Chapter: Essentials of Psychiatry: Personality Disorders
Personality Disorder
Personality
Disorder
Definition
A
personality disorder is defined in DSM-IV-TR as “an enduring pattern of inner
experience and behavior that deviates markedly from the expectations of the
individual’s culture, is pervasive and inflexible, has an onset in adolescence
or early adulthood, is stable over time, and leads to distress or impairment”.
The DSM-IV-TR general diagnostic criteria for a personality disorder are
provided below.
Personality disorder is the only class of mental disorders in DSM-IV-TR for which an explicit definition and criterion set are provided. A general definition and criterion set can be useful to psychiatrists because the most common personality disorder di-agnosis in clinical practice is often the diagnosis “not otherwise specified” (NOS) (Clark et al., 1995). Psychiatrists provide the NOS diagnosis when they determine that a personality disorderis present but the symptomatology fails to meet the criterion set for one of the 10 specific personality disorders. A general defini-tion of what is meant by a personality disorder is therefore helpful when determining whether the NOS diagnosis should in fact be provided. Points worth emphasizing with respect to the general criterion set are presented in the following discussion of the as-sessment, differential diagnosis, epidemiology and course of per-sonality disorders
Etiology and Pathophysiology
A primary
purpose of a diagnosis is to lead to scientific knowledge concerning the
etiology for a patient’s condition and the identi-fication of a specific
pathology for which a particular treatment (e.g., medication) would ameliorate
the condition. However, many of the mental disorders in DSM-IV-TR, including
the personality disorders, may not in fact have single etiologies or even
specific pathologies. The DSM-IV-TR personality disorders might be, for the
most part, constellations of maladaptive personality traits that are the result
of multiple genetic dispositions interacting with a variety of detrimental
environmental experiences. The DSM-IV-TR personality disorder diagnoses do
provide the clinician with a substantial amount of important information
concerning the etiology and pathology for a patient’s particular personal-ity
syndrome, but there are likely to be alternative pathways to the development of
maladaptive personality traits and alterna-tive neurophysiological,
cognitive–behavioral, interpersonal and psychodynamic models for their
pathology (Livesley, 2001).
Assessment and Differential Diagnosis
Since
1980, the multiaxial system appears to have been successful in encouraging
psychiatrists no longer to make arbitrary distinc-tions between personality
disorders and other mental disorders. Ironically, however, the placement of the
personality disorders on a separate axis may have also contributed to the
development of false assumptions and misleading expectations concerning the
distinctions between personality disorders and other mental dis-orders with
respect to etiology, pathology, or treatment. It has been difficult to provide
a brief list of specific diagnostic criteria for the broad and complex behavior
patterns that constitute a per-sonality disorder. The only personality disorder
to be diagnosed reliably in general clinical practice has been antisocial and
the validity of this diagnosis has been questioned precisely because of its
emphasis on overt and behaviorally specific acts of crimi-nality,
irresponsibility and delinquency.
There are
assessment instruments, however, that will help psychiatrists obtain more
reliable and valid personality disor-der diagnoses. Semi-structured interviews
will obtain reliable diagnoses of personality disorders and are therefore the
preferred method for the assessment of personality disorders in clinical settings.
Semi-structured interviews provide a researched set of required and recommended
interview queries and observations to assess each of the personality disorder
diagnostic criteria. Psy-chiatrists can find the administration of a
semi-structured inter-view to be constraining but a major strength of
semi-structured interviews is their assurance through an explicit structure
that each relevant diagnostic criterion has in fact been systematically
assessed. Idiosyncratic and subjective interviewing techniques are much more
likely to result in gender- and culturally-biased assessments relative to
unstructured clinical interviews. The manuals that accompany a semi-structured
interview also pro-vide useful information for understanding the rationale of
each diagnostic criterion, for interpreting vague or inconsistent
symp-tomatology, and for resolving diagnostic ambiguities. There are currently
five semi-structured interviews for the assessment of the DSM-IV-TR (American
Psychiatric Association, 2000) per-sonality disorder diagnostic criteria: 1)
Diagnostic Interview for Personality Disorders (Zanarini et al., 1995); 2) International Personality Disorder Examination
(Loranger, 1999); 3) Personal-ity Disorder Interview-IV (Widiger et al., 1995); 4) Structured Clinical
Interview for DSM-IV-TR Axis II PersonalityDisorders (First et al., 1997); and 5) Structured
Interview for DSM-IV-TR Personality Disorders (Pfohl et al., 1997). The par-ticular advantages and disadvantages of each
particular interview have been discussed extensively (Widiger and Coker, 2002).
