Chapter: Clinical Anesthesiology: Anesthetic Equipment & Monitors : Non cardiovascular Monitoring
Pulse Oximetry - Respiratory Gas Exchange Monitors
PULSE OXIMETRY
Indications & Contraindications
Pulse oximeters are mandatory monitors
for any anesthetic, including cases of moderate sedation. There are no
contraindications.
Techniques & Complications
Pulse oximeters combine the principles
of oximetry and plethysmography to noninvasively measure oxygen saturation in
arterial blood. A sensor con-taining light sources (two or three light-emitting
diodes) and a light detector (a photodiode) is placed across a finger, toe,
earlobe, or any other perfused tissue that can be transilluminated. When the
light source and detector are opposite one another across the perfused tissue,
transmittance oximetry is used. When the light source and detector are placed
on the same side of the patient (eg, the forehead), the backscatter
(reflectance) of light is recorded by the detector.
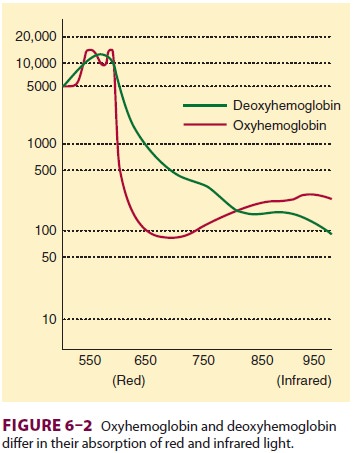
Oximetry depends on the observation that
oxygenated and reduced hemoglobin differ in their absorption of red and
infrared light (Lambert–Beer law). Specifically, oxyhemoglobin (HbO2) absorbs more infrared light (940 nm), whereas
deoxyhemo-globin absorbs more red light (660 nm) and thus appears blue, or
cyanotic, to the naked eye. The change in light absorption during arterial
pulsations is the basis of oximetric determinations (Figure 6–2). The ratio of the
absorptions at the red and infrared wavelengths is analyzed by a microprocessor
to pro-vide the oxygen saturation (Spo2)
of arterial blood based on established norms. The greater the ratio of red/
infrared absorption, the lower the arterial satu-ration. Arterial pulsations
are identified by plethys-mography, allowing corrections for light absorption
by nonpulsating venous blood and tissue. Heat from the light source or sensor
pressure may, rarely, result in tissue damage if the monitor is not
periodically moved. No user calibration is required.
Clinical Considerations
In
addition to Spo2, pulse oximeters provide an indication of tissue
perfusion (pulse amplitude) and measure heart rate. Because Spo2 is
normally close to 100%, only gross abnormalities are detectable in most
anesthetized patients. Depending on a particu-lar patient’s oxygen–hemoglobin
dissociation curve, a 90% saturation may indicate a Pao2 of less
than 65 mm Hg. This compares with clinically detect-able cyanosis, which
requires 5 g of desaturated hemoglobin and usually corresponds to an Spo2
of less than 80%. Bronchial intubation will usually go undetected by pulse
oximetry in the absence of lung disease or low fraction of inspired oxygen
concen-trations (Fio2).
Because
carboxyhemoglobin (COHb) and HbO2 absorb light at 660 nm
identically, pulse oxim-eters that compare only two wavelengths of light will
register a falsely high reading in patients with car-bon monoxide poisoning.
Methemoglobin has the same absorption coefficient at both red and infra-red
wavelengths. The resulting 1:1 absorption ratio corresponds to a saturation
reading of 85%. Thus, methemoglobinemia causes a falsely low satura-tion
reading when Sao2 is actually greater than 85% and a falsely high reading if
Sao2 is actually less than 85%.
Most
pulse oximeters are inaccurate at low Spo2, and all demonstrate a
delay between changes in Sao2 and Spo2. Other causes of
pulse oximetry artifact include excessive ambient light, motion, methy-lene
blue dye, venous pulsations in a dependent limb, low perfusion (eg, low cardiac
output, pro-found anemia, hypothermia, increased systemic vascular resistance),
malpositioned sensor, and leakage of light from the light-emitting diode to the
photodiode, bypassing the arterial bed (opti-cal shunting). Nevertheless, pulse
oximetry can be an invaluable aid to the rapid diagnosis of hypoxia, which may
occur in unrecognized esophageal intu-bation, and it furthers the goal of monitoring
oxygen delivery to vital organs. In the recovery room, pulse oximetry helps
identify postoperative pulmonary problems, such as severe hypoventilation,
broncho-spasm, and atelectasis.
Two
extensions of pulse oximetry technol-ogy are mixed venous blood oxygen
saturation (Svo2) and
noninvasive brain oximetry. The for-mer requires the placement of a pulmonary
artery catheter containing fiberoptic sensors that continu-ously determine Svo2
in a manner analogous to pulse oximetry. Because Svo 2 varies with
changes in hemoglobin concentration, cardiac output, arterial oxygen
saturation, and whole-body oxygen con-sumption, its interpretation is somewhat
complex. A variation of this technique involves placing the fiberoptic sensor
in the internal jugular vein, which provides measurements of jugular bulb
oxygen satu-ration in an attempt to assess the adequacy of cere-bral oxygen
delivery.
Noninvasive
brain oximetry monitors regional oxygen saturation (rSo2) of
hemoglobin in the brain. A sensor placed on the forehead emits light of
spe-cific wavelengths and measures the light reflected back to the sensor
(near-infrared optical spectros-copy). Unlike pulse oximetry, brain oximetry
mea-sures venous and capillary blood oxygen saturation in addition to arterial
blood saturation. Thus, its oxygen saturation readings represent the average
oxygen saturation of all regional microvascular hemoglobin (approximately 70%).
Cardiac arrest, cerebral embolization, deep hypothermia, or severe hypoxia
cause a dramatic decrease in rSo2. (See the section “Neurological
System Monitors.”)
Related Topics