Chapter: Essential Anesthesia From Science to Practice : Clinical management : Vascular access and fluid management
Peripheral venous cannulation - Vascular access
Peripheral venous cannulation
Let’s go
through the steps involved:
(i) Explain the need for vascular access and obtain consent from the patient.Parents can
be of great help in preparing a child for an i.v.
(ii) Topicalize If there is sufficient time (30–45 minutes), a topical anesthetic
suchas EMLA (eutectic mixture of local anesthetics) can be applied to the
intended site. In our practice, this is only worthwhile for small children.
(iii)
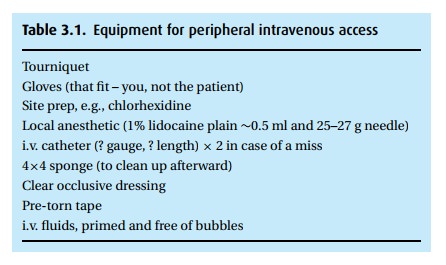
Acquire equipment (Table 3.1) Weusually select the largest catheter appro-priate for the selected
vein.
(iv) Don clean gloves They need not be sterile. From now on, you are dealing withthe
patient’s blood, and you should expose neither yourself nor the patient to the
possibility of infection.
(v)Select the site This involves more than just looking for the most visible vein.We
often use the back of the hand because veins are both visible and easy to
immobilize. Things to consider: use the non-dominant hand, avoid “creases”
where kinking is likely, e.g., wrist, seek a relatively straight vein without
venous valves that may hinder its cannulation; inserting at a venous fork is helpful
as the vein tends to be better stabilized. Finally, we do not cannulate an arm
that has been the target of an arteriovenous shunt (as for dialysis) or a lymph
node dissection (as in a mastectomy).
(vi) Apply a tourniquet Should be tight enough to obstruct venous return withoutrestricting
arterial flow. Do not actually tie a knot, just fold one side under the other.
(vii)
Prepare the site We prefer to use a bactericidal agent such as
chlorhexidine;next best would be an iodine-containing solution, e.g., betadine,
which must be allowed to dry and should not be wiped off with alcohol. Finally,
a patient allergic to both of the above should be washed with alcohol alone.
(viii) Inject local anesthetic Awake patients benefit greatly if we take the
time to first anesthetize their skin. It requires only a tiny volume (∼0.1 mL) of local anesthetic injected
immediately adjacent to (not over) the vein, minimizing the risk of obscuring
visibility of the vein. While injection of lidocaine burns, we can reduce the
discomfort by:
Counter-irritation
– with a free finger, scratch the patient’s skin near the injection site, this
“confuses” the nerve endings and reduces pain.
Alkalinize
the lidocaine – add 1 mL bicarbonate (8.4%) to every 10 mL lidocaine.
Some
argue that using local anesthesia insures two sticks instead of one, and that a
“needle is a needle.” We beg to differ: first, the local should be administered
with a 25–27 g needle, which is barely felt by most patients; second, the i.v.
does not always go in on the first try; and third, the pain of the needle
without local is worse than the local anesthetic injection (personal
experience).
(ix) Stabilize the vein with traction below the puncture site.
(x)Puncture the skin at a 30–45-degree angle (through the local anestheticwheal!).
(xi) Proceed into the vein either directly from above or from the side; make sureyou can see
the plastic hub of the needle to observe the return of blood.
(xii)
Advance catheter When you see a flash of blood, reduce your
angle andadvance a tiny amount (literally 1–2 mm), then feed the catheter off
the needle. Fully advance the catheter before pulling out the needle. You
cannot thread the flexible catheter without the stiff needle as a stylet, and
the needle cannot be reinserted as the catheter may be punctured.
(xiii) Remove the tourniquet (facilitated by proper placement in the first place).
(xiv) Apply gentle pressure over the tip of the catheter to prevent bleedingback
(xv)
Remove the needle and dispose in a “Sharps” container.
(xvi) Connect i.v. fluid administration set and open to observe free flow, thenslow down the
administration as indicated by the patient’s condition.
(xvii) Observe the i.v. site to confirm intravascular and not interstitial placement(not
foolproof but helpful).
(xviii)
Secure the i.v. With due respect to those who consider this
an art form, finda method that allows visibility of the entry site (to observe
for infection) and the area over the tip of the catheter (to detect
infiltration). Secure the i.v. so that motion will not dislodge it. A loop in
the tubing prevents a small amount of traction from pulling directly on the
catheter.
The
fluid administered depends on the goal for the infusion. In general, fluids
should be administered through a programmable pump with adequate safety
measures. That said, in anesthesia we usually control the rate of fluid
adminis-tration through the i.v. tubing’s roller clamp. In this case, do not hang more fluidthan you want the
patient to receive. For an infant, do not hang a liter bag withouta
buretrol (a 150–200 mL reservoir attached between the i.v. fluid bag and the
catheter). If the roller clamp is inadvertently left open, the patient will not
be fluid overloaded.
When we
recognize the potential need for rapid fluid administration (read: major blood
letting), we plan our intravenous access accordingly. The maximum attainable
flow rate depends on the resistance of the system, including the length and
diameter of everything from the tubing to the vein itself. So, remove any small
diameter connectors and select a shorter, larger catheter (at least an 18 g in
an adult).1 Selecting a large
vein for rapid flow is obvious, but the effect of cold fluids may be
underestimated. Finally, two medium bore i.v.s accommodate more fluid than a
single large bore.
Related Topics