The
administration of an entire personality disorder semi-structured interview can
take 2 hours, an amount of time that is impractical for routine clinical
practice. However, this time can be reduced substantially by first
administering a self-report questionnaire that screens for the presence of the
DSM-IV-TR personality disorders (Widiger and Coker, 2002). A psychiatrist can
then confine the interview to the few personality disorders that the
self-report inventory suggested would be present. Self-report inventories are
useful in ensuring that all of the personality disorders were systematically
considered and in alerting the clini-cian to the presence of maladaptive
personality traits that might otherwise have been missed. There are a number of
alternative self-report inventories that can be used and the advantages and
disadvantages of each of them have been discussed extensively (Widiger and
Coker, 2002).
Gender
and cultural biases are one potential source of inaccurate personality disorder
diagnosis that are worth noting in particular. One of the general diagnostic
criteria for personality disorder is that the personality trait must deviate
markedly from the expectations of a person’s culture (see DSM-IV-TR general
diagnostic criteria for personality disorders). The purpose of this cultural
deviation requirement is to compel clinicians to consider the cultural
background of the patient. A behavior pattern that appears to be aberrant from
the perspective of one’s own culture (e.g., submissiveness or emotionality)
could be quite normative and adaptive within another culture. The cultural
expectations or norms of the psychiatrist might not be relevant or applicable
to a patient from a different cultural background. However, one should not
infer from this requirement that a personality disorder is primarily or simply
a deviation from a cultural norm. Devia-tion from the expectations of one’s
culture is not necessarily mal-adaptive, nor is conformity to one’s culture
necessarily healthy. Many of the personality disorders may even represent (in
part) extreme or excessive variants of behavior patterns that are val-ued or
encouraged within a particular culture. For example, it is usually adaptive to
be confident but not to be arrogant, to be agreeable but not to be submissive,
or to be conscientious but not to be perfectionistic.
Epidemiology and Comorbidity
Virtually
all patients must have had a characteristic manner of thinking, feeling,
behaving and relating to others prior to the onset of an Axis I disorder that
could have an important impact on the course and treatment of the respective
mental disorder and many of these persons would be diagnosed with a DSM-IV-TR
personality. Estimates of the prevalence of personality disor-der within
clinical settings is typically above 50%. As many as 60% of inpatients within
some clinical settings would be diag-nosed with borderline personality disorder
and as many as 50% of inmates within a correctional setting could be diagnosed
with antisocial personality disorder. Although the comorbid presence of a
personality disorder is likely to have an important impact on the course and
treatment of an Axis I disorder the prevalence of personality disorder is
generally underestimated in clini-cal practice due in part to the failure to
provide systematic or comprehensive assessments of personality disorder
symptom-atology and perhaps as well to the lack of funding for the treat-ment of
personality disorders.
Approximately
10 to 15% of the general population would be diagnosed with one of the 10
DSM-IV-TR personality disor-ders, excluding PDNOS. However the studies of
community pop-ulations have important limitations that qualify their results.
For example, many of the studies sampled persons who would prob-ably have less
personality disorder pathology than a randomly selected sample (e.g., some
studies have sampled persons without any history of Axis I psychopathology) and
the studies have used either the DSM-III (American Psychiatric Association,
1980) or DSM-III-R (American Psychiatric Association, 1987) criterion sets
rather than DSM-IV-TR (American Psychiatric Association, 2000). Nevertheless,
the prevalence estimates are generally close to those provided in DSM-IV-TR.
