Chapter: Medical Surgical Nursing: Management of Patients With Complications From Heart Disease
Nursing Process: The Patient With Heart Failure
NURSING
PROCESS:THE PATIENT WITH HEART FAILURE
Assessment
The
nursing assessment for the patient with HF focuses on ob-serving for
effectiveness of therapy and for the patient’s ability to understand and
implement self-management strategies. Signs and symptoms of pulmonary and
systemic fluid overload are recorded and reported immediately so that
adjustments can be made in ther-apy. The nurse also explores the patient’s
emotional response to the diagnosis of HF, a chronic illness.
HEALTH HISTORY
The
nurse explores sleep disturbances, particularly sleep suddenly in-terrupted by
shortness of breath. The nurse also asks about the num-ber of pillows needed
for sleep (an indication of orthopnea), activities of daily living, and the
activities that cause shortness of breath. The nurse also explores the
patient’s understanding of HF, the self-management strategies, and the desire
to adhere to those strate-gies. The nurse helps patients to identify things
that they have lost because of the diagnosis, their emotional response to that
loss, and successful coping skills that they have used previously. Family and
significant others are often included in these discussions.
PHYSICAL EXAMINATION
The
lungs are auscultated to detect crackles and wheezes or their absence.
Crackles, which are produced by the sudden opening of small airways and alveoli
that have adhered together by edema and exudate, may be heard at the end of
inspiration and are not cleared with coughing. They may also sound like
gurgling that may clear with coughing or suctioning. The rate and depth of
res-pirations are also documented.
The
heart is auscultated for an S3 heart sound, a sign that the heart is beginning to
fail and that increased blood volume re-mains in the ventricle with each beat.
HR and rhythm are also documented. Rapid rates indicate that SV has decreased
and that the ventricle has less time to fill, producing some blood stagna-tion
in the atria and eventually in the pulmonary bed.
JVD is
also assessed; distention greater than 3 cm above the sternal angle is
considered abnormal. This is an estimate, not a precise measurement, of central
venous pressure.
Sensorium
and level of consciousness must be evaluated. As the volume of blood ejected by
the heart decreases, so does the amount of oxygen transported to the brain.
The
nurse makes sure that dependent parts of the patient’s body are assessed for
perfusion and edema. With significant de-creases in SV, there is a decrease in
perfusion to the periphery, causing the skin to feel cool and appear pale or
cyanotic. If the patient is sitting upright, the feet and lower legs are
examined for edema; if the patient is supine in bed, the sacrum and back are
assessed for edema. Fingers and hands may also become edematous.
In
extreme cases of HF, the patient may develop periorbital edema, in which the
eyelids may swell shut.
The
liver is assessed for hepatojugular reflux. The patient is asked to breathe
normally while manual pressure is applied over the right upper quadrant of the
abdomen for 30 to 60 seconds. If neck vein distention increases more than 1 cm,
the test finding is positive for increased venous pressure.
If the
patient is hospitalized, the nurse measures output care-fully to establish a
baseline against which to measure the effective-ness of diuretic therapy.
Intake and output records are rigorously maintained. It is important to know
whether the patient has ingested more fluid than he or she has excreted
(positive fluid balance), which is then correlated with a gain in weight. The
pa-tient must be monitored for oliguria (diminished urine output, <400 mL/24
hours) or anuria (urine output
<50 mL/24 hours).
The
patient is weighed daily in the hospital or at home, at the same time of day,
with the same type of clothing, and on the same scale. If there is a
significant change in weight (ie, 2- to 3-lb increase in a day or 5-lb increase
in a week), the patient is instructed to notify the physician or adjust the
medications (eg, increase the diuretic dose).
