Chapter: Paediatrics: Emergency and high dependency care
Paediatrics: Fluid and electrolytes: dehydration
Fluid and electrolytes: dehydration
Dehydration can lead to shock,
severe metabolic acidosis, and death, par-ticularly in infants. Its severity
can be assessed using change in weight or the following physical signs.
Mild dehydration (0–5%)
·
Weight loss: 5% in infants and 3% in children.
·
Skin turgor: may be decreased.
·
Mucous membranes: dry.
·
Urine: may be low.
·
Heart rate: increased.
·
Blood pressure: normal.
·
Perfusion: normal.
·
Skin colour: pale.
·
Consciousness: irritable.
Moderate dehydration (5–10%)
·
Weight loss: 10% in infants and 6% in children.
·
Skin turgor: decreased.
·
Mucous membranes: very dry.
·
Urine: oliguric.
·
Heart rate: increased.
·
BP: may be normal.
·
Perfusion: prolonged capillary refill
(capillary refill time (CRT) > 2s).
·
Skin colour: grey.
·
Consciousness: lethargic.
Severe dehydration (10–15%)
·
Weight loss: 15% in infants and 9% in children.
·
Skin turgor: poor with tenting.
·
Mucous membranes: parched.
·
Urine: anuric.
·
Heart rate: increased.
·
Blood pressure: decreased.
·
Perfusion: prolonged CRT.
·
Skin colour: mottled; blue or white.
·
Consciousness: comatose.
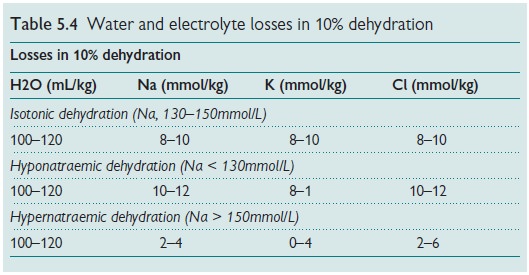
After you have assessed the degree
of dehydration in your patient, two problems need to be addressed—water and
electrolyte losses. In practice, our treatment is aimed at correcting both the
water and electrolyte losses (Table 5.4).
Isotonic and hyponatraemic dehydration
·First assess the degree of
dehydration (use weight change and signs).
·Calculate the fluid deficit.
·FBC with differential.
·Serum electrolytes (Na, K, Ca)
with urea, creatinine, and glucose.
Emergency treatment is directed
toward restoring any compromise in the circulation. (See shock: use 20mL/kg IV
normal saline). Monitoring should include: vital signs, losses (urine output,
stool, vomitus, NG), daily weights, and blood tests. After the initial phase,
fluid administration should be calculated to correct deficits over 48hr.
Overall, take into account the deficit, maintenance requirements, and any
ongoing losses:
Hourly rate = (24hr maintenance +
deficit – resuscitation fluids)/24
Hypernatraemic dehydration
·Water losses exceed sodium loss.
·Cerebral oedema is a risk during
rehydration, so correction of the deficit should be achieved slowly and evenly,
over 48hr.
·Emergency treatment of shock is
treated with 10–20mL/kg IV saline. Thereafter, calculate the deficit and
restore patient’s needs.
·Monitor as above, with at least
8-hourly electrolyte studies.
·Use 0.9% saline so that sodium
correction occurs slowly.
Seizures and cerebral oedema may
complicate the rehydration phase of hypernatraemic dehydration. If these occur,
treat symptomatically and refer to an intensive care unit. There may be a
number of causes of these problems—your initial role in this emergency is to do
the ABCs. Further investigations and CT scan may be needed.
Related Topics