Chapter: Medical Surgical Nursing: Management of Patients With Neurologic Infections, Autoimmune Disorders, and Neuropathies
Nursing Process: The Patient With Guillain-Barré Syndrome
NURSING PROCESS: THE PATIENT WITH GUILLAIN-BARRÉ
SYNDROME
Assessment
Ongoing assessment for
disease progression is critical. The pa-tient is monitored for life-threatening
complications (respiratory failure, cardiac dysrhythmias, DVTs) so that
appropriate inter-ventions can be initiated. Because of the threat to the
patient in this sudden, potentially life-threatening disease, the nurse must
assess the patient’s and family’s ability to cope and their use of appropriate
coping strategies.
Diagnosis
NURSING DIAGNOSES
Based on the assessment data, the patient’s major nursing
diag-noses may include the following:
·
Ineffective breathing pattern
and impaired gas exchange re-lated to rapidly progressive weakness and
impending respi-ratory failure
·
Impaired physical mobility
related to paralysis
·
Imbalanced nutrition, less
than body requirements, related to inability to swallow
·
Impaired verbal communication
related to cranial nerve dysfunction
·
Fear and anxiety related to
loss of control and paralysis
COLLABORATIVE PROBLEMS/POTENTIAL COMPLICATIONS
Based on the assessment
data, potential complications that may develop include the following:
·
Respiratory failure
·
Autonomic dysfunction
Planning and Goals
The major goals for the patient may include improved
respiratory function, increased mobility, improved nutritional status,
effec-tive communication, decreased fear and anxiety, and absence of
complications.
Nursing Interventions
MAINTAINING RESPIRATORY FUNCTION
Respiratory function can
be maximized with incentive spirome-try and chest physiotherapy. Monitoring for
changes in vital ca-pacity and negative inspiratory force are key to early
intervention for neuromuscular respiratory failure. Mechanical ventilation is
required if the vital capacity falls, making spontaneous breathing impossible
and tissue oxygenation inadequate.
Parameters for determining the appropriate time to begin
me-chanical ventilation include a vital capacity of 12 to 15 mL/kg, downward
vital capacity trend over 4 to 6 hours, and an inability to clear secretions
(Bella & Chad, 1999). The potential need for mechanical ventilation should
be discussed with the patient and family on admission to provide time for
psychological prepara-tion and decision-making. Intubation and mechanical
ventilation will result in less anxiety if it is initiated on a nonemergent
basis to a well-informed patient. The patient may require mechanical
ventilation for a long period..
Bulbar weakness that impairs the ability to swallow and
clear secretions is another factor in the development of respiratory fail-ure
in the patient with Guillain-Barré. Suctioning may be needed to maintain a
clear airway.
The nurse assesses the blood pressure and heart rate
frequently to identify autonomic dysfunction so that interventions can be
initiated quickly if needed. Medications are administered or a temporary
pacemaker is placed for clinically significant brady-cardia (Winer, 2002).
ENHANCING PHYSICAL MOBILITY
Nursing interventions to enhance physical mobility and
prevent the complications of immobility are key to the function and sur-vival
of these patients. The paralyzed extremities are supported in functional
positions, and passive range-of-motion exercises are performed at least twice
daily.
DVT and pulmonary
embolism are threats to the paralyzed patient. Nursing interventions are aimed
at preventing DVT. Range-of-motion exercises, altering positioning,
anticoagulation, thigh-high elastic compression stockings or sequential
com-pression boots, and adequate hydration will decrease the risk for DVT.
Padding may be placed over bony prominences such as the
el-bows and heels to reduce the risk for pressure ulcers. The need for
consistent position changes every 2 hours cannot be overempha-sized. The nurse
evaluates laboratory test results that may indi-cate malnutrition or
dehydration, both of which increase the risk for pressure ulcers. Collaboration
with the physician and dietitian will result in a plan to meet the patient’s
nutritional and hydra-tion needs.
PROVIDING ADEQUATE NUTRITION
Paralytic ileus may
result from insufficient parasympathetic ac-tivity. In this event, the nurse
administers IV fluids and parenteral nutrition as prescribed and monitors for
the return of bowel sounds. If the patient cannot swallow due to bulbar paralysis (immobility of
muscles), a gastrostomy tube may be placed to ad-minister nutrients. The nurse
carefully assesses the return of the gag reflex and bowel sounds before
resuming oral nutrition.
IMPROVING COMMUNICATION
Because of paralysis and
ventilator management, the patient can-not talk, laugh, or cry and thus has no
method for communicating needs or expressing emotion. Establishing some form of
com-munication with picture cards or an eye blink system will provide a means
of communication. Collaboration with the speech ther-apist may be helpful in
developing a communication mechanism that is most effective for a specific
patient.
DECREASING FEAR AND ANXIETY
The patient and family are faced with a sudden,
potentially life-threatening disease, and anxiety and fear are constant themes
for them. The impact of disease on the family will depend on the patient’s age
and role within the family. Referral to a support group may provide information
and support to the patient and family.
The family may feel helpless in caring for the patient.
Me-chanical ventilation and monitoring devices may frighten and intimidate
them. Family members often want to participate in physical care; with
instruction and support by the nurse, they should be allowed to do so.
