Chapter: Essential Anesthesia From Science to Practice : Clinical management : Vascular access and fluid management
Pulmonary artery catheterization - Vascular access
Pulmonary artery catheterization
In
addition to the risks of central venous catheterization listed above, pulmonary
artery (PA) catheterization has caused catastrophic pulmonary artery rupture
and
Thus, this invasive technique requires rigorous
justifi-cation. Do you really need to have PA pressure, PA occlusion pressure
(PAOP, also known as pulmonary capillary wedge pressure, PCWP), or cardiac
output? And how will it affect your management?
After
placing an introducer (a special large-bore central venous catheter) via the
central venous access technique above, a PAC is sterilely inserted through the
introducer.
(i) Prepare the catheter: flush and cap the PAC
ports. Test the balloon for symmet-ric inflation and passive deflation on
release of the syringe pressure. Connect the PA distal port to a pressure transducer with the monitor in view.
Cover the catheter with the clear plastic sheath3
that maintains internal sterility for subsequent manipulation of catheter
depth.
(ii) Advance the catheter through the introducer to
20 cm and confirm the CVP waveform on the monitor (see below). Instruct an
assistant to inflate the balloon.
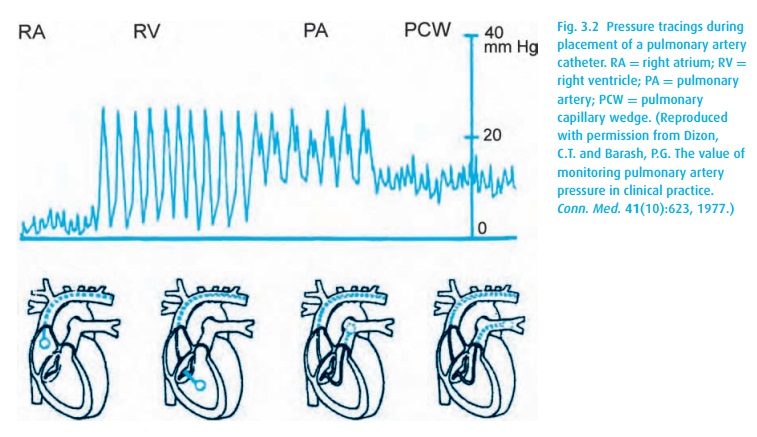
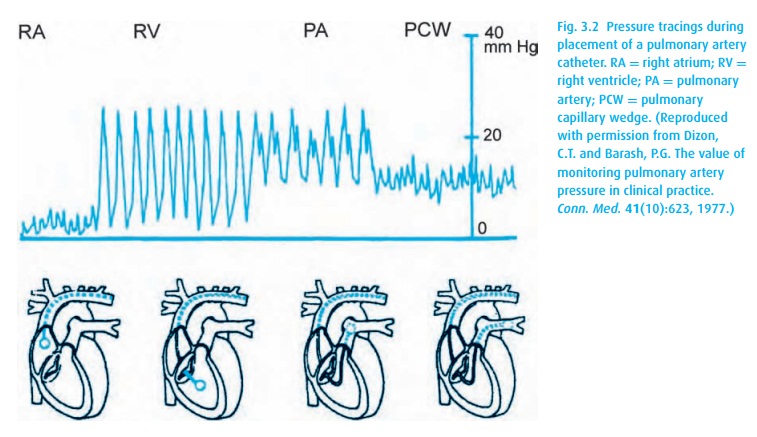
(iii) Advance the catheter while keeping track of its
depth as well as the waveform transduced from its tip (Fig. 3.2). The RV tracing should appear before the
catheter has been advanced about 30 cm, and the PAOP before 50 cm. If they do
not, deflate the balloon, pull back the catheter 10 cm or so, reinflate the balloon
and try again. Over-insertion can result in a knot, necessitating a vascular
procedure to remove the catheter.
(iv) Once the PAOP tracing is obtained, deflate the
balloon and confirm reappear-ance of the PA trace. If this does not occur, you
must withdraw the catheter a few centimeters. Continue manipulation until the
PA trace with the balloon deflated becomes the PAOP (or wedge) trace on
inflation. Always inflate the balloon to just barely occlude the PA pressure in
order to avoid rupturing the vessel. And remember . . . balloon up on catheter advancement, balloon downon withdrawal.
(v) Aspirate to confirm intravascular location, and
flush all ports. Obtain a chest radiograph to confirm proper location (within
the mediastinal shadow).
Related Topics