Chapter: Psychiatric Mental Health Nursing : Neurobiologic Theories and Psychopharmacology
Antidepressant Drugs - Psychopharmacology
Antidepressant Drugs
Antidepressant drugs are primarily used in the
treatment of major depressive
illness, anxiety disorders, the depressed phase of bipolar disorder, and
psychotic depression. Off-label uses of antidepressants include the treatment
of chronic pain, migraine headaches, peripheral and diabetic neuropathies,
sleep apnea, dermatologic disorders, panic disorder, and eating disorders.
Although the mechanism of action is not completely understood, antidepressants
somehow interact with the two neurotransmitters, norepi-nephrine and serotonin,
that regulate mood, arousal, attention, sensory processing, and appetite.
┬Ę
Antidepressants are divided into four groups:
┬Ę
Tricyclic and the related cyclic antidepressants
┬Ę
Selective serotonin reuptake inhibitors (SSRIs)
┬Ę
MAO inhibitors (MAOIs)
┬Ę
Other antidepressants such as venlafaxine desvenlafaxine (Pristiq)
(Effexor), bupropion (Wellbutrin), duloxetine (Cymbalta), trazodone (Desyrel),
and nefazodone (Serzone).
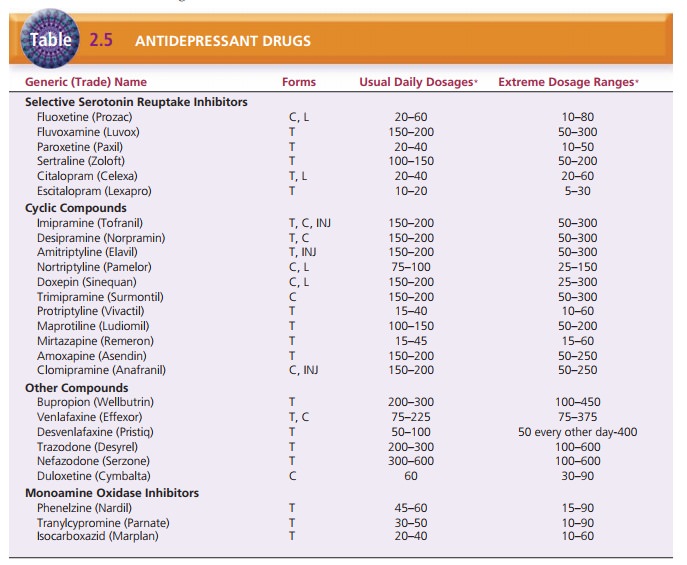
Table 2.5 lists the dosage forms, usual daily dosages, and extreme
dosage ranges.
The cyclic compounds became available in the 1950s and for years
were the first choice of drugs to treat depres-sion even though they cause
varying degrees of sedation, orthostatic hypotension (drop in blood pressure on
rising), and anticholinergic side effects. In addition, cyclic antide-pressants
are potentially lethal if taken in an overdose.
During that same period, the MAOIs were discovered to have a
positive effect on people with depression. Although the MAOIs have a low
incidence of sedation and anticho-linergic effects, they must be used with
extreme caution for several reasons:
A life-threatening side effect, hypertensive crisis, may occur if
the client ingests foods containing tyramine (an amino acid) while taking
MAOIs.
Because of the risk for potentially fatal drug interactions, MAOIs
cannot be given in combination with other MAOIs, tricyclic antidepressants,
meperidine (Demerol), CNS depressants, many antihypertensives, or general
anesthetics.
MAOIs are potentially lethal in overdose and pose a potential risk
in clients with depression who may be considering suicide.![]()
![]()
The SSRIs, first available in 1987 with the release of fluoxetine
(Prozac), have replaced the cyclic drugs as the first choice in treating
depression because they are equal in efficacy and produce fewer troublesome
side effects. The SSRIs and clomipramine are effective in the treatment of OCD
as well. Prozac Weekly is the first and only medication that can be given once
a week as main-tenance therapy for depression after the client has been
stabilized on fluoxetine. It contains 90 mg of fluoxetine with an enteric
coating that delays release into the bloodstream.