In addition to fear, the
patient may experience isolation, lone-liness, and lack of control. Nursing
interventions that increase the patient’s sense of control include providing
information about the condition, emphasizing a positive appraisal of coping
resources, and teaching relaxation exercises and distraction techniques. The
positive attitude and atmosphere of the multidisciplinary team are important to
promote a sense of well-being.
Diversional activities
are encouraged to decrease loneliness and isolation. Encouraging visitors,
engaging visitors or volun-teers to read to the patient, listening to music or
books on tape, and watching television are ways to alleviate the patient’s
sense of isolation.
MONITORING AND MANAGING POTENTIAL COMPLICATIONS
Thorough assessment of
respiratory function at regular intervals is essential because respiratory
insufficiency and subsequent failure due to weakness or paralysis of the
intercostal muscles and di-aphragm may develop quickly. Respiratory failure is
the major cause of mortality, which is reported to be as high as 10% to 20%.
Vital capacity is monitored frequently and at regular intervals in addition to
respiratory rate and the quality of respirations, so that respiratory
insufficiency can be anticipated. Decreasing vital ca-pacity associated with
weakness of the muscles used in swallowing, which causes difficulty in both
coughing and swallowing, indi-cates impending respiratory failure. Signs and
symptoms include breathlessness while speaking, shallow and irregular
breathing, use of accessory muscles, tachycardia, and changes in respiratory
pattern.
Parameters for determining the onset of respiratory
failure are established on admission, allowing intubation and the initiation of
mechanical ventilation on a nonemergent basis. This also al-lows the patient to
be prepared for the procedure in a controlled manner, which reduces anxiety and
complications.
Other complications include cardiac dysrhythmias, which
ne-cessitate ECG monitoring, transient hypertension, orthostatic hypotension,
DVT, pulmonary embolism, urinary retention, and other threats to any
immobilized and paralyzed patient. These re-quire monitoring and attention to
prevent them and prompt treatment if indicated.
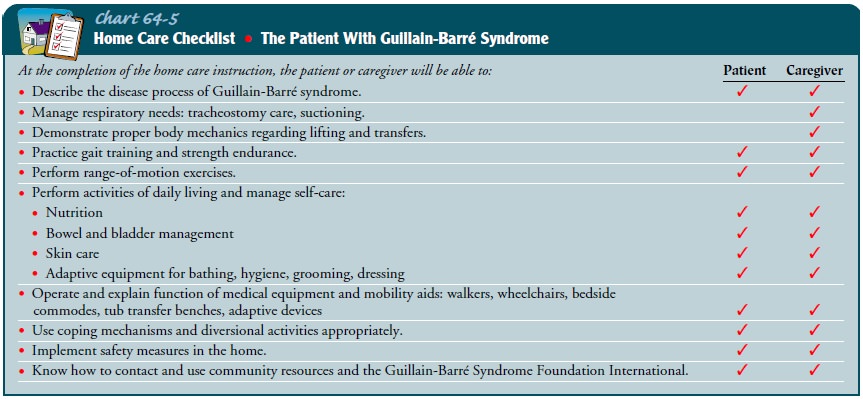
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care
Patients with
Guillain-Barré syndrome and their families are usu-ally frightened by the
sudden onset of life-threatening symptoms and their severity. Therefore,
teaching the patient and family about the disorder and its generally favorable
prognosis is impor-tant (Chart 64-5). During the acute phase of the illness,
the patient and family are instructed about strategies they can implement to
minimize the effects of immobility and other complications. As function begins
to return, family members and other home care providers are instructed about
care of the patient and their role in the rehabilitation process. Preparation
for discharge is an inter-disciplinary effort requiring family or caregiver
education by all team members, including the nurse, physician, occupational and
physical therapists, speech therapist, and respiratory therapist.
Continuing Care
Most patients with Guillain-Barré syndrome experience
complete recovery. Patients who have experienced total or prolonged paral-ysis
require intensive rehabilitation; the extent depends on the pa-tient’s needs.
Approaches include a comprehensive inpatient program if deficits are
significant, an outpatient program if the patient can travel by car, or a home program
of physical and oc-cupational therapy. The recovery phase may be long and will
re-quire patience as well as involvement on the part of the patient and family.
During acute care the focus is on obvious needs, issues,
and deficits. The nurse needs to remind or instruct patients and fam-ily
members of the need for continuing health promotion and screening practices
following this initial phase of care.
Evaluation
EXPECTED PATIENT OUTCOMES
Expected patient outcomes may include:
1) Maintains
effective respirations and airway clearance
a) Has
normal breath sounds on auscultation
b) Demonstrates
gradual improvement in respiratory function
2) Shows
increasing mobility
a) Regains
use of extremities
b) Participates
in rehabilitation program
c) Demonstrates
no contractures and minimal muscle atrophy
3) Receives
adequate nutrition and hydration
a) Consumes
diet adequate to meet nutritional needs
b) Swallows
without aspiration
4) Demonstrates
recovery of speech
a) Can
communicate needs through alternative strategies
b) Practices
exercises recommended by the speech therapist
5) Shows
lessening fear and anxiety
6) Absence
of complications
a) Breathes
spontaneously
b) Has
vital capacity within normal range
c) Exhibits
normal arterial blood gases and oximetry
Related Topics