Diagnosis
NURSING DIAGNOSES
• Activity intolerance (or risk for activity intolerance) related to imbalance between oxygen supply and demand because of decreased CO
• Excess fluid volume related to excess fluid or sodium intake and retention of fluid because of HF and its medical therapy
• Anxiety related to breathlessness and restlessness from in-adequate oxygenation
• Powerlessness related to inability to perform role responsi-bilities because of chronic illness and hospitalizations
• Noncompliance related to lack of knowledge
COLLABORATIVE PROBLEMS/POTENTIAL COMPLICATIONS
Based on the assessment data, potential complications that may develop include the following:
• Cardiogenic shock
• Dysrhythmias
• Thromboembolism
• Pericardial effusion and cardiac tamponade
Planning and Goals
Major
goals for the patient may include promoting activity and reducing fatigue,
relieving fluid overload symptoms, decreasing the incidence of anxiety or
increasing the patient’s ability to manage anxiety, teaching the patient about
the self-care pro-gram, and encouraging the patient to verbalize his or her
ability to make decisions and influence outcomes.
Nursing Interventions
PROMOTING ACTIVITY TOLERANCE
Although
prolonged bed rest and even short periods of recumbency promote diuresis by
improving renal perfusion, they also promote decreased activity tolerance.
Prolonged bed rest, which may be self-imposed, should be avoided because of the
deconditioning effects and hazards, such as pressure ulcers (especially in
edematous pa-tients), phlebothrombosis, and pulmonary embolism. An acute event
that causes severe symptoms or that requires hospitaliza-tion indicates the
need for initial bed rest. Otherwise, a total of 30 minutes of physical
activity three to five times each week should be encouraged (Georgiou et al.,
2001). The nurse and patient can collaborate to develop a schedule that
promotes pacing and prior-itization of activities. The schedule should
alternate activities with periods of rest and avoid having two significant
energy-consuming activities occur on the same day or in immediate succession.
• Begin with a few minutes of warm-up activities.
• Avoid performing physical activities outside in extreme hot, cold, or humid weather.
• Ensure that you are able to talk during the physical activity; if you are unable to do so, decrease the intensity of activity.
• Wait 2 hours after eating a meal before performing the physical activity.
• Stop the activity if severe shortness of breath, pain, or dizzi-ness develops.
• End with cool-down activities and a cool-down period.
Because
some patients may be severely debilitated, they may need to perform physical
activities only 3 to 5 minutes at a time, one to four times per day. The
patient then should be advised to increase the duration of the activity, then
the frequency, before increasing the intensity of the activity (Meyer, 2001).
Barriers
to performing an activity are identified, and methods of adjusting an activity
to ensure pacing but still accomplish the task are discussed. For example,
objects that need to be taken up-stairs can be put in a basket at the bottom of
the stairs through-out the day. At the end of the day, the person can carry the
objects up the stairs all at once. Likewise, the person can carry cleaning
supplies around in a basket or backpack rather than walk back and forth to
obtain the items. Vegetables can be chopped or peeled while sitting at the kitchen
table rather than standing at the kitchen counter. Small, frequent meals
decrease the amount of energy needed for digestion while providing adequate
nutri-tion. The nurse helps the patient to identify peak and low peri-ods of
energy and plan energy-consuming activities for peak periods. For example, the
person may prepare the meals for the entire day in the morning. Pacing and
prioritizing activities help maintain the patient’s energy to allow
participation in regular physical activity .
The
patient’s response to activities needs to be monitored. If the patient is
hospitalized, vital signs and oxygen saturation level are monitored before,
during, and immediately after an ac-tivity to identify whether they are within
the desired range. Heart rate should return to baseline within 3 minutes. If
the pa-tient is at home, the degree of fatigue felt after the activity can be
used as assessment of the response. If the patient tolerates the activity,
short-term and long-term goals can be developed to gradually increase the
intensity, duration, and frequency of ac-tivity. Referral to a cardiac
rehabilitation program may be needed, especially for HF patients with recent
myocardial infarction, recent open-heart surgery, or increased anxiety. A
supervised pro-gram may also benefit those who need the structured
environ-ment, significant educational support, regular encouragement, and
interpersonal contact.
MANAGING FLUID VOLUME
Patients
with severe HF may receive intravenous diuretic therapy, but patients with less
severe symptoms may receive oral diuretic medication (see Table 30-4 for a
summary of common diuretics). Oral diuretics should be administered early in
the morning so that diuresis does not interfere with the patient’s nighttime
rest. Discussing the timing of medication administration is especially
important for patients, such as elderly people, who may have uri-nary urgency
or incontinence. A single dose of a diuretic may cause the patient to excrete a
large volume of fluid shortly after administration.
