Chapter: Essential Anesthesia From Science to Practice : Clinical management : Regional anesthesia
Local anesthetic toxicity
Local anesthetic toxicity
Local
anesthetics exhibit dose-related toxicity. Therefore, concerns about poten-tial
toxicity grow with increasing doses of local anesthetic (see also
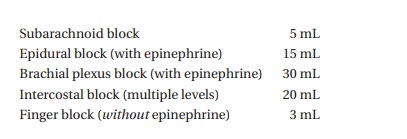
Pharmacology). Typical volumes of local anesthetics used for various blocks
follow (we use lidocaine 1.5% as an example):
Of
these, intercostal nerve blocks lead to the highest local anesthetic blood
levels and therefore are most likely to cause toxicity, because multiple small
depots of the local anesthetic offer a relatively large surface for absorption
of the drug into blood vessels. In order to reduce the rate of absorption, we
often add 1:200 000 epinephrine (5 mcg/mL) to the local anesthetic, which not
only reduces the absorption of the drug and thus the chance of toxicity, but
also prolongs the anesthetic effect.
An added
advantage of the epinephrine: should the injection be inadvertently
intravascular (as into an epidural vein), the prompt development of
epinephrine-induced tachycardia will give a clear signal.
Either
an inadvertent intravascular injection or rapid absorption of properly placed
local anesthetic can trigger toxic manifestations. We reduce this risk by
dividing the dose into multiple smaller boluses, looking for signs of toxicity
in-between. Early typical symptoms include a metallic taste, ringing in the
ears, and tingling around the mouth. Sleepiness or mental status changes often
accom-pany these symptoms. Central nervous system toxicity progresses to seizures
(treated with small intravenous doses
of thiopental or a benzodiazepine) and eventual coma. Cardiovascular effects
include hypotension due to vasodilation and myocardial depression, but may
progress to complete cardiovascular col-lapse. This is particularly true with
bupivacaine, whose slow unbinding from sodium receptors causes stubborn
ventricular arrhythmias. However, eventually the drug will give way. Therefore,
do not give up on resuscitative efforts.
As with
all emergencies, the treatment includes the common sense steps, such as to stop
injecting and then to follow the standard ABCs of basic life support. “A”
(airway) and “B” (breathing with oxygen) are particularly important since
hypoxia and acidosis worsen the toxicity. It sounds obvious, but do not use
lidocaine to treat local anesthetic-induced ventricular arrhythmias! Use
amiodarone (start with 1mg/kg slowly i.v.) instead.
Anesthesiologists
skilled in both regional and general techniques offer patients a broad range of
options for their operation. Regional anesthesia occupies a niche in outpatient
surgery, where rapid awakening and minimal nausea/vomiting are sought. In many
procedures, regional with light general anesthesia provides good operative
conditions for the surgeon and excellent postoperative analgesia. Regional
anesthesia plays a growing role in postoperative pain management for
outpatients and for the care of some patients with chronic pain.
Related Topics