Chapter: Essentials of Psychiatry: Personality Disorders
Borderline Personality Disorder
Borderline
Personality Disorder
Definition
Borderline
personality disorder (BPD) is a pervasive pattern of impulsivity and
instability in interpersonal relationships and self-image (American Psychiatric
Association, 2000). A broad domain of general personality functioning is
neuroticism or emotional instability. characterized by facets of angry
hostility, anxiousness, depressiveness, impulsivity and vulnerability; BPD is
essentially the most extreme and highly maladaptive variant of emotional
instability. This disorder is indicated by the presence of five or more of the
nine diagnostic criteria presented in the DSM-IV-TR criteria for BPD.
Etiology and Pathology
There are studies to indicate that BPD may breed true but most research has suggested an association with mood and impulse dyscontrol disorders. There is also consistent empirical support for a childhood history of physical and/or sexual abuse, as well as parental conflict, loss and neglect. It appears that past traumatic events are important in many if not most cases of BPD, contrib-uting to the overlap and association with post traumatic stress and dissociative disorders but the nature and age at which these events have occurred will vary. BPD may involve the interaction of a genetic disposition towards dyscontrol of mood and impulses (i.e., emotionally unstable temperament), with a cumulative and evolving series of intensely pathogenic relationships.
There are
numerous theories regarding the pathogenic mechanisms of BPD, most concern
issues regarding abandon-ment, separation, and/or exploitative abuse, which is
one of the reasons that frantic efforts to avoid abandonment is the first item
in the DSM-IV-TR diagnostic criterion set. Persons with BPD have quite intense,
disturbed, and/or abusive relationships with the significant persons of their
past, including their parents, contributing to the development of malevolent
perceptions and expectations of others. These expectations, along with an impair-ment
in the ability to regulate affect and impulses may contribute to the
perpetuation of intense, angry and unstable relationships. Neurochemical
dysregulation is evident in persons with BPD but it is unclear whether this
dysregulation is a result, cause, or cor-relate of prior interpersonal traumas.
Assessment and Differential Diagnosis
All of
the DSM-IV assessment instruments described earlier include the assessment of
BPD. However, an instrument that is focused on the assessment of BPD is the
Diagnostic Interview for Borderlines-Revised (DIB-R; Zanarini et al., 1989). The DIB-R provides a more
thorough assessment of components of BPD (e.g., impulsivity, affective
dysregulation and cognitive–perceptual aberrations) than is provided by more
general DSM-IV-TR per-sonality disorder semi-structured interviews, but
psychiatrists might find it impractical to devote up to 2 hours to assess one
particular personality disorder, especially when it is likely that other
maladaptive personality traits not covered by the DIB-R are also likely to be
present.
Most
persons with BPD develop mood disorders and it is at times difficult to
differentiate BPD from a mood disorder if the assessment is confined to the
current symptomatology. A diagnosis of BPD requires that the borderline
symptomatology be evident since adolescence, which should differentiate BPD
from a mood disorder in all cases other than a chronic mood disorder. If there
is a chronic mood disorder, then the additional features of transient,
stress-related paranoid ideation, dissociative experi-ences, impulsivity and
anger dyscontrol that are evident in BPD should be emphasized in the diagnosis
(Gunderson, 2001).
Epidemiology and Comorbidity
Approximately
1 to 2% of the general population would meet the DSM-IV criteria for BPD. BPD
is the most prevalent personality disorder within maximum clinical settings.
Approximately 15% of all inpatients (51% of inpatients with a personality
disorder) and 8% of all outpatients (27% of outpatients with a personality disorder)
have a borderline personality disorder. Approximately 75% of persons with BPD
will be female. Persons with BPD meet DSM-IV-TR criteria for at least one Axis
I disorder. The range of potential Axis I comorbid psychopathology includes
mood (major depressive disorder), anxiety (post traumatic stress dis-order),
eating (bulimia nervosa), substance (alcohol dependence), dissociative
(dissociative identity disorder), and psychotic (brief psychotic) disorders
(Gunderson, 2001). Persons with BPD also meet DSM-IV-TR criteria for at least
one other personality dis-order, particularly histrionic, dependent,
antisocial, schizotypal, or passive–aggressive. Researchers and clinicians have
at times responded to this extensive cooccurrence by imposing a diag-nostic hierarchy
whereby other disorders are not diagnosed in the presence of BPD because BPD is
generally the most severely dysfunctional disorder (Gunderson et al., 2000). A potential limitation of
this approach is that it resolves the complexity of personality by largely
ignoring it. This approach may fail to rec-ognize the presence of maladaptive
personality traits that could be important for understanding a patient’s
dysfunctions and for developing an optimal treatment plan.
Course
As
children, persons with BPD are likely to have been emotionally unstable,
impulsive and angry or hostile. Their chaotic impulsiv-ity and intense
affectivity may contribute to involvement within rebellious groups as a child
or adolescent, along with a variety of Axis I disorders, including eating,
substance use and mood dis-orders. BPD is often diagnosed in children and
adolescents but considerable caution should be used when doing so as some of
the symptoms of BPD (e.g., identity disturbance and unstable rela-tionships)
could be confused with a normal adolescent rebellion or identity crisis. As
adults, persons with BPD may require numerous hospitalizations due to their
affect and impulse dyscontrol, psy-chotic-like and dissociative symptomatology
and risk of suicide. Minor problems quickly become crises as the intensity of
affect and impulsivity result in disastrous decisions. They are at a high risk
for developing depressive, substance-related, bulimic and post traumatic stress
disorders. The potential for suicide increases with comorbid mood and
substance-related disorder. Approximately 3 to 10% commit suicide by the age of
30 years. Relationships tend to be very unstable and explosive and employment
history is poor. Affectivity and impulsivity, however, may begin to diminish as
the person reaches the age of 30 years, or earlier if the person becomes
involved with a supportive and patient sexual partner. Some, however, may
obtain stability by abandoning the effort to obtain a relationship, opting
instead for a lonelier but less volatile life. The mellowing of the
symptomatology, however, can be eas-ily disrupted by the occurrence of a severe
stressor (e.g., divorce by or death of a significant other) that results in a
brief psychotic, dissociative, or mood disorder episode.
