Chapter: Medical Surgical Nursing: Pain Management
Neurologic and Neurosurgical Approaches to Pain Management
Neurologic and Neurosurgical Approaches to Pain
Management
In some situations, especially with long-term and severe in-tractable
pain, usual pharmacologic and nonpharmacologic methods of pain relief are
ineffective. In those situations, neuro-logic and neurosurgical approaches to
pain management may be considered. Intractable pain refers to pain that cannot
be relieved satisfactorily by the usual approaches, including medications. Such
pain usually is the result of malignancy (especially of the cervix, bladder,
prostate, and lower bowel), but it may occur in other conditions, such as
postherpetic neuralgia, trigeminal neu-ralgia, spinal cord arachnoiditis, and
uncontrollable ischemia and other forms of tissue destruction.
Neurologic and
neurosurgical methods available for pain relief include (1) stimulation
procedures (intermittent electrical stimulation of a tract or center to inhibit
the transmission of pain impulses), (2) administration of intraspinal opioids
(see pre-vious discussion), and (3) interruption of the tracts conducting the
pain impulse from the periphery to cerebral integration cen-ters. The latter
are destructive or ablative procedures, and their effects are permanent.
Ablative procedures are used when other methods of pain relief have failed.
STIMULATION PROCEDURES
Electrical stimulation, or neuromodulation, is a method of sup-pressing
pain by applying controlled low-voltage electrical pulses to the different
parts of the nervous system. Electrical stimulation is thought to relieve pain
by blocking painful stimuli (the gate control theory). This pain-modulating
technique is administered by many modes. TENS and dorsal spinal cord
stimulation are the most common types of electrical stimulation used. (See
previous discussion of TENS.) In addition, there are also brain-stimulating
techniques in which electrodes are implanted in the periventric-ular area of
the posterior third ventricle, allowing the patient to stimulate this area to
produce analgesia.
In spinal cord stimulation, a technique used for the relief of chronic,
intractable pain, ischemic pain, and pain from angina, a surgically implanted
device allows the patient to apply pulsed electrical stimulation to the dorsal
aspect of the spinal cord to block pain impulses (Linderoth & Meyerson,
2002). (The largest accumulation of afferent fibers is found in the dorsal
column of the spinal cord.) The dorsal column stimulation unit consists of a
radiofrequency stimulation transmitter, a transmitter antenna, a radiofrequency
receiver, and a stimulation electrode. The battery-powered transmitter and
antenna are worn externally; the re-ceiver and electrode are implanted. A
laminectomy is performed above the highest level of pain input, and the
electrode is placed in the epidural space over the posterior column of the
spinal cord. (The placement of the stimulating systems varies.) A subcutaneous
pocket is constructed over the clavicular area or some other site for placement
of the receiver. The two are connected by a sub-cutaneous tunnel. Careful
patient selection is necessary, and not all patients receive total pain relief.
Deep brain stimulation is performed for special pain prob-lems when the
patient does not respond to the usual techniques of pain control. With the
patient under local anesthesia, electrodes are introduced through a burr hole
in the skull and inserted into a selected site in the brain, depending on the
location or type of pain. After the effectiveness of stimulation is confirmed,
the im-planted electrode is connected to a radiofrequency device or
pulse-generator system operated by external telemetry. It is used in
neuropathic pain that may occur with damage or injury that oc-curred following
stroke, brain or spinal cord injuries, or phantom limb pain. Use of deep brain
stimulation has decreased and may be related to improved pain control and
intraspinal therapies (Rezai & Lozano, 2002).
Interruption of Pain Pathways
As described above, stimulation of a peripheral nerve, the spinal cord,
or the deep brain using minute amounts of electricity and a stimulating device
is used if all other pharmacologic and non-pharmacologic treatments fail to
provide adequate relief. These treatments are reversible. If they need to be
discontinued, the ner-vous system continues to function. Treatments that
interrupt the pain pathways, however, are permanent.
Pain-conducting fibers
can be interrupted at any point from their origin to the cerebral cortex. Some
part of the nervous system is destroyed, resulting in varying amounts of
neurologic deficit and incapacity. In time, pain usually returns as a result of
either regeneration of axonal fibers or the development of alter-native pain
pathways.