There is
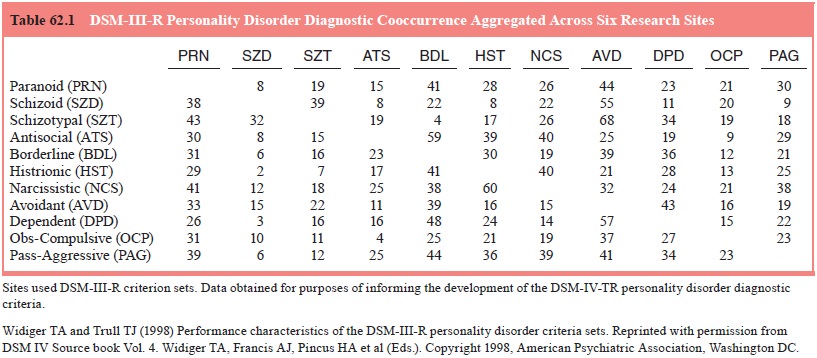
also considerable personality disorder diagnostic cooccurrence (Table 62.1).
Patients who meet the DSM-IV diag-nostic criteria for one personality disorder
are likely to meet the diagnostic criteria for another DSM-IV instructs
psychiatrists that all diagnoses should be recorded because it can be
impor-tant to consider (for example) the presence of antisocial traits in
someone with a borderline personality disorder or the pres-ence of paranoid
traits in someone with a dependent personality disorder. However, the extent of
diagnostic cooccurrence is at times so extensive that most researchers prefer a
more dimen-sional description of personality. Diagnostic categories provide
clear, vivid descriptions of discrete personality types but the per-sonality
structure of actual patients might be more accurately described by a
constellation of maladaptive personality traits.
Alternative
dimensional models of personality disorder are being developed. One such model,
based on a theory of tem-perament and character, consists of seven dimensions.
Cloninger (2000) proposes that there are four temperaments (reward depen-dence,
harm avoidance, novelty seeking and persistence), each governed by a particular
neurotransmitter system, and three character dimensions (self-directedness,
cooperativeness and self-transcendence). The presence of a personality disorder
is said to be determined primarily by the four temperaments and
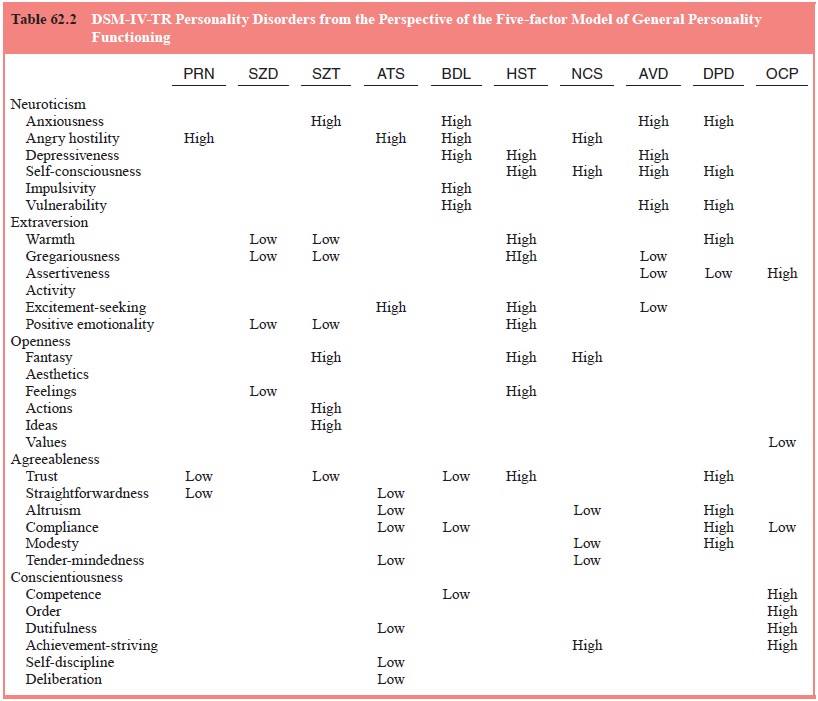
Table
62.2 provides a description of the DSM-IV-TR per-sonality disorders in terms of
this five-factor model. For example, the schizoid personality disorder may
represent an extreme vari-ant of introversion, avoidant may represent extreme
neuroticism and introversion, and antisocial personality disorder an extreme
variant of antagonism and undependability. Advantages of under-standing
personality disorders in terms of this dimensional model are the provision of
more specific descriptions of individual patients (including adaptive as well
as maladaptive personality functioning) and the avoidance of arbitrary
categorical distinc-tions. An additional factor is the ability to bring to bear
on an understanding of personality disorders the extensive amount of research
on the heritability, temperament, development and course of general personality
functioning.
