Chapter: Medical Surgical Nursing: Assessment of Respiratory Function
Physical Assessment of the Lower Respiratory Structures and Breathing
PHYSICAL ASSESSMENT OF THE LOWER RESPIRATORY STRUCTURES AND
BREATHING
Thorax
Inspection of the thorax provides information about the muscu-loskeletal structure, the patient’s nutritional status, and the res-piratory system. The nurse observes the skin over the thorax for color and turgor and for evidence of loss of subcutaneous tissue. It is important to note asymmetry, if present. When findings are recorded or reported, anatomic landmarks are used as points of reference (Chart 21-7).
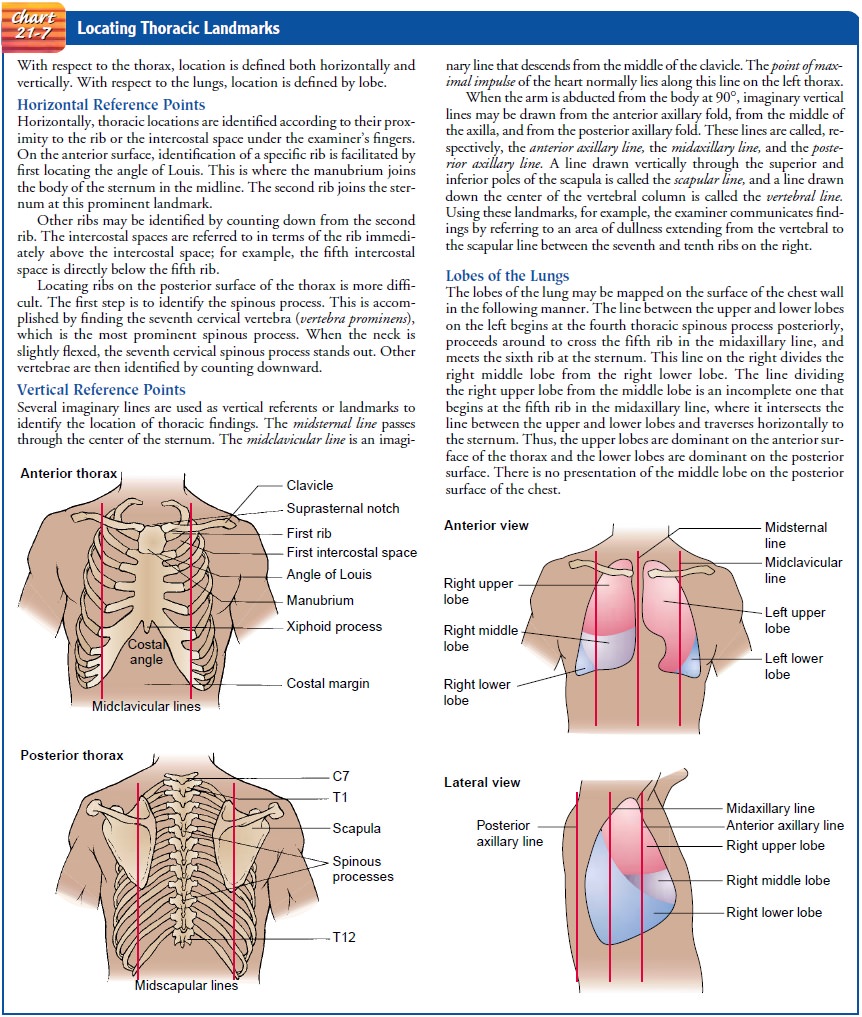
CHEST CONFIGURATION
Normally,
the ratio of the anteroposterior diameter to the lateral diameter is 1 2.
However, there are four main deformities of the chest associated with
respiratory disease that alter this relation-ship: barrel chest, funnel chest
(pectus excavatum), pigeon chest (pectus carinatum), and kyphoscoliosis.
Barrel Chest.
Barrel
chest occurs as a result of overinflation ofthe lungs. There is an increase in
the anteroposterior diameter of the thorax. In a patient with emphysema, the
ribs are more widely spaced and the intercostal spaces tend to bulge on
expiration. The appearance of the patient with advanced emphysema is thus quite
characteristic and often allows the observer to detect its presence easily,
even from a distance.