Preferred Drugs for Clients at High Risk for Suicide
Suicide is always a primary consideration when treating clients
with depression. SSRIs, venlafaxine, nefazodone, and bupropion are often better
choices for those who are potentially suicidal or highly impulsive because they
carry no risk of lethal overdose, in contrast to the cyclic com-pounds and the
MAOIs. However, SSRIs are effective only for mild and moderate depression.
Evaluation of the risk for suicide must continue even after treatment with
anti-depressants is initiated. The client may feel more energized but still
have suicidal thoughts, which increases the likeli-hood of a suicide attempt.
Also, because it often takes weeks before the medications have a full
therapeutic effect, clients may become discouraged and tired of waiting to feel
better, which can result in suicidal behavior. There is an FDA-required warning
for SSRIs and increased suicidal risk in children and adolescents.
Mechanism of Action
The precise mechanism by which antidepressants produce their
therapeutic effects is not known, but much is known about their action on the
CNS. The major interaction is with the monoamine neurotransmitter systems in
the brain, particularly norepinephrine and serotonin. Both of these
neurotransmitters are released throughout the brain and help to regulate
arousal, vigilance, attention, mood, sensory processing, and appetite.
Norepinephrine, sero-tonin, and dopamine are removed from the synapses after
release by reuptake into presynaptic neurons. After reuptake, these three
neurotransmitters are reloaded for subsequent release or metabolized by the
enzyme MAO. The SSRIs block the reuptake of serotonin, the cyclic
anti-depressants and venlafaxine block the reuptake of norepi-nephrine
primarily and block serotonin to some degree, and the MAOIs interfere with
enzyme metabolism. This is not the complete explanation, however; the blockade
of serotonin and norepinephrine reuptake and the inhibition of MAO occur in a
matter of hours, whereas antidepres-sants are rarely effective until taken for
several weeks. The cyclic compounds may take 4 to 6 weeks to be effective,
MAOIs need 2 to 4 weeks for effectiveness, and SSRIs may be effective in 2 to 3
weeks. Researchers believe that the actions of these drugs are an ŌĆ£initiating
eventŌĆØ and that eventual therapeutic effectiveness results when neurons respond
more slowly, making serotonin available at the synapses (Lehne, 2006).
Side Effects of Selective Serotonin Reuptake Inhibitors
SSRIs have fewer side effects compared with the cyclic compounds.
Enhanced serotonin transmission can lead to several common side effects such as
anxiety, agitation, akathisia (motor restlessness), nausea, insomnia, and
sex-ual dysfunction, specifically diminished sexual drive or difficulty
achieving an erection or orgasm. In addition, weight gain is both an initial
and ongoing problem during antidepressant therapy, although SSRIs cause less
weight gain than other antidepressants. Taking medications with food usually
can minimize nausea. Akathisia usually is treated with a beta-blocker such as
propranolol (Inderal) or a benzodiazepine. Insomnia may continue to be a
prob-lem even if the client takes the medication in the morning; a
sedative-hypnotic or low-dosage trazodone may be needed.
Less common side effects include sedation (particularly with paroxetine [Paxil]), sweating, diarrhea, hand tremor, and headaches. Diarrhea and headaches usually can be managed with symptomatic treatment. Sweating and con-tinued sedation most likely indicate the need for a change to another antidepressant.
Side Effects of Cyclic Antidepressants
Cyclic compounds have more side effects than do SSRIs and the newer
miscellaneous compounds. The individual medications in this category vary in
terms of the intensity of side effects, but generally side effects fall into
the same categories. The cyclic antidepressants block cholinergic receptors,
resulting in anticholinergic effects such as dry mouth, constipation, urinary
hesitancy or retention, dry nasal passages, and blurred near vision. More
severe anti-cholinergic effects such as agitation, delirium, and ileus may
occur, particularly in older adults. Other common side effects include
orthostatic hypotension, sedation, weight gain, and tachycardia. Clients may
develop toler-ance to anticholinergic effects, but these side effects are
common reasons that clients discontinue drug therapy. Clients taking cyclic
compounds frequently report sexual dysfunction similar to problems experienced
with SSRIs. Both weight gain and sexual dysfunction are cited as com-mon
reasons for noncompliance (Stahl, 2006).
