Chapter: Clinical Anesthesiology: Anesthetic Equipment & Monitors : Non cardiovascular Monitoring
Peripheral Nerve Stimulation
PERIPHERAL NERVE STIMULATION
Indications
Because of the variation in patient
sensitivity to neuromuscular blocking agents, the neuromus-cular function of
all patients receiving intermedi-ate- or long-acting neuromuscular blocking
agents should be monitored. In addition, peripheral nerve stimulation is
helpful in assessing paralysis dur-ing rapid-sequence inductions or during
continu-ous infusions of short-acting agents. Furthermore, peripheral nerve
stimulators can help locate nerves to be blocked by regional anesthesia.
Contraindications
Th ere are no contraindications to
neuromuscu-lar monitoring, although certain sites may be pre-cluded by the
surgical procedure. Additionally, atrophied muscles in areas of hemiplegia or
nerve damage may appear refractory to neuromuscular blockade secondary to the
proliferation of receptors. Determining the degree of neuromuscular block-ade
using such an extremity could lead to potential overdosing of competitive
neuromuscular blocking agents.
Techniques & Complications
A peripheral nerve stimulator delivers
current (60-80 mA) to a pair of either ECG silver chloride pads or subcutaneous
needles placed over a peripheral motor nerve. The evoked mechanical or
electri-cal response of the innervated muscle is observed. Although
electromyography provides a fast, accu-rate, and quantitative measure of
neuromuscular transmission, visual or tactile observation of mus-cle contraction
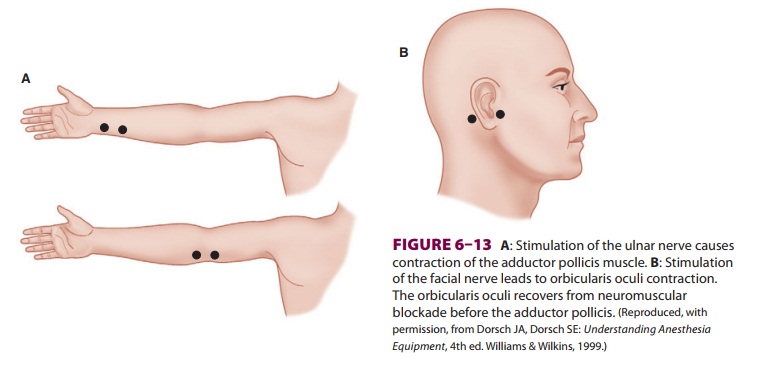
is usually relied upon in clinical practice. Ulnar nerve stimulation of the
adductor pollicis muscle and facial nerve stimulation of the orbicularis oculi
are most commonly monitored (Figure 6–13). Because it is the inhibition of
the
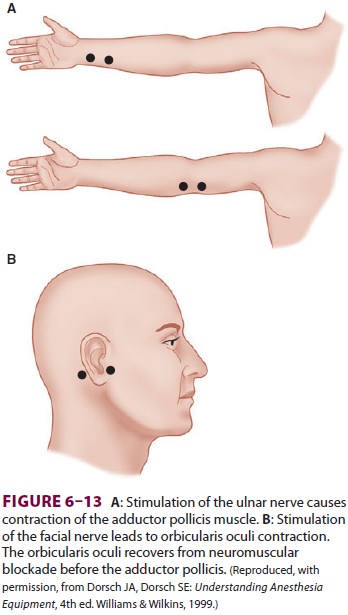
neuromuscular receptor that needs to be
monitored, direct stimulation of muscle should be avoided by placing electrodes
over the course of the nerve and not over the muscle itself. To deliver a
supramaxi-mal stimulation to the underlying nerve, peripheral nerve stimulators
must be capable of generating at least a 50-mA current across a 1000-Ω load. This
current is uncomfortable for a conscious patient. Complications of nerve
stimulation are limited to skin irritation and abrasion at the site of
electrode attachment.
Because of concerns of residual
neuromus-cular blockade, increased attention has been focused on providing
quantitative measures of the degree of neuromuscular blockade perioperatively.
Acceleromyography uses a piezoelectric transducer on the muscle to be
stimulated. Movement of the muscle generates an electrical current that can be
quantified and displayed. Indeed, acceleromyogra-phy can better predict
residual paralysis, compared with routine tactile train-of-four monitoring used
in most operating rooms, if calibrated from the begin-ning of the operative
period to establish baselines prior to administration of neuromuscular blocking
agents.