Funnel Chest (Pectus Excavatum).
Funnel chest occurs whenthere is a depression in the lower portion
of the sternum. This may compress the heart and great vessels, resulting in
murmurs. Funnel chest may occur with rickets or Marfan’s syndrome.
Pigeon Chest (Pectus Carinatum).
A pigeon chest occurs as a re-sult of displacement of the sternum.
There is an increase in the anteroposterior diameter. This may occur with
rickets, Marfan’s syndrome, or severe kyphoscoliosis.
Kyphoscoliosis.
A
kyphoscoliosis is characterized by elevation ofthe scapula and a corresponding
S-shaped spine. This deformity limits lung expansion within the thorax. It may
occur with os-teoporosis and other skeletal disorders that affect the thorax.
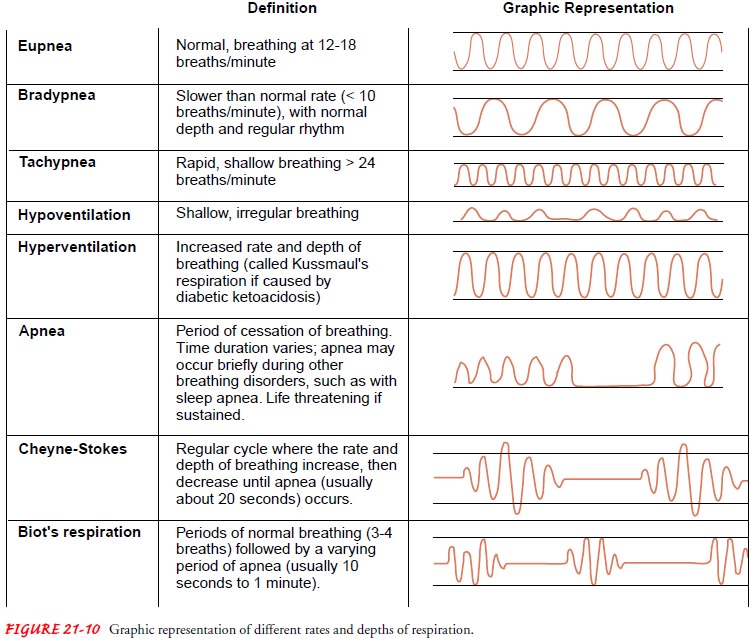
BREATHING PATTERNS AND RESPIRATORY RATES
Observing
the rate and depth of respiration is a simple but im-portant aspect of assessment.
The normal adult who is resting comfortably takes 12 to 18 breaths per minute.
Except for occa-sional sighs, respirations are regular in depth and rhythm.
This normal pattern is described as eupnea.
Bradypnea, also called slow breathing, is associated with in-creased intracranial pressure, brain injury, and drug overdose. Tachypnea, or rapid breathing, is commonly seen in patients with pneumonia, pulmonary edema, metabolic acidosis, septicemia, severe pain, and rib fracture. Shallow, irregular breathing is re-ferred to as hypoventilation.
An increase in depth of respirations is
called hyperpnea. An in-crease in both rate and depth that results in a lowered
arterial PCO2 level is referred to as hyperventilation. With rapid breath-ing,
inspiration and expiration are nearly equal in duration. Hy-perventilation that
is marked by an increase in rate and depth, associated with severe acidosis
of diabetic or renal origin, is called Kussmaul’s respiration.Apnea describes
varying periods of cessation of breathing. If sustained, apnea is
life-threatening. Cheyne-Stokes respiration is characterized by alternating
epi-sodes of apnea (cessation of breathing) and periods of deep breath-ing.
Deep respirations become increasingly shallow, followed by apnea that may last approximately 20
seconds. The cycle repeats after each apneic period. The duration of the period
of apnea may vary and may progressively lengthen; therefore, it is timed and
re-ported. Cheyne-Stokes respiration is usually associated with heart failure
and damage to the respiratory center (drug-induced, tumor, trauma).