Treatment
Persons
with BPD often develop intense, dependent, hostile, un-stable and manipulative
relationships with their therapists as they do with their peers. At one time
they might be very compliant, responsive and even idealizing, but later angry,
accusatory and devaluing. Their tendency to be manipulatively as well as
impul-sively self-destructive is often very stressful and difficult to treat
(Stone, 2000).
Persons
with BPD are often highly motivated for treatment. Psychotherapeutic approaches
tend to be both supportive and ex-ploratory. Therapists should provide a safe,
secure environment in which anger can be expressed and actively addressed
without destroying the therapeutic relationship. The historical roots of
current bitterness, anger and depression within past familial rela-tionships
should eventually be explored, but immediate, current issues and conflicts must
also be explicitly addressed. Suicidal behavior should be confronted and
contained, by hospitalization when necessary. Patients with BPD can be very
difficult to treat because the focus of the patient’s love and wrath will often
be shifted toward the therapist, and the treatment may itself become the
patient’s latest unstable, intense relationship. Immediate and ongoing
consultation with colleagues is often necessary, as it is not unusual for
therapists to be unaware of the extent to which they are developing or
expressing feelings of anger, attraction, annoyance, or intolerance toward
their borderline patient.
A
particular form of cognitive–behavioral therapy, dialecti-cal behavior therapy,
has been shown empirically to be effective in the treatment of BPD (Linehan,
2000). Part of the strategy entailskeeping patients focused initially on the
priorities of reducing sui-cidal threats and gestures, behaviors that can
disrupt or resist treat-ment, and behaviors that affect the immediate quality
of life (e.g., bulimia, substance abuse, or unemployment). Once these goals are
achieved, the focus can then shift to a mastery of new coping skills,
management of reactions to stress and other individualized goals. Individual
therapy is augmented by skills-training groups that may be highly structured
(e.g., comparable to a classroom format). Patients are taught skills for coping
with identity diffu-sion, tolerating distress, improving interpersonal
relationships, controlling emotions and resolving interpersonal crises.
Patients are given homework assignments to practice these skills that are
further addressed and reinforced within individual sessions. Neg-ative affect
is also addressed through a mindful meditation that contributes to an
acceptance and tolerance of past abusive experi-ences and current stress. The
dialectical component of the therapy is that “the dialectical therapist helps
the patient achieve synthesis of oppositions, rather than focusing on verifying
either side of an oppositional argument”. An illustrative list of dialectical
strategies is presented in Table 62.3.
DBT,
however, also includes more general principles of treatment that are important
to emphasize in all forms of therapy for BPD (Linehan, 1993; Stone, 1993,
2000), some of which are presented in Table 62.4. For example, exasperated
therapists may unjustly experience and even accuse borderline patients of being
unmotivated or unwilling to work. It is important to appreciate that they do
want to improve and are doing the best that they can. One should not make the
therapy personal, but instead identify the sources of the inhibition or
interference to their motivation to change. One should take seriously their
complaints that their lives are indeed unbearable but not absolve them of their
responsibility to solve their own problems. They are unlikely to change simply
through a passive reception of insight, nurturance, support and

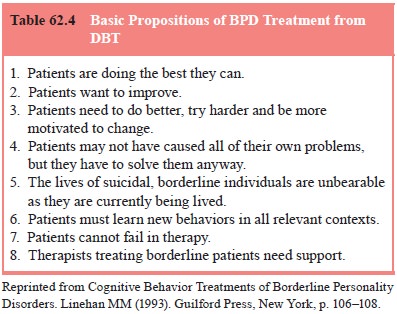
medication.
They will need to work actively on changing their lives. Therapists will often
be tempted to rescue their patients, particularly when they are within a
crisis. However, it is precisely at such times that there will be the best
opportunity to develop and learn new coping strategies. Failures can occur, and
it is a fail-ure of the therapy that should be conscientiously and effectively
addressed by the therapist. Finally, therapists need honestly to recognize
their own limitations. All therapists have their own flaws and limits and
patients with BPD invariably strain and overwhelm these limits. Therapists need
to be open and recep-tive to outside support, advice and criticism.
Pharmacologic
treatment of patients with BPD is varied, as it depends primarily on the
predominant Axis I symptomatology. Persons with BPD can display a wide variety
of Axis I symptoms, including anxiety, depression, hallucinations, delusions
and dis-sociations. It is important in their pharmacologic treatment not to be
unduly influenced by transient symptoms or by symptoms that are readily
addressed through exploratory or supportive tech-niques. On the other hand, it
is equally important to be flexible in the use of medications and not to be
unduly resistant to their use. Relying solely upon one’s own psychotherapeutic
skills can be unnecessary and even irresponsible.
Related Topics