Destructive procedures used to interrupt the transmission of pain
include cordotomy and rhizotomy. These procedures are of-fered if the patient
is thought to be near the end of life and will have an improved quality of life
as an outcome (Linderoth & Meyerson, 2002). Often these procedures can
provide pain relief for the duration of a patient’s life. The use of other
methods to interrupt pain transmission is waning since the use of intraspinal
therapies and newer pain management treatments are available.
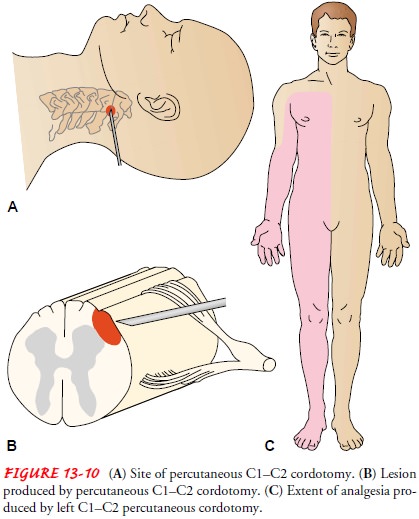
CORDOTOMY
A cordotomy is the
division of certain tracts of the spinal cord (Fig. 13-10). It may be performed
percutaneously, by the open method after laminectomy, or by other techniques.
Cordotomy is performed to interrupt the transmission of pain (Hodge &
Christensen, 2002). Care must be taken to destroy only the sen-sation of pain,
leaving motor functions intact.
RHIZOTOMY
Sensory nerve roots are
destroyed where they enter the spinal cord. A lesion is made in the dorsal root
to destroy neuronal dys-function and reduce nociceptive input. With the advent
of micro-surgical techniques, the complications are few, with mild sensory
deficits and mild weakness (Fig. 13-11).
Nursing Interventions
With each of these procedures, patients are provided with written and verbal instructions about their expected effect on pain and on possible untoward consequences.
The patient is monitored for specific effects of each method of pain intervention, both positive and
negative. The specific nursing care of patients who undergo neurologic and
neurosurgical procedures for the relief of chronic pain depends on the type of
procedure performed, its effectiveness in relieving the pain, and the changes
in neurologic function that accompany the procedure. After the procedure, the
patient’s pain level and neurologic function are assessed. Other nursing
inter-ventions that may be indicated include positioning, turning and skin
care, bowel and bladder management, and interventions to promote patient
safety. Pain management remains an important aspect of nursing care with each
of these procedures.
ALTERNATIVE THERAPIES
People suffering chronic, debilitating pain are often desperate. Often
they will try anything, recommended by anyone, at any price. Information about
an array of potential therapies can be found on the Internet and in the
self-help section of the book-store. Therapies specifically recommended for
pain from these sources include but are not limited to chelation, therapeutic
touch, music therapy, herbal therapy, reflexology, magnetic ther-apy,
electrotherapy, polarity therapy, acupressure, emu oil, pectin therapy,
aromatherapy, homeopathy, and macrobiotic dieting. Many of these “therapies”
(with the exception of macrobiotic di-eting) are probably not harmful. However,
they have yet to be proven effective by the standards used to evaluate the
effective-ness of medical and nursing interventions. The National Institutes of
Health has established an office to examine the effectiveness of alternative
therapies.
Despite the lack of
scientific evidence that these therapies are effective, a patient may find any
one of them helpful via theplacebo response. It is important when caring for a
patient who is using or considering using untested therapies (often referred to
as alternative therapies) not to diminish the patient’s hope and potential
placebo response. This must be weighed against the professional nurse’s
responsibility to protect the patient from costly and potentially harmful and
dangerous therapies that the patient is not in a position to evaluate
scientifically.
Problems arise when
patients do not find relief but are de-prived of conventional therapy because
the alternative therapy “should be helping,” or when patients abandon
conventional therapy for alternative therapy. In addition, few alternative
ther-apies are free. Desperate patients may risk financial ruin seeking
alternative therapies that do not work.
The nurse’s role is to
help the patient and family understand scientific research and how that differs
from anecdotal evidence. Without diminishing the placebo effects the patient
may receive, the nurse encourages the patient to assess the effectiveness of
the therapy continually using standard pain assessment techniques. In addition,
the nurse encourages the patient using alternative therapies to combine them
with conventional therapies and to discuss this use with the physician.
Related Topics