Biot’s respirations, or cluster
breathing, are cycles of breaths that vary in depth and have varying periods of
apnea. Biot’s res-pirations are seen with some central nervous system
disorders.
Certain
patterns of respiration are characteristic of specific dis-ease states.
Respiratory rhythms and their deviation from normal are important observations
that the nurse reports and documents. The rate and depth of different patterns
of respiration are pre-sented in Figure 21-10.
In
thin people, it is quite normal to note a slight retraction of the intercostal
spaces during quiet breathing. Bulging during expiration implies obstruction of
expiratory airflow, as in em-physema. Marked retraction on inspiration,
particularly if asym-metric, implies blockage of a branch of the respiratory
tree. Asymmetric bulging of the intercostal spaces, on one side or the other,
is created by an increase in pressure within the hemitho-rax. This may be a
result of air trapped under pressure within the pleural cavity where it does
not normally appear (pneu-mothorax) or the pressure of fluid within the pleural
space (pleural effusion).
Thoracic Palpation
The nurse palpates the thorax for
tenderness, masses, lesions, res-piratory excursion, and vocal fremitus. If the
patient has reported an area of pain or if lesions are apparent, the nurse
performs di-rect palpation with the fingertips (for skin lesions and
subcuta-neous masses) or with the ball of the hand (for deeper masses or
generalized flank or rib discomfort).
RESPIRATORY EXCURSION
Respiratory
excursion is an estimation of thoracic expansion and may disclose significant
information about thoracic movement during breathing. The nurse assesses the
patient for range and symmetry of excursion. The patient is instructed to
inhale deeply while the movement of the nurse’s thumbs (placed along the costal
margin on the anterior chest wall) during inspiration and expiration is observed.
This movement is normally symmetric.
Posterior
assessment is performed by placing the thumbs adja-cent to the spinal column at
the level of the tenth rib (Fig. 21-11). The hands lightly grasp the lateral
rib cage. Sliding the thumbs medially about 2.5 cm (1 inch) raises a small
skinfold between the thumbs. The patient is instructed to take a full
inspiration and to exhale fully. The nurse observes for normal flattening of
the skin-fold and feels the symmetric movement of the thorax.

Decreased
chest excursion may be due to chronic fibrotic disease. Asymmetric excursion
may be due to splinting second-ary to pleurisy, fractured ribs, trauma, or
unilateral bronchial obstruction.
TACTILE FREMITUS
Sound
generated by the larynx travels distally along the bronchial tree to set the
chest wall in resonant motion. This is especially true of consonant sounds. The
detection of the resulting vibra-tion on the chest wall by touch is called
tactile fremitus.
Normal
fremitus is widely varied. It is influenced by the thick-ness of the chest
wall, especially if that thickness is muscular. However, the increase in
subcutaneous tissue associated with obe-sity may also affect fremitus.
Lower-pitched sounds travel better through the normal lung and produce greater
vibration of the chest wall. Thus, fremitus is more pronounced in men than in
women because of the deeper male voice. Normally, fremitus is most pronounced
where the large bronchi are closest to the chest wall and least palpable over
the distant lung fields. Therefore, it is most palpable in the upper thorax,
anteriorly and posteriorly.
The patient is asked to repeat
“ninety-nine” or “one, two, three,” or “eee, eee, eee” as the nurse’s hands move
down the pa-tient’s thorax. The vibrations are detected with the palmar
sur-faces of the fingers and hands, or the ulnar aspect of the extended hands,
on the thorax. The hand or hands are moved in sequence down the thorax.
Corresponding areas of the thorax are com-pared (Fig. 21-12). Bony areas are
not tested.
Air does not conduct sound well but a
solid substance such as tissue does, provided that it has elasticity and is not
compressed. Thus, an increase in solid tissue per unit volume of lung will
en-hance fremitus; an increase in air per unit volume of lung will im-pede
sound. Patients with emphysema, which results in the rupture of alveoli and
trapping of air, exhibit almost no tactile fremitus. A patient with
consolidation of a lobe of the lung from pneumonia will have increased tactile
fremitus over that lobe. Air in the pleural space will not conduct sound.