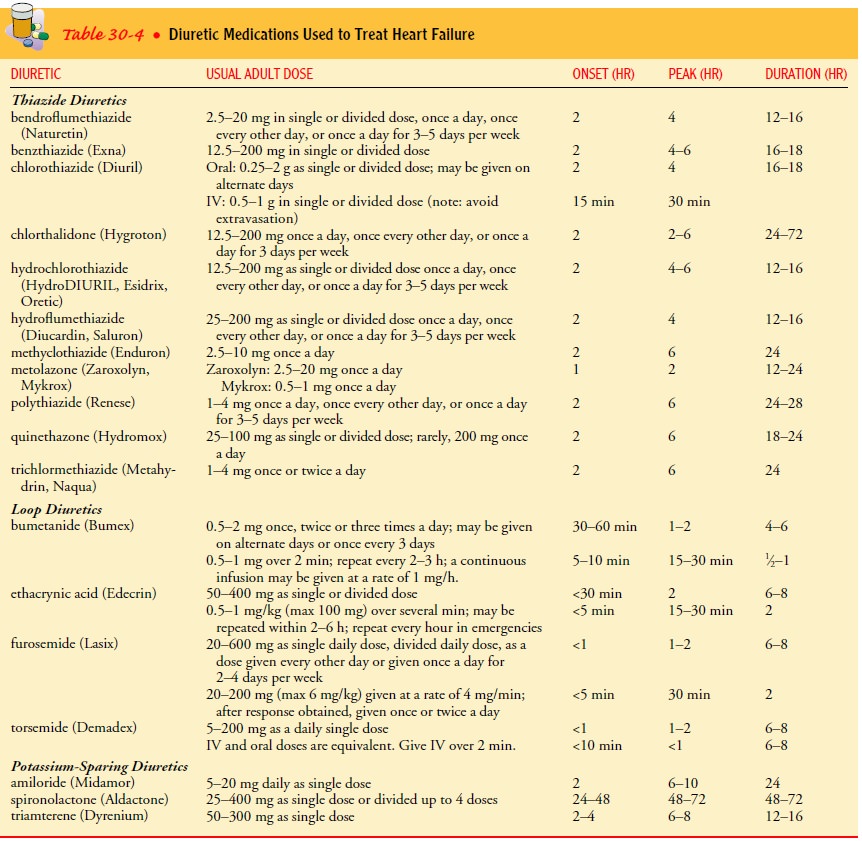
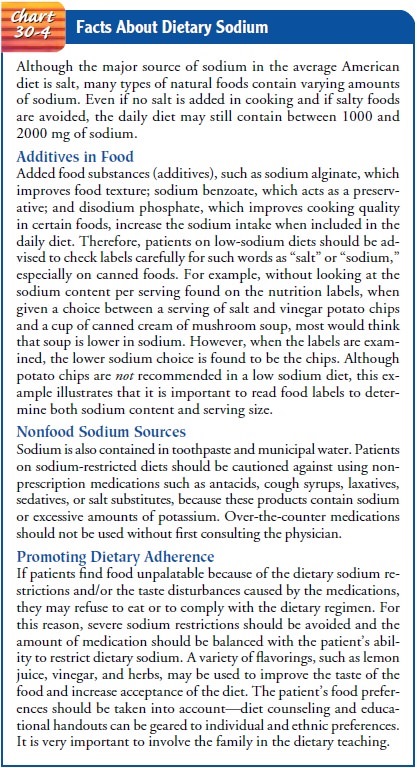
The nurse monitors the patient’s fluid status closely— auscultating the lungs, monitoring daily body weights, and as-sisting the patient to adhere to a low-sodium diet by reading food labels and avoiding high-sodium foods such as canned, processed, and convenience foods (Chart 30-4). If the diet includes fluid re-striction, the nurse can assist the patient to plan the fluid in-take throughout the day while respecting the patient’s dietary preferences.
