Chapter: Essential Anesthesia From Science to Practice : Clinical management : Vascular access and fluid management
Risks - Fluid management
Risks
Blood
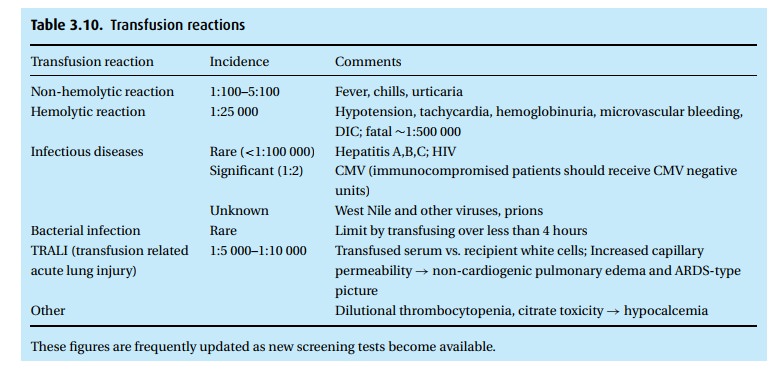
transfusions are inherently dangerous (Table 3.10).
In addition to the frequent non-hemolytic reactions, ABO incompatibility
threatens the poten-tial of a hemolytic reaction with hypotension, hematuria,
and fever. The diag-nosis can be made more readily if the patient is awake
since the symptoms of nausea, vomiting, flank or back pain and dizziness
frequently accompany a transfusion reaction.
Therapy includes stopping the infusion immediately (we return
both the remaining banked blood and a sample from the patient for testing),
treating mild symptoms with antihistamines and acetaminophen to reduce fever,
and perhaps adding corticosteroids to reduce the immune response. We worry most
about the potential for shock, kidney failure, and dissemi-nated intravascular
coagulation (DIC). In this last nasty syndrome, the antigen/ antibody reaction
can trigger factor XII (Hageman) which kicks the kinin system into action
leading to the generation of bradykinin and, through it, damage of endothelium
(oozing), hypotension, and thrombosis via the release of endo-genous tissue
thromboplastin. Human error plays a large part in transfusion reac-tions, which
account for more than half of transfusion-related deaths . . . transla-tion, double check all blood (patient and donor
blood types) before transfusing!
Unfortunately,
there are several types of transfusion reactions, and some can manifest even
several days after the transfusion.
As we
are largely water, maintenance of the patient’s fluid status represents one of
anesthesiology’s greatest challenges. Using vigilance, anticipation,
appropriate monitors, and vascular access, we manage fluids, blood, and blood
products to maintain stability and perfusion of vital organs.
Related Topics