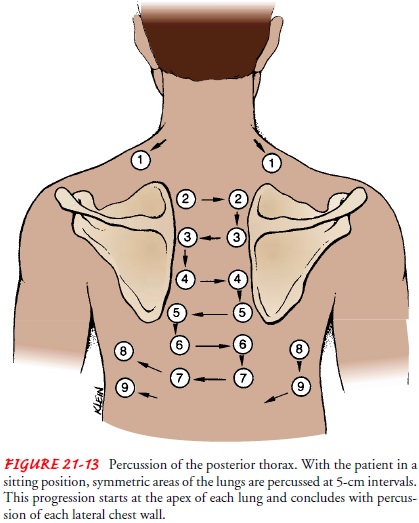
Thoracic Percussion
Percussion sets the chest wall and underlying structures in mo-tion, producing audible and tactile vibrations. The nurse uses percussion to determine whether underlying tissues are filled with air, fluid, or solid material. Percussion also is used to estimate the size and location of certain structures within the thorax (eg, di-aphragm, heart, liver).
Percussion
usually begins with the posterior thorax. Ideally, the patient is in a sitting
position with the head flexed forward and the arms crossed on the lap. This
position separates the scapulae widely and exposes more lung area for
assessment. The nurse percusses across each shoulder top, locating the 5-cm
width of resonance overlying the lung apices (Fig. 21-13). Then the nurse
proceeds down the posterior thorax, percussing symmetric areas at 5- to 6-cm
(2- to 2.5-inch) intervals. The middle finger is positioned parallel to the
ribs in the intercostal space; the fin-ger is placed firmly against the chest
wall before striking it with the middle finger of the opposite hand. Bony
structures (scapu-lae or ribs) are not percussed.
Percussion
over the anterior chest is performed with the pa-tient in an upright position
with shoulders arched backward and arms at the side. The nurse begins in the
supraclavicular area and proceeds downward, from one intercostal space to the
next. In the female patient, it may be necessary to displace the breasts for an
adequate examination. Dullness noted to the left of the ster-num between the
third and fifth intercostal spaces is a normal finding because it is the
location of the heart. Similarly, there is a normal span of liver dullness in
the right thorax from the fifth in-tercostal space to the right costal margin
at the midclavicular line.
The
anterior and lateral thorax is examined with the patient in a supine position.
If the patient cannot sit up, percussion of the pos-terior thorax is performed
with the patient positioned on the side.
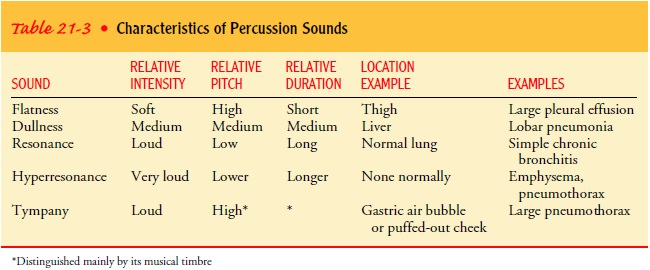
Dullness
over the lung occurs when air-filled lung tissue is re-placed by fluid or solid
tissue. Table 21-3 reviews percussion sounds and their characteristics.
DIAPHRAGMATIC EXCURSION
The normal resonance of the lung stops at the diaphragm. The position of the diaphragm is different during inspiration than during expiration.
To
assess the position and motion of the diaphragm, the nurse instructs the patient
to take a deep breath and hold it while the maximal descent of the diaphragm is
percussed. The point at which the percussion note at the midscapular line
changes from resonance to dullness is marked with a pen. The patient is then
instructed to exhale fully and hold it while the nurse again per-cusses
downward to the dullness of the diaphragm. This point is also marked. The
distance between the two markings indicates the range of motion of the
diaphragm.
Maximal
excursion of the diaphragm may be as much as 8 to 10 cm (3 to 4 inches) in
healthy, tall young men, but for most peo-ple it is usually 5 to 7 cm (2 to
2.75 inches). Normally, the di-aphragm is about 2 cm (0.75 inches) higher on
the right because of the position of the heart and the liver above and below
the left and right segments of the diaphragm, respectively. Decreased
diaphrag-matic excursion may occur with pleural effusion and emphysema. An
increase in intra-abdominal pressure, as in pregnancy or ascites, may account
for a diaphragm that is positioned high in the thorax.
