Chapter: Paediatrics: Practical procedures
Paediatrics: Endotracheal intubation
Endotracheal intubation
Indications
This procedure is used as part of
advanced resuscitation and care.
Equipment
•
Appropriately-sized laryngoscope: neonatal laryngoscopes are
straight; blade size starts at 0
(7.5cm long) for use in preterm infants. Use size 1 (10cm) in term infants. In older
children use curved blade laryngoscopes (Macintosh).
•
ETT size: 2–2.5mm (internal diameter) in
infant <1000g; 3mm when 1000–3000g;
3.5mm when >3000g. The appropriate size then increases as child size
increases up to male adult size of 8–9mm. Cole (shouldered) ETTs are suitable
for oral intubation in newborns. Straight (non-shouldered) tubes can be used
for oral or nasal intubation.
•
Appropriately-sized
introducer if required.
•
Lubricating
jelly if attempting nasal intubation.
•
Magill
forceps if attempting nasal intubation.
•
Suction
catheter and tubing connected to suction source.
•
Appropriate
ETT connection adaptors, tubing, and O2 source.
•
Fixation
device and tape.
Procedure
•
Oral
intubation is preferred during short-term intubation or during resuscitation.
Nasal intubation has advantages if ventilation is prolonged.
•
Check
laryngoscope light, O2 supply, and suction.
•
Connect
child to pulse oximeter and cardiac monitor.
•
Sedation
or anaesthesia should be given prior to elective intubation.
•
Pre-oxygenate
the child by hyperventilation with 85% O2 for 15–30s prior to
elective intubation.
•
Place
the child in the supine position with the head in the neutral position and the
neck slightly extended.
•
Stand
immediately behind the child’s head.
•
If nasal
intubation is being performed, a prelubricated ETT should be passed into one
nostril as far as the nasopharynx prior to insertion of laryngoscope. If the
ETT will not pass easily, do not try force, as this may lead to penetration of
the cribriform plate.
•
Open
the mouth and use suction to clear airway secretions.
•
Holding
the laryngoscope in the left hand, initially insert the blade to the right side
of the mouth and advance to the base of the tongue.
•
Once
inserted move the laryngoscope blade into the centre of the mouth, thereby
pushing the tongue to the left.
•
Advance
the blade further until epiglottis is seen and then insert blade tip into the
valleculla (space between base of tongue and epiglottis).
•
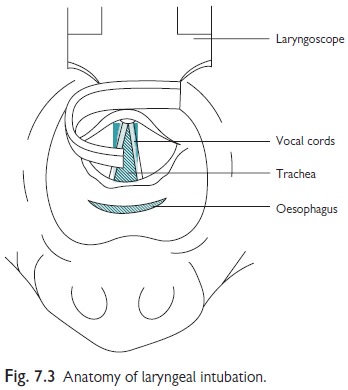
Vertically
lift up the whole blade, thereby exposing the vocal cords (see Fig. 7.3). Apply
cricoid pressure with the little finger of the left hand to see the vocal
cords. Perform suction if needed.
•
If the
vocal cords cannot be seen after 30s do not try to attempt blind intubation.
Abandon the attempt, maintain patent airway, and perform mask ventilation,
before trying again.
•
Once
the vocal cords are seen, insert the ETT between the vocal cords. If difficult,
or performing nasal intubation, use the Magill forceps with the right hand to
advance the ETT tip.
•
If
using a straight tube, the ETT should be advanced until the thick black line at
the tip is level with the vocal cords. If using a Cole ETT, advance it until
the shoulder just reaches the vocal cords.
•
If
using a cuffed tube advance until the cuff is just below the vocal cords and no
further. Then inflate the cuff with air using a syringe.
•
Once
intubation is successful, connect tubing and ventilate.
•
Visually
check chest movement and auscultate over each lung to ensure appropriate and
equal bilateral air entry.
•
If
this procedure is successful, SpO2 and heart rate should improve.
•
Fix
ETT in place appropriately following local institutional guidelines.
•
Perform
a CXR to confirm position of ETT, which should ideally be 1–2cm above the
carina, depending on the childs’ size.
•
Causes
of failure to intubate include: poor visualization of vocal cords due to over
extension of neck or advancement of laryngoscope too far into the oesophagus;
spasm of vocal cords (wait, as almost certainly vocal cords will open
eventually—do not attempt to force ETT through as this may cause damage);
anatomical abnormalities, e.g. laryngeal atresia; vocal cord oedema.
•
Conditions
that may give an impression of failed intubation (little or no chest movement
on ventilation after intubation) include: thoracic pathology (e.g. tension
pneumothorax, diaphragmatic hernia); intubation of the right main bronchus
(detected by unequal air entry); and particulate obstruction of airway or ETT.
Related Topics