Clinical Considerations
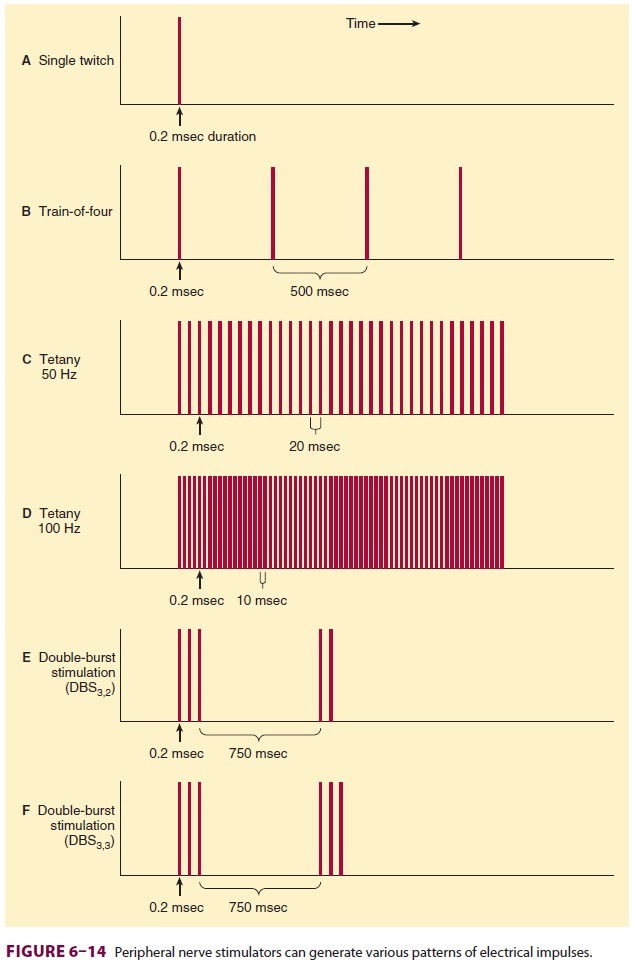
The degree of neuromuscular blockade is
monitored by applying various patterns of electrical stimula-tion (Figure 6–14).
All stimuli are 200 µs in dura-tion and of square-wave pattern and equal
current intensity. A twitch is a single pulse that is delivered from every 1 to
every 10 sec (1–0.1 Hz). Increasing block results in decreased evoked response
to stimulation.
Train-of-four stimulation denotes four
suc-cessive 200-µs stimuli in 2 sec (2 Hz). The twitches in a
train-of-four pattern progressively fade as nondepolarizing muscle relaxant
block increases. The ratio of the responses to the first and fourth twitches is
a sensitive indicator of nondepolarizing muscle paralysis. Because it is
difficult to estimate the train-of-four ratio, it is more convenient to
visually observe the sequential disappearance of the twitches, as this also
correlates with the extent of blockade. Disappearance of the fourth twitch
rep-resents a 75% block, the third twitch an 80% block, and the second twitch a 90% block. Clinical
relax-ation usually requires 75% to 95% neuromuscular blockade.Tetany at 50 or
100 Hz is a sensitive test of neu-romuscular function. Sustained contraction
for 5 sec indicates adequate—but not necessarily complete— reversal from
neuromuscular blockade. Double-burst stimulation (DBS) represents two variations
of tetany that are less painful to the patient. The DBS3,3 pattern of nerve stimulation consists of three
short (200-µs) high-frequency bursts separated by 20 ms
intervals (50 Hz) followed 750 ms later by another three bursts. DBS3,2 consists of three 200-µs impulses at 50 Hz followed 750 ms
later by two such impulses. DBS is more sensitive than train-of-four
stimulation for the clinical (ie, visual) evaluation of fade.Because muscle
groups differ in their sensi-tivity to neuromuscular blocking agents, use of
the peripheral nerve stimulator cannot replace direct observation of the
muscles (eg, the dia-phragm) that need to be relaxed for a specific sur-gical
procedure. Furthermore, recovery of adductor pollicis function does not exactly
paral-lel recovery of muscles required to maintain an airway. The diaphragm,
rectus abdominis, laryngeal adductors, and orbicularis oculi mus-cles recover
from neuromuscular blockade sooner than do the adductor pollicis. Other
indicators of adequate recovery include sustained (≥5 s) head lift, the ability to generate
an inspira-tory pressure of at least –25 cm H2O,
and a force-ful hand grip. Twitch tension is reduced by hypothermia of the
monitored muscle group (6%/°C). Decisions regarding adequacy of rever-sal of
neuromuscular blockade, as well as timing of extubation, should be made only by
consider-ing both the patient’s clinical presentation and assessments
determined by peripheral nervestimulation. Postoperative residual curari-zation
(PORC) remains a problem in postanesthesia care, producing potentially
injurious airway and respiratory function compromise. Reversal of neuromuscular
blocking agents is warranted, as is the use of intermediate acting
neuromuscular blocking agents instead of longer acting drugs.
Related Topics