Course
Personality
disorders must be evident since adolescence or young adulthood and have been
relatively chronic and stable throughout adult life (see DSM-IV-TR criteria for
personality disorders). The World Health Organization’s (WHO) International Classifi cation of Diseases, 10th Revision (ICD-10, World Health Organization, 1992) does recognize the existence of
personality change second- ary to catastrophic experiences and to brain injury
or disease, but only the latter is included within DSM-IV-TR (American
Psychiatric Association, 2000). A 75-year-old man can be diag-nosed with a
DSM-IV-TR dependent personality disorder but the symptoms must have been
present throughout the duration of his adulthood (e.g., since the age of 18
years) unless the dependent behavior was a direct, explicit expression of a
neurochemical dis-ease or lesion.
The
requirement that a personality disorder be evident since late adolescence and
be relatively chronic thereafter has been a traditional means with which to
distinguish a personal-ity disorder from an Axis I disorder. Mood, anxiety,
psychotic, sexual and other mental disorders have traditionally been
con-ceptualized as conditions that arise at some point during a person’s life
and that are relatively limited or circumscribed in their expression and
duration. Personality disorders, in contrast, are conditions that are evident
as early as late adolescence (and in some instances prior to that time), are
evident in everyday functioning, and are stable throughout adulthood. However,
the consistency of this distinction across disorders in the clas-sification has
been decreasing with each edition of the DSM, as early-onset and chronic
variants of Axis I disorders are being added to the diagnostic manual (e.g.,
early-onset dysthy-mia and generalized social phobia). Some researchers have in
fact suggested abandoning the concept of personality disorders and replacing
them with early-onset and chronic variants of existing Axis I disorders. For
example, avoidant personality disorder could become generalized social phobia,
obsessive– compulsive personality disorder could become an early-onset variant
of obsessive–compulsive anxiety disorder, and bor-derline personality disorder
could become an early-onset and chronic mood dyscontrol.
Treatment
One of
the mistaken assumptions or expectations of Axis II is that personality
disorders are untreatable. In fact, maladaptive personality traits are often
the focus of clinical attention. Person-ality disorders are among the more
difficult of mental disorders to treat as they involve entrenched behavior
patterns, some of which will be integral to a patient’s self-image.
Nevertheless, there is compelling empirical support to indicate that meaningful
respon-sivity to psychosocial and pharmacologic treatment does occur. Treatment
of a personality disorder is unlikely to result in the development of a fully
healthy or ideal personality structure, but clinically and socially meaningful
change to personality struc-ture and functioning does occur. In fact, given the
considerable social, occupational, medical and other costs that are engendered
by such personality disorders as the antisocial and borderline, even marginal
reductions in symptomatology can represent quite significant and meaningful
public health care, social and clinical benefits.
DSM-IV-TR
includes 10 individual personality disorder diagnoses that are organized into
three clusters: 1) paranoid, schizoid and schizotypal (placed within an
odd–eccentric clus-ter); 2) antisocial, borderline, histrionic and narcissistic
(dra-matic–emotional–erratic cluster); and 3) avoidant, dependent and
obsessive–compulsive (anxious–fearful cluster) (American Psy-chiatric
Association, 2000). Each of these personality disorders, along with the two
that are included in the appendix to DSM-IV-TR for disorders needing further
study (i.e., passive–aggressive and depressive), will be discussed in turn.
Related Topics