If the patient is receiving intravenous fluids, the amount
of fluid needs to be monitored closely, and the physi-cian or pharmacist can be
consulted about the possibility of maximizing the amount of medication in the
same amount of intravenous fluid (eg, double-concentrating to decrease the
fluid volume administered).
The
nurse positions the patient or teaches the patient how to assume a position
that shifts fluid away from the heart. The num-ber of pillows may be increased,
the head of the bed may be elevated (20- to 30-cm [8- to 10-inch] blocks may be
used), or the patient may sit in a comfortable armchair. In this position, the
venous return to the heart (preload) is reduced, pulmonary con-gestion is
alleviated, and impingement of the liver on the di-aphragm is minimized. The
lower arms are supported with pillows to eliminate the fatigue caused by the
constant pull of their weight on the shoulder muscles.
The
patient who can breathe only in the upright position may sit on the side of the
bed with the feet supported on a chair, the head and arms resting on an overbed
table, and the lumbosacral spine supported by a pillow. If pulmonary congestion
is present, positioning the patient in an armchair is advantageous, because
this position favors the shift of fluid away from the lungs.
Because
decreased circulation in edematous areas increases the risk of skin injury, the
nurse assesses for skin breakdown and in-stitutes preventive measures. Frequent
changes of position, posi-tioning to avoid pressure, the use of elastic
compression stockings, and leg exercises may help to prevent skin injury.
CONTROLLING ANXIETY
Because
patients in HF have difficulty maintaining adequate oxy-genation, they are
likely to be restless and anxious and feel over-whelmed by breathlessness.
These symptoms tend to intensify at night. Emotional stress stimulates the
sympathetic nervous sys-tem, which causes vasoconstriction, elevated arterial
pressure, and increased heart rate. This sympathetic response increases the
amount of work that the heart has to do. By decreasing anxiety, the patient’s
cardiac work also is decreased. Oxygen may be ad-ministered during an acute
event to diminish the work of breath-ing and to increase the patient’s comfort.
When
the patient exhibits anxiety, the nurse takes steps to promote physical comfort
and psychological support. In many cases, a family member’s presence provides
reassurance. To help decrease the patient’s anxiety, the nurse should speak in
a slow, calm, and confident manner and maintain eye contact. When necessary,
the nurse should also state specific, brief directions for an activity.
After
the patient is comfortable, the nurse can begin teaching ways to control
anxiety and to avoid anxiety-provoking situa-tions. The nurse explains how to
use relaxation techniques and assists the patient to identify factors that
contribute to anxiety. Lack of sleep may increase anxiety, which may prevent
adequate rest. Other contributing factors may include misinformation, lack of
information, or poor nutritional status. Promoting phys-ical comfort, providing
accurate information, and teaching the patient to perform relaxation techniques
and to avoid anxiety-triggering situations may relax the patient.
In
cases of confusion and anxiety reactions that affect the pa-tient’s safety, the
use of restraints should be avoided. Restraints are likely to be resisted, and
resistance inevitably increases the car-diac workload. The patient who insists
on getting out of bed at night can be seated comfortably in an armchair. As
cerebral and systemic circulation improves, the degree of anxiety decreases,
and the quality of sleep improves.
MINIMIZING POWERLESSNESS
Patients
need to recognize that they are not helpless and that they can influence the
direction of their lives and the outcomes of treatment. The nurse assesses for
factors contributing to a sense of powerlessness and intervenes accordingly.
Contributing factors may include lack of knowledge and lack of opportunities to
make decisions, particularly if health care providers and family mem-bers behave
in maternalistic or paternalistic ways. If the patient is hospitalized,
hospital policies may promote standardization and limit the patient’s ability
to make decisions (eg, what time to have meals, take medications, prepare for
bed).