Side Effects of Monoamine
Oxidase Inhibitors
The most common side effects of MAOIs include daytime sedation,
insomnia, weight gain, dry mouth, orthostatic hypotension, and sexual
dysfunction. The sedation and insomnia are difficult to treat and may
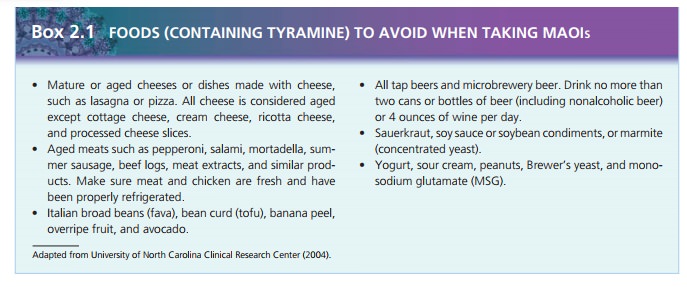
necessitate a change in medication. Of particular concern with MAOIs is the
potential for a life-threatening hypertensive crisis if the client ingests food
that contains tyramine or takes sympathomimetic drugs. Because the enzyme MAO
is necessary to break down the tyramine in certain foods, its inhibition
results in increased serum tyramine levels, causing severe hypertension,
hyperpyrexia, tachycardia, diaphoresis, tremulousness, and cardiac
dysrhythmias. Drugs that may cause potentially fatal interactions with MAOIs
include SSRIs, certain cyclic compounds, buspirone (BuSpar), dextromethorphan,
and opiate deriva-tives such as meperidine. The client must be able to follow a
tyramine-free diet;
Studies are currently underway to determine whether a selegiline
transdermal patch would be effective in treating depression without the risks
of dietary tyramine and orally ingested MAOIs.
Side Effects of Other Antidepressants
Of the other or novel antidepressant medications, nefa-zodone,
trazodone, and mirtazapine commonly cause seda-tion. Both nefazodone and trazodone
commonly cause headaches. Nefazodone also can cause dry mouth and nau-sea.
Bupropion and venlafaxine desvenlafaxine may cause loss of appetite, nausea,
agitation, and insomnia. Venlafax-ine also may cause dizziness, sweating, or
sedation. Sexual dysfunction is much less common with the novel
antide-pressants, with one notable exception: Trazodone can cause priapism (a
sustained and painful erection that necessitates immediate treatment and
discontinuation of the drug). Priapism also may result in impotence.
Drug Interactions
An uncommon but potentially serious drug interaction, called serotonin syndrome (or serotonergic
syndrome), can result from taking an MAOI and an SSRI at the same time. It also
can occur if the client takes one of these drugs too close to the end of
therapy with the other. In other words, one drug must clear the personŌĆÖs system
before ini-tiation of therapy with the other. Symptoms include agita-tion,
sweating, fever, tachycardia, hypotension, rigidity, hyperreflexia, and, in extreme
reactions, even coma and death (Krishnan, 2006). These symptoms are similar to
those seen with an SSRI overdose.
Client Teaching
Clients should take SSRIs first thing in the morning unless
sedation is a problem; generally, paroxetine most often causes sedation. If the
client forgets a dose of an SSRI, he or she can take it up to 8 hours after the
missed dose. To minimize side effects, clients generally should take cyclic
compounds at night in a single daily dose when possible. If the client forgets
a dose of a cyclic compound, he or she should take it within 3 hours of the
missed dose or omit the dose for that day. Clients should exercise caution when
driving or performing activities requiring sharp, alert reflexes until sedative
effects can be determined.
Clients taking MAOIs need to be aware that a life-threatening
hyperadrenergic crisis can occur if they do not observe certain dietary
restrictions. They should receive a written list of foods to avoid while taking
MAOIs. The nurse should make clients aware of the risk for serious or even
fatal drug interactions when taking MAOIs and instruct them not to take any
additional medication, including over-the-counter preparations, without
check-ing with the physician or pharmacist.
Related Topics