
collectively referred to as EPS, each of these reactions has distinct features.
One client can experience all the reactions in the same course of therapy,
which makes distinguishing among them difficult. Blockade of D2 receptors in
the midbrain region of the brain stem is responsible for the development of
EPS. Conventional antipsychotic drugs cause a greater incidence of EPS than do
atypical antipsychotic drugs, with ziprasidone (Geodon) rarely causing EPS
(Daniel, Copeland, & Tamminga, 2006).
Therapies for acute dystonia, pseudoparkinsonism, and akathisia are
similar and include lowering the dosage of the antipsychotic, changing to a
different antipsychotic, or administering anticholinergic medication
(discussion to follow). Whereas anticholinergic drugs also produce side
effects, atypical antipsychotic medications are often pre-scribed because the
incidence of EPS side effects associ-ated with them is decreased.
Acute dystonia includes
acute muscular rigidity and cramping, a stiff or thick tongue with difficulty
swallow-ing, and, in severe cases, laryngospasm and respiratory dif-ficulties.
Dystonia is most likely to occur in the first week of treatment, in clients
younger than 40 years, in males, and in those receiving high-potency drugs such
as halo-peridol and thiothixene. Spasms or stiffness in muscle groups can
produce torticollis (twisted head and
neck), opisthotonus (tightness in the
entire body with the head back and an
arched neck), or oculogyric crisis
(eyes rolled back in a locked position). Acute dystonic reactions can be
painful and frightening for the client. Immediate treatment with
anticholinergic drugs, such as intramuscular benztro-pine mesylate (Cogentin)
or intramuscular or intravenous diphenhydramine (Benadryl), usually brings
rapid relief.
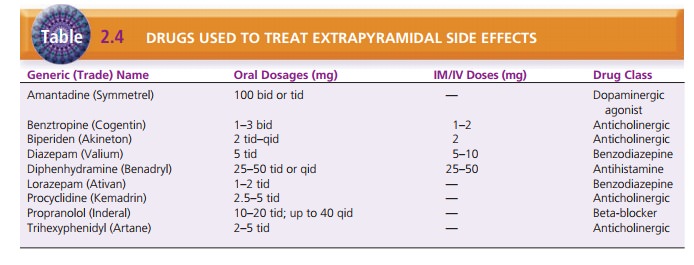
Table 2.4 lists the drugs, and their routes and dosages, used to
treat EPS. The addition of a regularly scheduled oral anticholinergic such as
benztropine may allow the client to continue taking the antipsychotic drug with
no further dystonia. Recurrent dystonic reactions would necessitate a lower
dosage or a change in the antipsychoticdrug.
Drug-induced parkinsonism,
or pseudoparkinsonism, is often
referred to by the generic label of EPS. Symptoms resemble those of ParkinsonŌĆÖs
disease and include a stiff, stooped posture; mask-like facies; decreased arm
swing; a shuffling, festinating gait (with small steps); cogwheel rigid-ity
(ratchet-like movements of joints); drooling; tremor; bradycardia; and coarse
pill-rolling movements of the thumb and fingers while at rest. Parkinsonism is
treated by changing to an antipsychotic medication that has a lower incidence
of EPS or by adding an oral anticholinergic agent or amantadine, which is a
dopamine agonist that increases transmission of dopamine blocked by the
antipsychotic drug.
Akathisia is reported by the client as
an intense need to move about. The
client appears restless or anxious and agitated, often with a rigid posture or
gait and a lack of spontaneous gestures. This feeling of internal restlessness
and the inability to sit still or rest often leads clients to discontinue their
antipsychotic medication. Akathisia can be treated by a change in antipsychotic
medication or by the addition of an oral agent such as a beta-blocker,
anti-cholinergic, or benzodiazepine.
Neuroleptic Malignant Syndrome. Neuroleptic malignant syndrome (NMS) is a potentially fatal idiosyncratic reac-tion to an antipsychotic
(or neuroleptic) drug. Although the Diagnostic
and Statistical Manual of Mental Disorders, 4th edition, Text Revision (American Psychiatric Associa-tion,
2000) notes that the death rate from this syndrome has been reported at 10% to
20%, those figures may have resulted from biased reporting; the reported rates
are now decreasing. The major symptoms of NMS are rigidity; high fever;
autonomic instability such as unstable blood pres-sure, diaphoresis, and
pallor; delirium; and elevated levels of enzymes, particularly creatine
phosphokinase. Clients with NMS usually are confused and often mute; they may
fluctuate from agitation to stupor. All antipsychotics seem to have the
potential to cause NMS, but high dosages ofhigh-potency drugs increase the
risk. NMS most often occurs in the first 2 weeks of therapy or after an
increase in dosage, but it can occur at any time.
Dehydration, poor nutrition, and concurrent medical illness all
increase the risk for NMS. Treatment includes immediate discontinuance of all
antipsychotic medica-tions and the institution of supportive medical care to
treat dehydration and hyperthermia until the clientŌĆÖs physical condition
stabilizes. After NMS, the decision to treat the client with other
antipsychotic drugs requires full discussion between the client and the
physician to weigh the relative risks against the potential benefits of
therapy.
Tardive Dyskinesia. Tardive dyskinesia (TD), a syndro me of permanent involuntary
movements, is most commonly caused by the long-term use of conventional
antipsychotic drugs. About 20% to 30% of patients on long-term treatment
develop symptoms of TD (Sadock & Sadock, 2008). The pathophysiology is
still unclear, and no effective treatment has been approved for general use.
