Chapter: Medical Surgical Nursing: Assessment of Respiratory Function
Physical Assessment of the Upper Respiratory Structures
PHYSICAL ASSESSMENT OF THE UPPER RESPIRATORY STRUCTURES
For
a routine examination of the upper airway, only a simple light source, such as
a penlight, is necessary. A more thorough exami-nation requires the use of a
nasal speculum.
Nose and Sinuses
The
nurse inspects the external nose for lesions, asymmetry, or inflammation and
then asks the patient to tilt the head backward. Gently pushing the tip of the
nose upward, the nurse examines the internal structures of the nose, inspecting
the mucosa for color, swelling, exudate, or bleeding. The nasal mucosa is
nor-mally redder than the oral mucosa, but it may appear swollen and hyperemic
if the patient has a common cold. In allergic rhinitis, however, the mucosa
appears pale and swollen.
Next
the nurse inspects the septum for deviation, perforation, or bleeding. Most
people have a slight degree of septal deviation, but actual displacement of the
cartilage into either the right or left side of the nose may produce nasal
obstruction. Such deviation usually causes no symptoms.
While
the head is still tilted back, the nurse inspects the infe-rior and middle
turbinates. In chronic rhinitis, nasal polyps may develop between the inferior and
middle turbinates; they are dis-tinguished by their gray appearance. Unlike the
turbinates, they are gelatinous and freely movable.
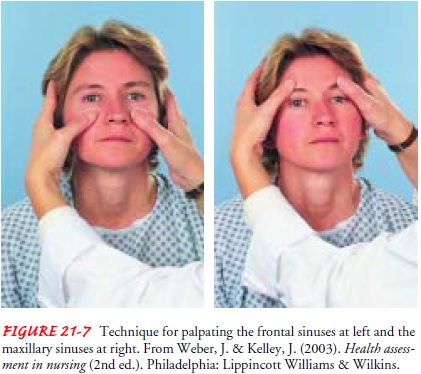
Next
the nurse may palpate the frontal and maxillary sinuses for tenderness (Fig.
21-7). Using the thumbs, the nurse applies gentle pressure in an upward fashion
at the supraorbital ridges (frontal sinuses) and in the cheek area adjacent to
the nose (max-illary sinuses). Tenderness in either area suggests inflammation.
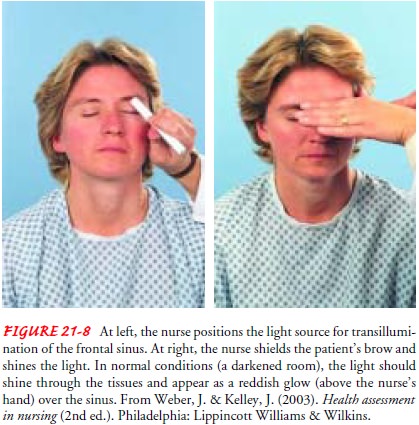
The frontal and maxillary sinuses can be inspected by transillu-mination
(passing a strong light through a bony area, such as the sinuses, to inspect
the cavity; Fig. 21-8). If the light fails to pen-etrate, the cavity is likely
to contain fluid or pus.
Pharynx and Mouth
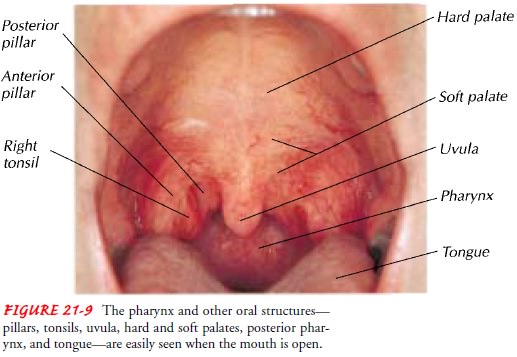
After
the nasal inspection, the nurse may assess the mouth and pharynx, instructing
the patient to open the mouth wide and take a deep breath. Usually this will
flatten the posterior tongue and briefly allow a full view of the anterior and
posterior pillars, ton-sils, uvula, and posterior pharynx (Fig. 21-9). The
nurse inspects these structures for color, symmetry, and evidence of exudate,
ul-ceration, or enlargement. If a tongue blade is needed to depress the tongue
to visualize the pharynx, it is pressed firmly beyond the midpoint of the tongue
to avoid a gagging response.
Trachea
Next
the position and mobility of the trachea are usually noted by direct palpation.
This is performed by placing the thumb and index finger of one hand on either
side of the trachea just above the sternal notch. The trachea is highly
sensitive, and palpating too firmly may trigger a coughing or gagging response.
The tra-chea is normally in the midline as it enters the thoracic inlet be-hind
the sternum, but it may be deviated by masses in the neck or mediastinum.
Pleural or pulmonary disorders, such as a pneu-mothorax, may also displace the
trachea.
Related Topics