Chapter: Essential Anesthesia From Science to Practice : Clinical management : Regional anesthesia
Regional anesthesia
Regional
anesthesia
We can
imagine future clinicians to prescribe treatments that would exclusively affect
a single cell type or a specific organ without spillover effects. That type of
explicit therapy would be the opposite to general anesthesia, the name of which
implies generalized effects of the anesthetic drugs. Indeed, anesthetics
delivered via the lungs or by intravenous injection flood all organs in the
body, causing numerous undesired effects. How much better to pinpoint the
effect with regional anesthesia. Here, we deliver the drug directly to the
nervous tissue where we hope to cause a specific effect. We are closer to the
ideal but not quite in heaven because we still have to contend with side
effects that arise when the anesthetic drug appears in the circulation. We also
lack the specificity of drugs that would block only one type of fiber and spare
all others. Nevertheless, regional anesthesia provides a tool that can be used
to great advantage for many patients.
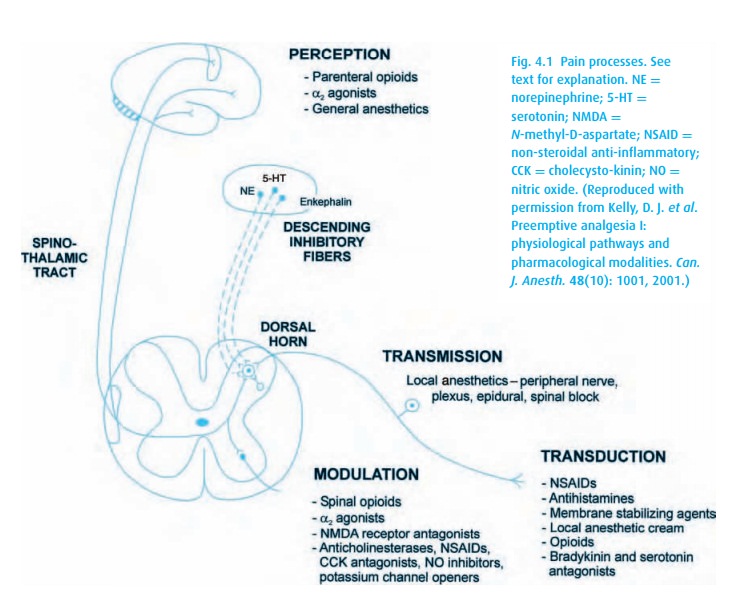
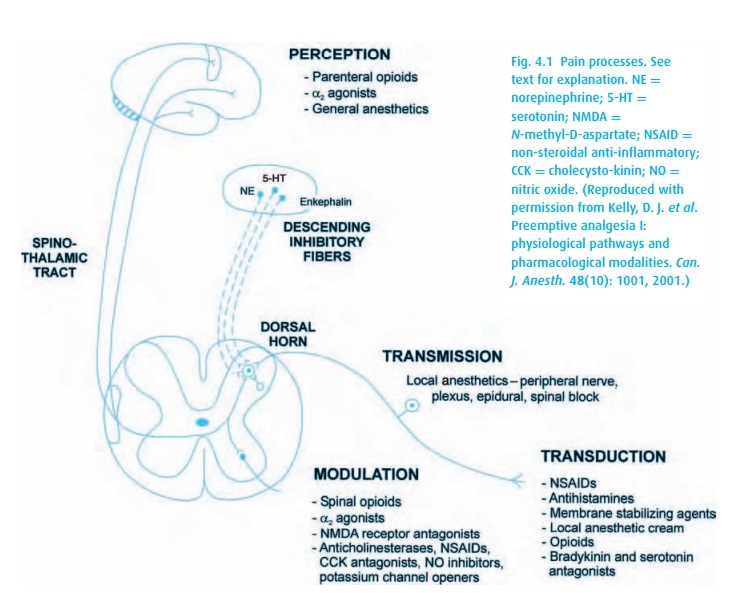
Four
distinct processes lead to the sensation of pain (Fig. 4.1):
·
Transduction Noxious stimulation of a peripheral receptor
releases localinflammatory mediators that cause changes in the activity and
sensitivity of sensory neurons. Pre-incisional
infiltration of local anesthetics effectively blocks transduction.
·
Transmission Once the noxious stimulus has been transduced,
the impulsestravel via A-delta and C fibers to the dorsal horn of the spinal
column where they synapse. The dorsal horn cells may be subject to “wind-up” or
enhanced excitability and sensitization. Transmission can be blocked with
regional anesthesia.
·
Perception Afferent fibers from the dorsal horn travel to
higher CNS cen-ters, mostly via the spinothalamic tracts. Activation of the
reticular forma-tion probably increases arousal and contributes the emotional
component of pain. Central-acting agents such as opioids alter perception.
·
Modulation Efferent pathways including inhibitory
neurotransmitters mod-ify the afferent nociceptive information.
The complexity of pain perception goes beyond this quick anatomic/physiologic summary. Strong emotional stimuli and distraction can completely block pain perception, as is often true for injuries sustained in battle (or when being eaten by a lion). Thus, in addition to the described processes of getting the signal from injured tissue to the brain, psychological factors modulate the pain experience.
While we
can interfere with the impulses traveling up the nervous pathways at any stage,
mounting evidence suggests that multi-modal and pre-emptive (before incision)
therapy can both improve immediate post-operative pain control and reduce the
risk of a subsequent chronic pain syndrome.
Transduction
of superficial noxious stimuli can be inhibited with pre-incisional local
infiltration. As the name implies, regional anesthesia involves anesthetiz-ing
a specific portion of the body, thereby preventing transmission. Because pain
sensation travels via nerves (A-delta and C fibers to be specific) from the
site of the injury to the spinal cord (dorsal columns) and then up to the
brain, the nerve impulse can be interrupted at numerous sites. Consider an
operation on the big toe. Local anesthetic infiltration suffices for only the
most superficial of procedures. For anything deeper, we make use of our
knowledge of the area’s innervation and the anatomic course of the nerves
through the body. Sensory impulses can be interrupted in several locations
including the ankle, popliteal fossa, sciatic notch, or at the spinal cord
level. The first three would be considered peripheral nerve blocks because they
block the transmission of the “pain mes-sage” before it reaches the central
nervous system. We can also block the message at the level of the central
nervous system with an epidural anesthetic (which could be a caudal block), or
a spinal (properly called a subarachnoid) block. Together, these last
approaches are called neuraxial anesthesia. And all can be effective for big
toe surgery.
When
used for operative anesthesia, we typically supplement a regional block with
sedation; the patient need not be aware during the procedure. A balance must be
struck between the patient’s comfort, and the side effects of sedation,
primarily respiratory depression. Also, all our sedatives, even midazolam
(Versed®), linger and produce a hangover effect. Therefore, the patient will
not be fully functional following the procedure, or even for the remainder of
the day. Some patients do not like this feeling and would prefer the reassuring
conversation of a caring anesthesiologist over drug-induced anxiolysis.
We may
be tempted to choose regional anesthesia for patients with cardio-vascular or
pulmonary problems, arguing that a properly conducted regional technique
stresses these systems less than does a general anesthetic. Be careful! If the
regional block is unsuccessful, if there are complications, or if the block
wears off during the operation, the patient may require emergency general
anesthe-sia and possibly also tracheal intubation. Similarly, regional
anesthesia must be used with caution in patients with a recognized “difficult
airway.” If we fear diffi-culty managing the patient’s airway, we would be
ill-advised to perform a regional anesthetic to “avoid the airway” without
adequate preparation (additional airway equipment, etc.).
Related Topics