However, Woods, Saksa, Baker, Cohen, and Tek (2008) report success in treating
TD with levetiracetam in clinical trials. The symptoms of TD include
involuntary movements of the tongue, facial and neck muscles, upper and lower
extremities, andtruncal musculature. Tongue thrusting and protruding, lip
smacking, blinking, grimacing, and other excessive unnec-essary facial
movements are characteristic. After it has devel-oped, TD is irreversible,
although decreasing or discontinuing antipsychotic medications can arrest its
progression. Unfor-tunately, antipsychotic medications can mask the beginning
symptoms of TD; that is, increased dosages of the antipsy-chotic medication
cause the initial symptoms to disappear temporarily. As the symptoms of TD
worsen, however, they ŌĆ£break throughŌĆØ the effect of the antipsychotic drug.![]()
![]()
Preventing TD is one goal when administering antipsy-chotics. This
can be done by keeping maintenance dosages as low as possible, changing
medications, and monitoring the client periodically for initial signs of TD
using a stan-dardized assessment tool such as the Abnormal Involun-tary
Movement Scale . Clients who have already developed signs of TD but still need
to take an antipsychotic medication often are given one of the atypi-cal
antipsychotic drugs that have not yet been found to cause or, therefore, worsen
TD.
Anticholinergic side effects
Often occur with the use of antipsychotics and include orthostatic
hypotension, dry mouth, constipation, urinary hesitance or retention, blurred
near vision, dry eyes, pho-tophobia, nasal congestion, and decreased memory.
These side effects usually decrease within 3 to 4 weeks but do not entirely remit.
The client taking anticholinergic agents for EPS may have increased problems
with anticholinergic side effects. Using calorie-free beverages or hard candy
may alleviate dry mouth; stool softeners, adequate fluid intake, and the
inclusion of grains and fruit in the diet may prevent constipation.
Other Side Effects. Antipsychotic drugs also
increase blood prolactin levels. Elevated prolactin may
cause breast enlargement and tenderness in men and women; dimin-ished libido,
erectile and orgasmic dysfunction, and men-strual irregularities; and increased
risk for breast cancer, and may contribute to weight gain.
Weight gain can accompany most antipsychotic medi-cations, but it
is most likely with the atypical antipsy-chotic drugs, with ziprasidone
(Geodon) being the exception. Weight increases are most significant with
clozapine (Clozaril) and olanzapine (Zyprexa). Since 2004, the FDA has made it
mandatory for drug manufac-turers that atypical antipsychotics carry a warning
of the increased risk for hyperglycemia and diabetes. Though the exact
mechanism of this weight gain is unknown, it is associated with increased
appetite, binge eating, carbo-hydrate craving, food preference changes, and
decreased satiety in some clients. In addition, clients with a genetic
predisposition for weight gain are at greater risk (MullerKennedy, 2006).
Prolactin elevation may stimulate feeding centers, histamine antagonism
stimulates appe-tite, and there may be an as yet undetermined interplay of
multiple neurotransmitter and receptor interactions with resultant changes in
appetite, energy intake, and feeding behavior. Obesity is common in clients
with schizophre-nia, further increasing the risk for type 2 diabetes melli-tus
and cardiovascular disease (Newcomer & Haupt, 2006). In addition, clients
with schizophrenia are less likely to exercise or eat low-fat nutritionally
balanced diets; this pattern decreases the likelihood that they can minimize
potential weight gain or lose excess weight. It is recommended that clients
taking antipsychotics be involved in an educational program to control weight
and decrease body mass index.
Most antipsychotic drugs cause relatively minor cardio-vascular
adverse effects such as postural hypotension, palpi-tations, and tachycardia.
Certain antipsychotic drugs, such as thioridazine (Mellaril), droperidol
(Inapsine), and mesoridazine (Serentil), also can cause a lengthening of the QT
interval. A QT interval longer than 500 ms is considered dangerous and is
associated with life-threatening dysrhyth-mias and sudden death. Though rare,
the lengthened QT interval can cause torsade de pointes, a rapid heart rhythm
of 150 to 250 beats per minute, resulting in a ŌĆ£twistedŌĆØ appear-ance on the
electrocardiogram; hence the name torsade de pointes (Glassman, 2005).
Thioridazine and mesoridazine are used to treat psychosis; droperidol is most
often used as an adjunct to anesthesia or to produce sedation. Sertindole
(Serlect) was never approved in the United States to treat psychosis, but was
used in Europe and was subsequently withdrawn from the market because of the
number of cardiac dysrhythmias and deaths that it caused.
Clozapine produces fewer traditional side effects than do most
antipsychotic drugs, but it has the potentially fatal side effect of
agranulocytosis. This develops suddenly and is characterized by fever, malaise,
ulcerative sore throat, and leukopenia. This side effect may not be manifested
immediately and can occur up to 24 weeks after the initia-tion of therapy.
Initially, clients needed to have a weekly white blood cell count (WBC) above
3,500 per mm3 to obtain the next weekŌĆÖs supply of clozapine. Currently,
all clients must have weekly WBCs drawn for the first 6 months. If the WBC is
3,500 per mm3 and the absolute neutrophil count (ANC) is 2,000 per
mm3, the client may have these labs monitored every 2 weeks for 6
months, and then every 4 weeks. This decreased monitoring is dependent on
continuous therapy with clozapine. Any interruption in therapy requires a
return to more frequent monitoring for a specified period of time. After
clozapine has been discontinued, weekly monitoring of the WBC and ANC is required
for 4 weeks.
Related Topics