Thoracic Auscultation
Auscultation
is useful in assessing the flow of air through the bronchial tree and in
evaluating the presence of fluid or solid ob-struction in the lung structures.
The nurse auscultates for normal breath sounds, adventitious sounds, and voice
sounds.
Examination
includes auscultation of the anterior, posterior, and lateral thorax and is
performed as follows. The nurse places the diaphragm of the stethoscope firmly
against the chest wall as the patient breathes slowly and deeply through the
mouth. Cor-responding areas of the chest are auscultated in a systematic
fash-ion from the apices to the bases and along midaxillary lines. The sequence
of auscultation and the positioning of the patient are similar to those used
for percussion. It often is necessary to listen to two full inspirations and
expirations at each anatomic location for valid interpretation of the sound
heard. Repeated deep breaths may result in symptoms of hyperventilation (eg,
light-headed-ness); this is avoided by having the patient rest and breathe
nor-mally periodically during the examination.
BREATH SOUNDS
Normal
breath sounds are distinguished by their location over a specific area of the
lung and are identified as vesicular, bron-chovesicular, and bronchial
(tubular) breath sounds (Table 21-4).
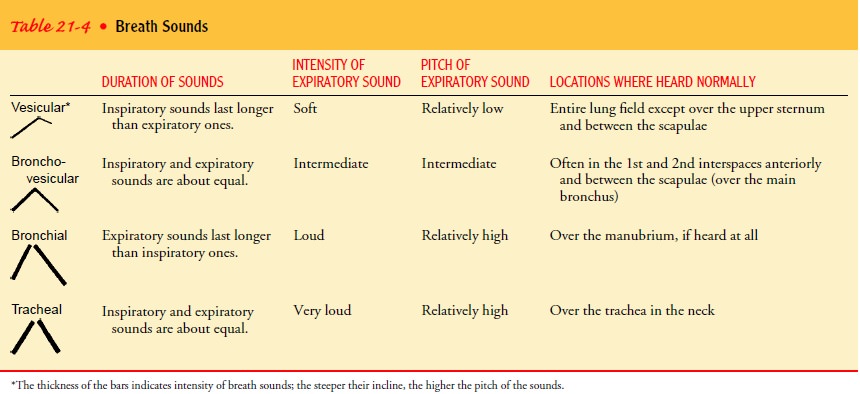
The
location, quality, and intensity of breath sounds are de-termined during
auscultation. When airflow is decreased by bron-chial obstruction (atelectasis)
or when fluid (pleural effusion) or tissue (obesity) separates the air passages
from the stethoscope, breath sounds are diminished or absent. For example, the
breath sounds of the patient with emphysema are faint or often com-pletely
inaudible. When heard, the expiratory phase is prolonged. Bronchial and
bronchovesicular sounds that are audible any-where except over the main
bronchus in the lungs signify pathol-ogy, usually indicating consolidation in
the lung (eg, pneumonia, heart failure). This finding requires further
evaluation.
ADVENTITIOUS SOUNDS
An abnormal condition that affects the
bronchial tree and alve-oli may produce adventitious (additional) sounds.
Adventitious sounds are divided into two categories: discrete, noncontinuous
sounds (crackles) and continuous musical sounds (wheezes). The duration of the
sound is the important distinction to make in identifying the sound as
noncontinuous or continuous. Pleural friction rubs are specific examples of
crackles (Table 21-5).