Taking
time to listen actively to patients often encourages them to express their
concerns and ask questions. Other strategies in-clude providing the patient
with decision-making opportunities, such as when activities are to occur or
where objects are to be placed, and increasing the frequency and significance
of those op-portunities over time; providing encouragement while identifying
the patient’s progress; and assisting the patient to differentiate be-tween
factors that can be controlled and those that cannot. In some cases, the nurse
may want to review hospital policies and standards that tend to promote
powerlessness and advocate for their elimi-nation or change (eg, limited
visiting hours, prohibition of food from home, required wearing of hospital
gowns).
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
The
nurse provides patient education and involves the patient in implementing the
therapeutic regimen to promote understand-ing and adherence to the plan. When
the patient understands or believes that the diagnosis of HF can be
successfully managed with lifestyle changes and medications, recurrences of
acute HF lessen, unnecessary hospitalizations decrease, and life expectancy
increases. Patients and their families need to be taught to follow the medication
regimen as prescribed, maintain a low-sodium diet, perform and record daily
weights, engage in routine physi-cal activity, and recognize symptoms that
indicate worsening HF. Although noncompliance is not well understood,
interventions that may promote adherence include teaching to ensure accurate
understanding. A summary of teaching points for the patient with HF is
presented in Chart 30-5.

The patient and family members are supported and encouraged to ask questions so that information can be clarified and under-standing enhanced. The nurse should be aware of cultural factors and adapt the teaching plan accordingly. Patients and their fami-lies need to be informed that the progression of the disease is in-fluenced in part by choices made about health care and the decisions about following the treatment plan. They also need to be informed that health care providers are there to assist them in reaching their health care goals. Patients and family members need to make the decisions about the treatment plan, but they also need to understand the possible outcomes of those decisions. The treat-ment plan then will be based on what the patient wants, not just what the physician or other health care team members think is needed. Ultimately, the nurse needs to convey that monitoring symptoms and daily weights, restricting sodium intake, avoiding excess fluids, preventing infection with influenza and pneumococ-cal immunizations, avoiding noxious agents (eg, alcohol, tobacco), and participating in regular exercise all aid in preventing exacerba-tions of HF.
Continuing Care
Depending
on the patient’s physical status and the availability of family assistance, a
home care referral may be indicated for a patient who has been hospitalized.
Elderly patients and those who have long-standing heart disease with
compromised phys-ical stamina often require assistance with the transition to
home after hospitalization for an acute episode of HF. It is important for the
home care nurse to assess the physical environment of the home. Suggestions for
adapting the home environment to meet the patient’s activity limitations are
important. If stairs are the concern, the patient can plan the day’s activities
so that stair climbing is minimized; for some patients, a temporary bedroom may
be set up on the main level of the home. The home care nurse collaborates with
the patient and family to maximize the benefits of these changes.
The
home care nurse also reinforces and clarifies information about dietary changes
and fluid restrictions, the need to monitor symptoms and daily body weights,
and the importance of obtain-ing follow-up health care. Assistance may be given
in scheduling and keeping appointments as well. The patient is encouraged to
gradually increase his or her self-care and responsibility for ac-complishing
the therapeutic regimen.
Evaluation
EXPECTED PATIENT OUTCOMES
Expected
patient outcomes may include:
1) Demonstrates tolerance
for increased activity
a) Describes adaptive
methods for usual activities
b) Stops any activity that
causes symptoms of intolerance
c) Maintains vital signs
(pulse, blood pressure, respira-tory rate, and pulse oximetry) within the
targeted range
d) Identifies factors that
contribute to activity intolerance and takes actions to avoid them
e) Establishes priorities
for activities
f) Schedules activities to
conserve energy and to reduce fatigue and dyspnea
2) Maintains fluid balance
a) Exhibits decreased
peripheral and sacral edema
b) Demonstrates methods for
preventing edema
3) Is less anxious
a) Avoids situations that
produce stress
b) Sleeps comfortably at
night
c) Reports decreased stress
and anxiety
4) Makes decisions
regarding care and treatment
a) States ability to
influence outcomes
5) Adheres to self-care
regimen
a) Performs and records
daily weights
b) Ensures dietary intake
includes no more than 2 to 3 g of sodium per day
c) Takes medications as
prescribed
d) Reports any unusual
symptoms or side effects
Related Topics