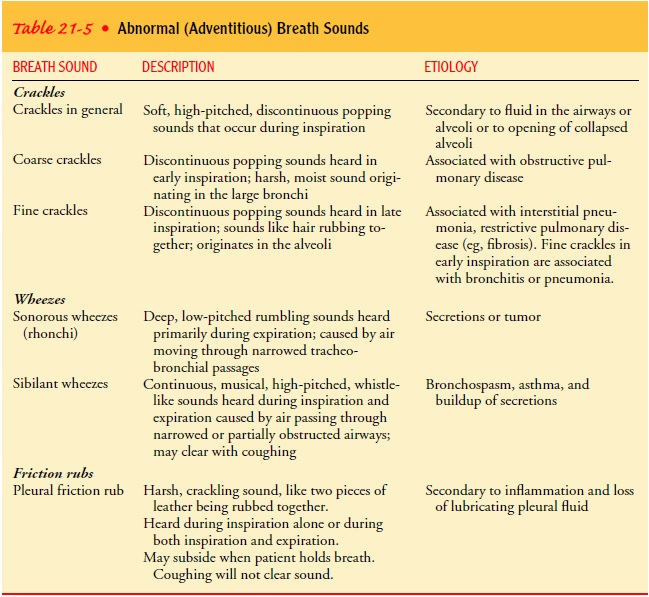
Crackles
(formerly referred to
as rales) are discrete, noncon-tinuous sounds that result from delayed
reopening of deflated air-ways. Crackles may or may not be cleared by coughing.
Crackles reflect underlying inflammation or congestion and are often pre-sent
in such conditions as pneumonia, bronchitis, heart failure, bronchiectasis, and
pulmonary fibrosis.
Friction rubs result from inflammation
of the pleural surfaces that induces a crackling, grating sound usually heard
in inspira-tion and expiration. The sound can be enhanced by applying pressure
to the chest wall with the diaphragm of the stethoscope. The sound is imitated
by rubbing the thumb and index finger to-gether near the ear. A friction rub is
best heard over the lower lat-eral anterior surface of the thorax.
Wheezes
are associated with
bronchial wall oscillation andchanges in airway diameter. Wheezes are commonly
heard in pa-tients with asthma, chronic bronchitis, and bronchiectasis.
VOICE SOUNDS
The
sound heard through the stethoscope as the patient speaks is known as vocal
resonance. The vibrations produced in the larynx are transmitted to the chest
wall as they pass through the bronchi and alveolar tissue. During the process,
the sounds are diminished in intensity and altered so that syllables are not
distin-guishable. Voice sounds are usually assessed by having the patient
repeat “ninety-nine” or “eee” while the nurse listens with the stethoscope in
corresponding areas of the chest from the apices to the bases.
Bronchophony describes vocal resonance
that is more intense and clearer than normal. Egophony describes voice sounds
that are distorted. It is best appreciated by having the patient repeat the
letter E. The distortion produced by consolidation transforms the sound into a
clearly heard A rather than E. Bronchophony and egophony have precisely the
same significance as bronchial breathing with an increase in tactile fremitus.
When an abnor-mality is detected, it should be evident using more than one
as-sessment method. A change in tactile fremitus is more subtle and can be
missed, but bronchial breathing and bronchophony can be noted loudly and
clearly.
Whispered pectoriloquy is a very subtle
finding, heard only in the presence of rather dense consolidation of the lungs.
Trans-mission of high-frequency components of sound is so enhanced by the
consolidated tissue that even whispered words are heard, a circumstance not
noted in normal physiology. The significance is the same as that of
bronchophony.
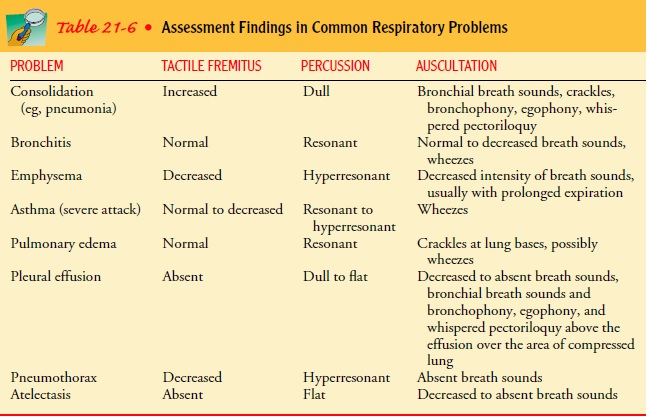
The
physical findings for the most common respiratory dis-eases are summarized in
Table 21-6.
Related Topics